INDICATIONS/CONTRAINDICATIONS
Dysphagia, food regurgitation, and chest pain are the presentation symptoms recorded in patients with epiphrenic diverticula. The main reason for suggesting a surgical approach is the regular and progressing discomfort resulting from the underlying motor dysfunction. The condition is usually present in high-strung individuals and proper physiologic and psychological investigation is indicated. Up to one-third of all patients with an epiphrenic diverticulum are asymptomatic. These patients can be treated conservatively but kept under observation as 20% will show an increase in size of the diverticulum. Inflammation, bleeding, fistulisation, and cancer formation are complications that may result from an intrathoracic epiphrenic diverticulum.
| Indications | • Severity of symptoms associated with the diverticulum • Complications related to the diverticulum • Progression in size of the diverticulum |
| Contraindications | • Asymptomatic patient • Associated medical condition |
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Symptom evaluation is important as symptom frequency, duration, and severity represent the main indicators to proceed with surgery.
Radiologic evaluation of the esophagus is essential to document the anatomy and exact location of the diverticulum. Epiphrenic diverticula are found on the distal 10 cm of the esophagus above the cardia (Fig. 16.1). They usually develop on the right posterolateral side of the esophageal wall and are frequently associated with a small sliding hiatal hernia.
Manometric evaluation of esophageal function is essential as a majority of the patients will be documented with a primary idiopathic motor disorder of the spastic or achalasic variety. Dysfunction of the lower esophageal sphincter (LES) may be recorded intermittently but is still a significant abnormality that probably plays a major role in the functional obstruction of the distal esophagus and the eventual appearance of hyper pressures and diverticular herniation through the esophageal wall. Endoscopy is essential to document location and orientation of the diverticulum but mostly to rule out associated benign or malignant esophageal lesions.
| Essential evaluation | • Symptoms • Esophagram • Motor function evaluation • Endoscopy |

Figure 16.1 Barium esophagram of an epiphrenic diverticulum.
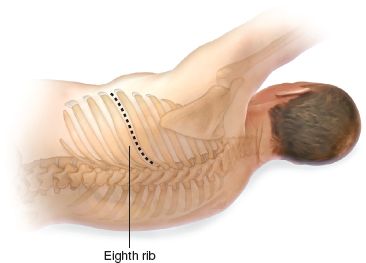
Figure 16.2 Thoracotomy above the eighth rib with the patient in the right lateral decubitus position.
 SURGERY
SURGERY
 The patient is positioned in a right lateral decubitus and a left thoracotomy above the eighth rib is completed. The rib is sectioned at the anterior and posterior extremities. Ventilation is via a double-lumen endotracheal tube, allowing the exclusion of the left lung. The inferior pulmonary ligament is divided and the lobe is retracted anteriorly and superiorly (Fig. 16.2).
The patient is positioned in a right lateral decubitus and a left thoracotomy above the eighth rib is completed. The rib is sectioned at the anterior and posterior extremities. Ventilation is via a double-lumen endotracheal tube, allowing the exclusion of the left lung. The inferior pulmonary ligament is divided and the lobe is retracted anteriorly and superiorly (Fig. 16.2).
 The mediastinal pleura is opened along the anterior border of the thoracic aorta, along the left crus of the diaphragm and then following the posterior pericardial reflection. The esophagus is mobilized progressively with careful separation of the contralateral pleura from mediastinal tissues. The integrity of both vagi nerves is protected.
The mediastinal pleura is opened along the anterior border of the thoracic aorta, along the left crus of the diaphragm and then following the posterior pericardial reflection. The esophagus is mobilized progressively with careful separation of the contralateral pleura from mediastinal tissues. The integrity of both vagi nerves is protected.
 The diverticulum location has been determined by radiologic and endoscopic investigation and Penrose drains are placed around the esophagus proximally at the level of the inferior pulmonary vein and distally at the level of the cardia (Fig. 16.3).
The diverticulum location has been determined by radiologic and endoscopic investigation and Penrose drains are placed around the esophagus proximally at the level of the inferior pulmonary vein and distally at the level of the cardia (Fig. 16.3).
