Chapter 20 Emergency Care of Musculoskeletal Injuries
Epidemiology of Orthopedic Injuries
Accidents continue to be a prominent cause of death and disability throughout the world. In the first 5 decades of life, trauma accounts for more deaths than any other cause. In all age groups, accidents are the fifth leading cause of death in the United States. In general, the amount of energy absorbed by a multiply injured patient corresponds to the extent of the musculoskeletal injuries. Because high energy is frequently involved, fractures and soft tissue injuries are common. Campbell et al found a 49% incidence of musculoskeletal injury among 5900 trauma patients seen at a level on trauma center from 2004–2006.1 When the disability associated with musculoskeletal injuries is tabulated, the ensuing costs are staggering; hundreds of billions of dollars are consumed by medical expenses, lost productivity, and property damage annually.
Terminology
Fracture Types
A fracture is a disruption of the normal architecture of bone. Fractures can be acute, subacute, or chronic. Acute fractures have sharp, well-defined edges of the fragments. Subacute fractures have signs of healing present on x-ray. The edges become blunted and less well defined as bony resorption and new bone formation occur. Chronic fractures have a rounded and sclerotic appearance after resorption and remodeling of bone has occurred at the fracture ends (Fig. 20-1). This distinction can usually be made on clinical examination. Chronic fractures are often termed delayed unions or nonunions. A delayed union is defined as a fracture that is taking longer to show progression toward healing than would normally be expected. The expected healing time varies, depending on the age of the patient and anatomic location of the fracture. For example, long bones in adults typically take 6 to 8 weeks to achieve full bony union, whereas pediatric fractures and metaphyseal fractures take less time. A nonunion is a fracture that has lost the potential to progress with healing. Generally, nonunion of a long bone is a fracture that has failed to show evidence of healing over a 4- to 6-month period.2 Chronic repetitive trauma can also cause microscopic disruptions when bone is stressed beyond its failure point. These injuries are termed stress fractures and are considered overuse injuries.
Because of increased plasticity, a more substantial periosteum, and the presence of growth plates, children’s bones are at risk for a different set of fractures (Fig. 20-2). Plastic deformity of a long bone in a pediatric patient is deformation of the bone without actual disruption of the bony cortex. Diagnosis of the deformity often necessitates radiography of the contralateral extremity to confirm asymmetry. Axial loads of long bones in children can lead to buckling of the cortex without a visible fracture line, appropriately termed a buckle fracture. Incomplete disruptions of the cortex are termed greenstick fractures in children or infractions in adults. A greenstick fracture consists of a cortical disruption on one side of the bone, with a buckle fracture or plastic deformation on the opposite side. The dense periosteal layer in children can contribute stability to many of these fractures if the layer remains intact. A fracture through the cartilaginous growth plate (physis) is another fracture type unique to children. A pure physeal fracture may not be radiographically apparent. These fractures are diagnosed clinically by the presence of pain over the growth plate.
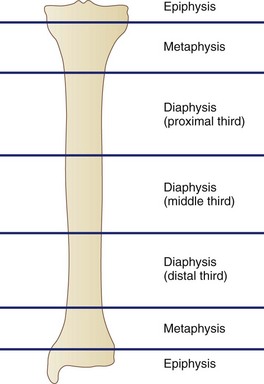
Long bone fractures are characterized by anatomic location (Fig. 20-3). The epiphysis includes the area between the physis, or physeal scar, and articular surface. The metaphysis is located between the epiphysis and shaft and includes the growth plate. The diaphysis encompasses the shaft of the bone between the proximal and distal metaphyses. The diaphysis is made up of mostly dense cortical bone, which has less vascularity than the soft cancellous bone of the metaphysis. This difference in vascularity affects the rate at which the bone heals. Fractures can be described according to location within these three sections or according to the location in the bone—proximal, middle, and distal. In addition, fractures within the diaphysis are usually divided into thirds (i.e., proximal, middle and distal thirds). Distally, the humerus and femur flare to form their articular surfaces. These flares are termed the epicondyles, and fractures in these areas are referred to as supracondylar or intracondylar. The articular surfaces distal to the epicondyles are known as condyles. Intracondylar fractures are intra-articular and may extend proximally. Such distinctions are important because these injuries present difficult treatment challenges.
