INDICATIONS
The indications for an OTW (Eloesser flap or Clagett window) are as follows:
 Chronic empyema
Chronic empyema
 Patients with significant comorbidity and prohibitive surgical risk who are not able to tolerate decortication.
Patients with significant comorbidity and prohibitive surgical risk who are not able to tolerate decortication.
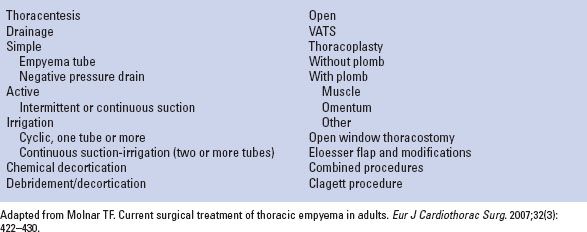
TABLE 23.1 Treatment Modalities for Thoracic Empyema
 Patients waiting for a more radical procedure (allows for nutritional buffering)
Patients waiting for a more radical procedure (allows for nutritional buffering)
 No response to conventional therapy
No response to conventional therapy
 Patients who are unresponsive to treatment modalities, which include tube thoracostomy and decortication.
Patients who are unresponsive to treatment modalities, which include tube thoracostomy and decortication.
 Patient too debilitated for a major thoracic procedure
Patient too debilitated for a major thoracic procedure
 Expectation of long-term drainage
Expectation of long-term drainage
 Discomfort from tube drainage placed posteriorly
Discomfort from tube drainage placed posteriorly
 Patients who are noncompliant
Patients who are noncompliant
 Postpneumonectomy empyema (with or without bronchopleural fistula)
Postpneumonectomy empyema (with or without bronchopleural fistula)
 SURGERY
SURGERY
Original Description of Eloesser Flap
The original procedure was described using local anesthesia. A U-shaped flap of skin and subcutaneous tissue is initially marked before making incision (Fig. 23.1). This U-shaped flap is half way between the posterior axillary line and the line at the inferior most portion of the scapula. The base of the flap is 2-in wide and is one rib space above the lower extent of the empyema cavity. The length of the flap is equivalent to the length of two rib spaces to ensure the flap reaches the pleural space. The rib and associated intercostal muscle directly beneath the flap is resected to the length of the flap itself. The tip of the flap is placed into the chest and the flap is sutured to the pleura at the apex and laterally using absorbable suture (Fig. 23.2). The wound is subsequently packed. As the lung parenchyma expands, the cavity collapses. The flap acts as a one way valve as an increase in intrapulmonary pressure creates negative pressure within the empyema cavity allowing the lung to re-expand and obliterate the space (Fig. 23.3).
Modified Eloesser Flap (MEP)
This technique was introduced into the literature in 1971 by Symbas et al. Essentially the principles are the same as the original technique described by Eloesser in 1935. Again, the procedure can be performed with local or general anesthesia. The location of the MEP is dependent on the location of the empyema cavity. In contrast to the original technique, an inverted U flap is incised over the empyema cavity. The flap includes skin and the subcutaneous tissue. The base of the flap is directly over the lower most extent of the empyema (in contrast to the original EF where the base of the flap is two rib spaces over the lower extent of the empyema cavity). The length of the flap is approximately two ribs including intercostal spaces. A segment of the underlying rib is resected, or multiple segments of one or more ribs may be resected depending on the size of the empyema and the body habitus of the patient. The flap is then sutured to the base of the cavity using large absorbable suture (Fig. 23.4A–F).
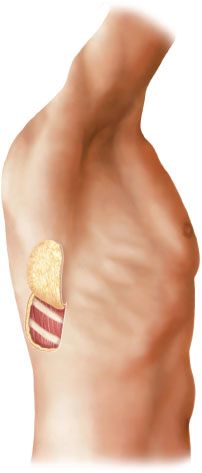
Figure 23.1 Flap of skin outlined.

Figure 23.2 Cross section of chest wall showing skin flap turned into chest and attached to pleura.
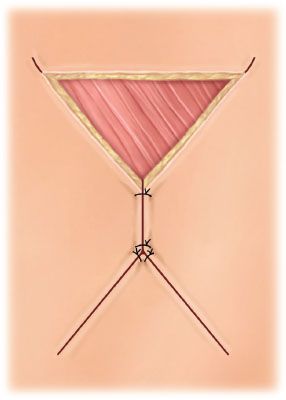
Figure 23.3 Skin flap turned into chest cavity; edges of defect approximated by sutures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