 Most of the epiphrenic diverticula will look toward the right pleural cavity. Thus, the esophagus and the diverticulum are freed progressively from fascia and vascular tissues of the mediastinum. Inflammation can be significant around the diverticulum, and frequently there are adhesions between the diverticulum and surrounding structures (Fig. 16.4).
Most of the epiphrenic diverticula will look toward the right pleural cavity. Thus, the esophagus and the diverticulum are freed progressively from fascia and vascular tissues of the mediastinum. Inflammation can be significant around the diverticulum, and frequently there are adhesions between the diverticulum and surrounding structures (Fig. 16.4).
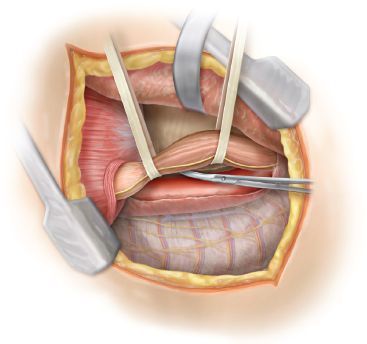
Figure 16.3 Penrose drains placed around the esophagus.
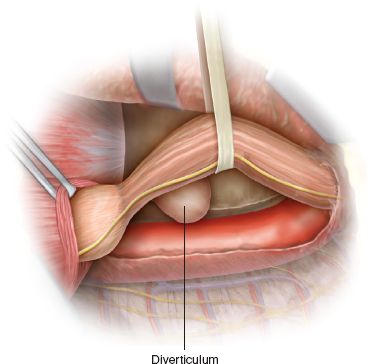
Figure 16.4 Visualization of the diverticulum after dissection from the fascia and vascular tissues of the mediastinum.
 The esophagus is freed between the inferior pulmonary vein and the diaphragm. A small hiatal hernia is frequently present, and we free all anterolateral hiatal attachments to mobilize the gastric fundus from the gastrosplenic vessels. The whole gastroesophageal junction is delivered into the chest through the hiatus.
The esophagus is freed between the inferior pulmonary vein and the diaphragm. A small hiatal hernia is frequently present, and we free all anterolateral hiatal attachments to mobilize the gastric fundus from the gastrosplenic vessels. The whole gastroesophageal junction is delivered into the chest through the hiatus.
 With the esophagus and proximal stomach completely mobilized, the esophagus and the diverticulum can be rotated easily to allow easy access for dissection of the diverticulum by the surgeon. With a Duval clamp holding the diverticulum, the fibromuscular tissue covering its neck or collar is freed progressively and the defect in the esophageal muscularis is identified (Fig. 16.5). A large, weighted bougie (50 to 56 French) is passed into the stomach and helps to free the esophageal mucosa above and below the collar of the diverticulum.
With the esophagus and proximal stomach completely mobilized, the esophagus and the diverticulum can be rotated easily to allow easy access for dissection of the diverticulum by the surgeon. With a Duval clamp holding the diverticulum, the fibromuscular tissue covering its neck or collar is freed progressively and the defect in the esophageal muscularis is identified (Fig. 16.5). A large, weighted bougie (50 to 56 French) is passed into the stomach and helps to free the esophageal mucosa above and below the collar of the diverticulum.
 The diverticulum generally develops due to the presence of a motor dysfunction of the esophagus. Depending on its position in the esophageal circumference, the diverticulum may be part of the myotomy that needs to be completed or may need to be treated separately.
The diverticulum generally develops due to the presence of a motor dysfunction of the esophagus. Depending on its position in the esophageal circumference, the diverticulum may be part of the myotomy that needs to be completed or may need to be treated separately.
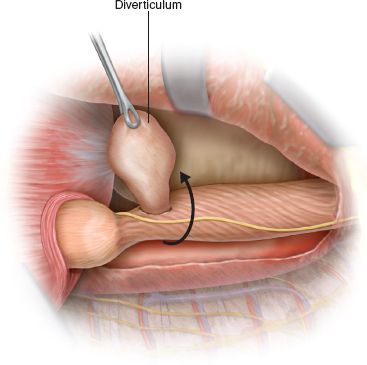
Figure 16.5 Duval clamp grasping the diverticulum, which has been freed from surrounding fibromuscular tissue.