A fracture may also be described by the pattern of cortical disruption (Fig. 20-4). The orientation of the primary fracture line may be transverse, oblique, or spiral. Transverse and oblique fractures occur when a bending moment is applied. Oblique fractures can be further characterized as long or short oblique. Spiral fractures generally result from a rotational force about the long axis of the bone. Comminution is the presence of multiple fragments within an individual fracture site and usually indicates a higher-energy injury or weakened bone in an older patient. A butterfly fragment is an area of comminution in one of the simple fracture patterns described earlier. Segmental fractures are fractures that occur at multiple levels in the same bone.
Fixation Principles
External Fixation
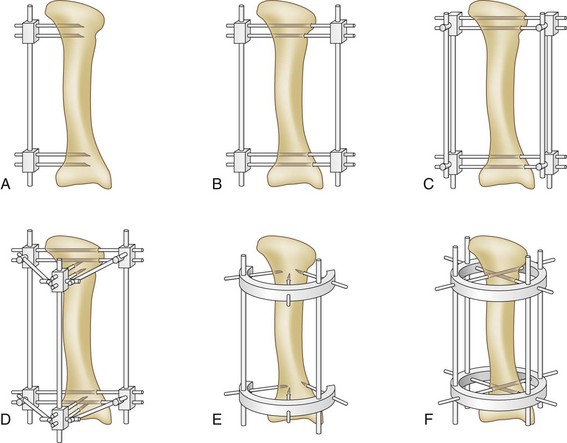
External frames are constructed from three components, pins, connectors, and rods or rings (Fig. 20-5). Pins are threaded or smooth and vary in length and diameter. They serve to connect the bone to the rest of the device. Pin placement is chosen to stabilize the fracture best while not compromising the viability of the fragments. Pins are never placed through compromised or infected skin. A variety of different clamps serves as connectors and secure pins to the rods that form the external frames. Most are universal joints that allow multiple degrees of freedom. Connecting clamps have advanced to the point that they now snap in place onto the pins and rods. They may be combined with rings or hinged rods and allow infinite permutations of frame constructs. Stabilizing rods are almost universally radiolucent to allow radiographic examination after application. Threaded rods, bone transport rails, motorized lengthening devices, and dynamic struts represent a small sample of the types of rods that can be used to achieve specific results.
Internal Fixation
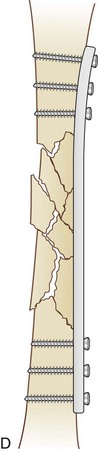
Pins and Screws
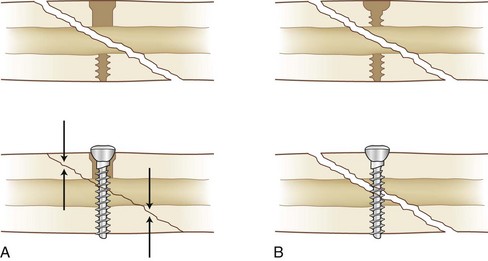
Pins and screws are the simplest implants. They can be introduced in a variety of areas and are often placed percutaneously through a poke hole in the skin. Kirschner wires may be used temporarily and frequently are used for the stabilization of small fragments. They can also be used provisionally to hold the fracture reduction while more stable fixation is applied. Screws can be used for interfragmentary compression when placed with a lag technique (Fig. 20-6). This technique involves the use of a gliding hole in one fragment to allow the screw to compress one fragment against another. Figure 20-6B shows a position screw. Without a gliding hole, a fully threaded screw will capture both fragments without compressing the far fragment to the near one, thus holding the position of the fragments.
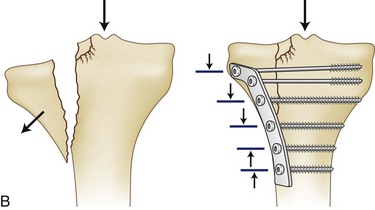
Plates
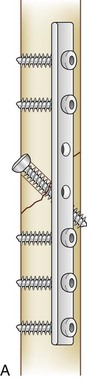
Plates are used frequently for the internal fixation of fractures. They allow even distribution of force across their length and can serve various biomechanical functions. The biomechanical properties of a plate depend on the material used, usually titanium or stainless steel, dimensions of the plate (thickness, width, and length), and technique with which it is applied (Fig. 20-7).
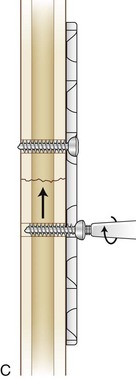
Tension Bands
When the forces across a fracture site tend to displace the fractured pieces in tension, the tension band technique can be applied to convert the displacing tensile forces on one side of a fracture into a compressive force across the entire contact area (Fig. 20-8). Traditionally, wires or cables are used to create tension bands. However, nonabsorbable suture and plates can also be used. Tension bands are used most frequently for fractures of the olecranon, where the pull of the triceps tends to distract the proximal fragment, and fractures of the patella, where the pull of the quadriceps tends to distract the superior pole. They are also commonly used for the femoral greater trochanter, humeral greater tuberosity, and medial malleolus.
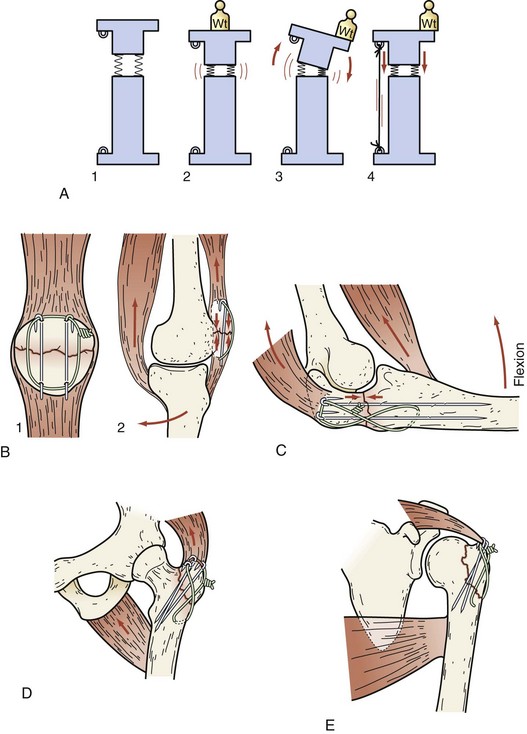
Intramedullary Nails
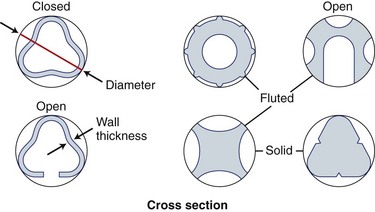
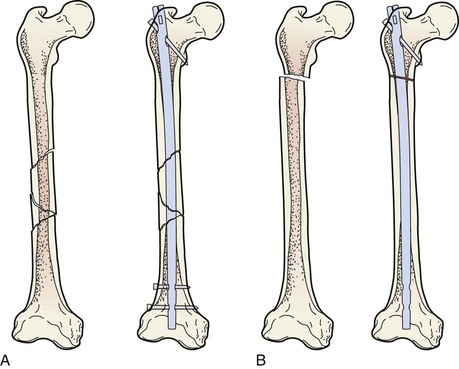
In contrast to wires, plates, and screws, intramedullary (IM) nails are placed in the medullary canal of long bones. They are used to splint or bridge a fracture and to control axial, bending, and rotational forces. IM nailing also permits fixation of a fracture through an incision distant from the fracture site. In this way, the periosteal blood supply at the fracture site is left undisturbed. Nails are made of various materials and can be fluted, smooth, solid, or cannulated (Fig. 20-9). When transverse screws are placed through the proximal and distal ends of the nail, the nail is said to be locked. Locked nails control rotation better and maintain bone length in the presence of comminution or bone loss. The locking holes in nails may be round or oval. Using a nail with an oval hole or leaving the nail unlocked at one end allows the bone fragment to slide axially along the nail and produces compression at the fracture site. Nails locked in this fashion are dynamically locked. When screws are inserted through round holes in both ends of the nail, no motion is allowed within the construct; they are statically locked (Fig. 20-10).
Patient Evaluation
History
Obtaining a detailed history of a skeletally injured patient is essential for accurate diagnosis and treatment. This can be challenging with multiply injured and older patients in the trauma setting; however, it is important to gather as much information as possible regarding the mechanism of injury. Often, trauma patients are unable to give accurate histories because of unconsciousness, intoxication, dementia, or delirium. In these cases, an account of the mechanism of injury and patient history should be obtained from family members, emergency medical response crew members, or other witnesses to the accident. Descriptions from the injury scene can be helpful because common patterns of injury follow from specific mechanisms (Table 20-1).
Table 20-1 Common Patterns and Associated Injuries
| INJURY PATTERN OR MECHANISM | ASSOCIATED INJURIES |
|---|---|
| Fall from a height | |
| Fall on outstretched hand (FOOSH) | |
| Ejection from a vehicle | |
| T-bone motor vehicle accident | |
| Head-on motor vehicle accident | |
| Posterior knee dislocation | |
| Supracondylar humerus fracture | |
| Anterior shoulder dislocation | |
| Posterior hip dislocation |
Trauma Room Evaluation
Examination of a multiply injured patient must first follow advanced trauma life support (ATLS) protocols in a systematic fashion and must be accompanied by appropriate treatment. The concept of life before limb demands that the ABCs (airway, breathing, and circulation) be addressed prior to evaluating for any orthopedic injuries. Hemodynamically unstable patients are assumed to be in hemorrhagic shock until proven otherwise. A search for occult hemorrhage is undertaken and may include the pleural cavities, abdomen, retroperitoneum, and pelvis. A plain chest radiograph may quickly reveal a hemothorax. Chest tubes are placed, if necessary. Pelvic instability and the need for rapid external pelvic fixation are addressed. There is debate over whether the anteroposterior (AP) pelvic film, which has traditionally been considered part of the standard trauma radiographic series, is justified with the advent of newer, ultrafast computed tomography (CT) scanners. Recent data have shown that in a stable awake patient who has no evidence of pelvic injury on physical examination, routine use of this study may not be cost-effective.3 However, in a patient with signs of pelvic injury on examination, hemodynamically unstable patient, or obtunded patient, the pelvic radiograph is essential for identifying unstable pelvic injury requiring immediate intervention in the trauma bay.4 In addition, the pelvic radiograph is necessary for preoperative planning in operative fractures and as a comparison film when following fracture healing over time. A FAST (focused assessment with sonography in trauma) scan has been shown to be a rapid and effective technique for assessing for free fluid in the abdomen.5 Positive scans have been shown to be strongly predictive of the need for laparotomy in hypotensive trauma patients. However, Gaarder and colleagues6 have found that even in the hands of experienced radiologists, the FAST scan is a relatively unreliable technique for detecting intra-abdominal bleeding in the hemodynamically unstable patient. Cha and associates7 have agreed with this conclusion and suggest that diagnostic peritoneal lavage and/or CT of the chest, abdomen, and pelvis be considered in hemodynamically unstable patients with suspected intra-abdominal injuries.
In their landmark article, Bone and coworkers8 have shown that urgent (within the first 24 hours) versus late stabilization in the multiply injured patient reduces the incidence of adult respiratory distress syndrome (ARDS) and multisystem organ failure. In addition, with adequate stabilization of the fracture, the patient can be mobilized, avoiding convalescence. However, more recently, Morshed and colleagues9 have shown that emergent fixation—within 12 hours—of femoral shaft fractures in polytrauma leads to an increased mortality rate. They suggest that this finding is likely caused by inadequate time for patient resuscitation in those taken to surgery in the first 12 hours from the time of injury. In isolated or less severe injuries, once the patient is stabilized, the timing of repair is less significant. Operative delay allows for resolution of the soft tissue swelling that may compromise soft tissue closure.
Plain radiographs of the cervical spine, including AP, lateral, and open-mouth odontoid views were previously considered part of the standard trauma series of radiographs. Recently, however, Mathen and associates have shown that the standard plain films fail to identify 55.5% of clinically relevant fractures identified by multislice CT and add no clinically relevant data.10 Similarly, a CT of the thoracic, lumbar, and sacral spine is faster and more accurate than radiography at identifying traumatic injury. With most trauma patients undergoing a CT of the chest, abdomen, and pelvis, reformatting the data into spinal reconstructions adds neither time nor radiation exposure. With this data, plain films are no longer indicated.
Examination of the extremities in a patient with isolated injuries or a multitrauma patient follows a simple, systematic, and reproducible pattern. Even when an isolated extremity injury is the primary reason for evaluation, the entire skeleton must be examined. The examiner must not be distracted from the task by obvious or severe injuries. Deformity, edema, ecchymosis, crepitus, tenderness, and pain with motion are the cardinal signs of an acute fracture. Each limb segment needs to be examined for lacerations and the signs of trauma described earlier. All joints are put through passive range of motion, at a minimum. Active range of motion is tested whenever possible. Joint effusions are evidence of intra-articular pathology (e.g., ligament or cartilage damage, or an intra-articular fracture). The joints are then manually stressed to assess the integrity of the ligamentous structures. A neurovascular examination is performed and documented. Pulses are recorded and compared with the opposite uninvolved extremity when possible. Doppler signals are obtained when palpable pulses are not present or are weak. Measuring the ankle-brachial index (ABI) is important when vascular injury is suspected. Motor function and sensation must be documented for the extremity dermatomes as well as the trunk in a patient with thoracic spine pain. To avoid the complications of a missed compartment syndrome, palpation of the involved compartments is performed. Any firm or tense compartments are checked for increased pressure if time and the patient’s condition allow. Fasciotomies are performed urgently if pressures are elevated. Gross alignment and interim immobilization of long bone fractures are achieved before transportation of the patient from the trauma room. This helps prevent further damage to underlying soft tissues, reduces patient discomfort, facilitates transportation, and may help prevent further embolization of IM contents.11 Traction splints or skeletal traction are applied when indicated.
Diagnostic Imaging
Because bone is a three-dimensional object, a single two-dimensional radiograph cannot describe a fracture. To understand the position and direction of the fracture fragments, orthogonal views (images taken at 90 degrees to one another) must be obtained. A bone may appear minimally displaced in one plane, but in another view may be significantly displaced (Fig. 20-11). All extremities with deformity need to be rotated to the anatomic position before taking radiographs to help decrease confusion when describing the fracture. When finer detail is necessary to evaluate a fracture pattern better or confirm the findings of an equivocal x-ray, a CT scan should be ordered. Magnetic resonance imaging (MRI) has become a particularly useful imaging modality. It is used to evaluate soft tissue, acute fractures, stress fractures, spinal cord injuries, and intra-articular pathology. Its role in the trauma setting has expanded as well, and it is particularly helpful in the setting of spinal cord injury. More frequently, MRI is used in the outpatient setting to evaluate soft tissue injuries and pathologic lesions. MRI is now commonly used for the diagnosis of acute fractures when plain films are negative.
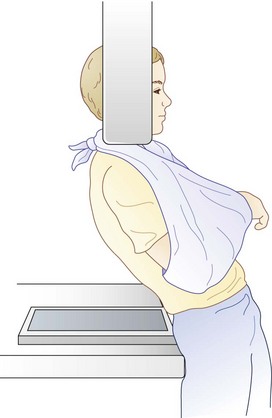
Shoulder
True AP and lateral views of the shoulder must be taken in relation to the scapula because of the orientation of the joint. The most useful lateral view is an axillary radiograph. The tube is angled cephalad, with the plate on the superior aspect of the abducted shoulder. This view is often difficult to obtain because of pain or instability at the proximal end of the humerus. The Velpeau view is a modified axillary view, which provides orthogonally equivalent images. While wearing a sling, the patient leans backward 30 degrees over the cassette on the table. The x-ray tube is placed above the shoulder and the beam is projected vertically down through the shoulder onto the cassette (Fig. 20-12). This allows the x-ray to be taken with the shoulder adducted and in a sling, allowing acquisition of the axillary images without the pain of shoulder abduction.
Elbow
AP and lateral views of the elbow provide visualization of most of the bony anatomy. Internal and external obliques are included in a complete elbow series and allow for better visualization of the medial and lateral epicondyles. On the lateral view, look for the fat pad sign or the sail sign for evidence of an occult fracture. The sail sign can be noted when hemiarthrosis from an intra-articular fracture forces the anterior and posterior fat pads out of the coronoid and olecranon fossae, respectively. On x-ray, the visualized fat pads resemble a sail (Fig. 20-13). Although the anterior fat pad can be visualized in a normal elbow, the presence of a posterior fat pad sign is strongly suggestive of occult fracture and, if clinically appropriate, warrants a CT scan.
Pelvis and Acetabulum
The standard AP radiograph of the pelvis provides an overview to the structural integrity of the hips and pelvic ring. If pelvic pathology is noted on this film or suspected from physical examination, further views are necessary. Judet views, or 45-degree oblique views of the pelvis, are used to evaluate the acetabuli (Fig. 20-14). Because of the spatial orientation of the acetabulum, these views represent orthogonal projections when the x-ray tube is canted toward or away from the affected side. Similarly, inlet and outlet views of the pelvis allow closer examination of the sacroiliac joints and the sacrum itself, as well as identifying AP disruption in the pelvic ring. The inlet view is taken with the beam angled 60 degrees caudad, thus making the beam perpendicular to the pelvic brim. The sacral ala, displacement of the sacroiliac joints, and displacement of the pubic symphysis in the AP plane are easily seen. The outlet view is a 30-degree oblique view, with the tube angled cephalad. The sacrum is pictured en fosse, and the neural foraminae are easily evaluated. If not already obtained as part of the trauma workup, a pelvic CT should be ordered to evaluate fractures of the acetabuli and sacrum. This allows detailed evaluation of the amount of articular involvement, displacement, and presence of bony fragments within the joint. It also provides information regarding sacral displacement or neural foraminal involvement. Finally, it allows evaluation for intrapelvic hematoma. MRI has little role in acute, traumatic pelvic ring injury; however, it is the imaging modality of choice for suspected osteomyelitis or pelvic abscess.
Hip
A hip series consists of AP and cross-table lateral x-rays. In an adult patient with acute groin pain and inability to bear weight, an occult hip fracture should be ruled out with an MRI or bone scan. In older patients with occult osteopenic hip fractures, bone scans, although accurate, are unreliable within 48 hours after injury. MRI has been shown to be at least as accurate as bone scans in the diagnosis of acute fractures. Additionally, the sensitivity and specificity of MRI were the same within 24 hours of admission as later. Earlier diagnosis can potentially lead to shorter hospital stays and, therefore, in theory offset the additional cost of MRI. In patients with femoral shaft fractures, the incidence of ipsilateral femoral neck fracture is as high as 9%. A protocol of AP internal rotation views of the hip, as well as thin cut CT (2-mm cuts) through the femoral neck in the emergency department (ED), has been shown to decrease the incidence of delayed diagnosis of this injury.12
Knee
AP, lateral, and internal or external oblique plain films allow visualization of most traumatic osseous abnormalities of the knee. If possible, standing films are useful for evaluating knee alignment and joint space narrowing. The lateral film can show an effusion, patellar fracture, posterior tibial plateau fracture, or tibial tubercle injury. If there is any doubt as to the degree of articular involvement, displacement, or depression, a CT scan should be ordered (Fig. 20-15). Although an MRI can be helpful in the acute setting, evaluation of ligamentous derangement is not urgent and can be deferred to the outpatient setting. In the setting of a knee dislocation, vascular injury should be assumed until proven otherwise. Serial measurements of the ABI are useful to monitor for vascular compromise, but vascular imaging in the form of CT angiography (CTA) or MR angiography (MRA) should be strongly considered in the setting of an acute knee dislocation.
Ankle
In the ankle, it is important to confirm maintenance of the mortise. The stability of the mortise depends on bony and ligamentous support. With AP, mortise, and lateral x-rays, disruptions in the bony anatomy can be visualized directly. Although the ligamentous structures cannot be visualized directly, assumptions about their continuity can be made by evaluating the spaces between the bones. Three main parameters are commonly used are the tibia-fibula overlap, tibia-fibula clear space, and medial clear space (Fig. 20-16). All three parameters should be measured on the AP radiograph. The medial clear space is the distance between the medial border of the talus and lateral border of the medial malleolus. A normal value is less than 4 mm. The tibia-fibula clear space is the distance between the medial border of the fibula and floor of the incisura fibularis. A normal value is less than 5 mm. The tibia-fibula overlap is the amount of the lateral tibia overlapping the medial fibula. A normal value is more than 10 mm. In an adult ankle, there should be some degree of tibia-fibula overlap in all views. Both the tibia-fibula clear space and overlap are measured 10 mm proximally to the tibial plafond. Excluding a direct blow injury, sustaining an isolated medial malleolar fracture is exceedingly rare. Most ankle injuries are caused by a twisting moment imparted to the ankle. The energy that enters through the medial malleolus must exit at some point on the lateral ankle. This may result in a lateral collateral ligament tear (rare), lateral malleolar fracture, or a more proximal fibula fracture. In some cases, the energy passes through the syndesmosis and exits at the proximal fibula. This is known as a Maisonneuve fracture. The disruption results in an unstable ankle mortise, which influences the treatment plan. Because of this, any isolated medial malleolar fracture should always get full-length AP and lateral tibia-fibula x-rays. In the case of an intra-articular fracture of the weight- bearing surface of the tibia (pilon fracture), a CT can be useful to evaluate the joint surface.
Foot
When an injury of the foot is suspected, the workup should start with a standard series of AP, lateral, and oblique x-rays. However, because of the complex three-dimensional structure of the foot, this standard series of films may not be adequate to visualize certain bones. In the case of a calcaneus fracture, a Harris axial view should be added to evaluate the varus-valgus alignment of the tuberosity, as well as any sagittal splits in the bone. Bohler’s angle—an angle formed by the bisection of a line drawn from the superior aspect of the calcaneal tuberosity to the superior aspect of the posterior facet and a line drawn from the tip of the anterior process to the superior aspect of the posterior facet—should be evaluated in the lateral view (Fig. 20-17). A normal Bohler’s angle is between 20 and 40 degrees. A decrease in this angle usually indicates fracture, with depression of the posterior facet. When in doubt, films of the uninjured foot should be taken for comparison. For fractures of the talus, the AP and lateral films should be evaluated for articular congruence at the tibiotalar, subtalar, and talonavicular joints. There are specialized views of the bone (e.g., Canale view for the talar neck and Broden’s view for evaluation of the subtalar joint); however, these views are radiology technician–dependent. In many cases, if a fracture is seen on the AP or lateral views, a CT scan is a faster and more cost-effective way to evaluate the displacement pattern. If x-rays are negative or equivocal and the patient has evidence of fracture—ecchymosis, pain out of proportion to plain film findings, significant soft tissue swelling—then a CT scan should be ordered. All but the most minimally displaced intra-articular fractures of the talus and calcaneus warrant a CT scan to define the fracture pattern and extent of articular displacement better. Except in the case of suspected osteomyelitis, MRI of the foot is of little use in the emergency setting.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree