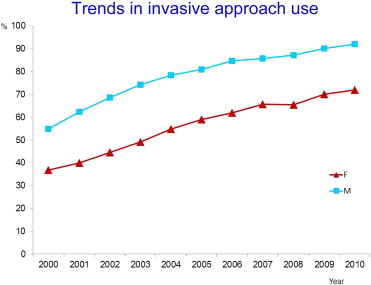
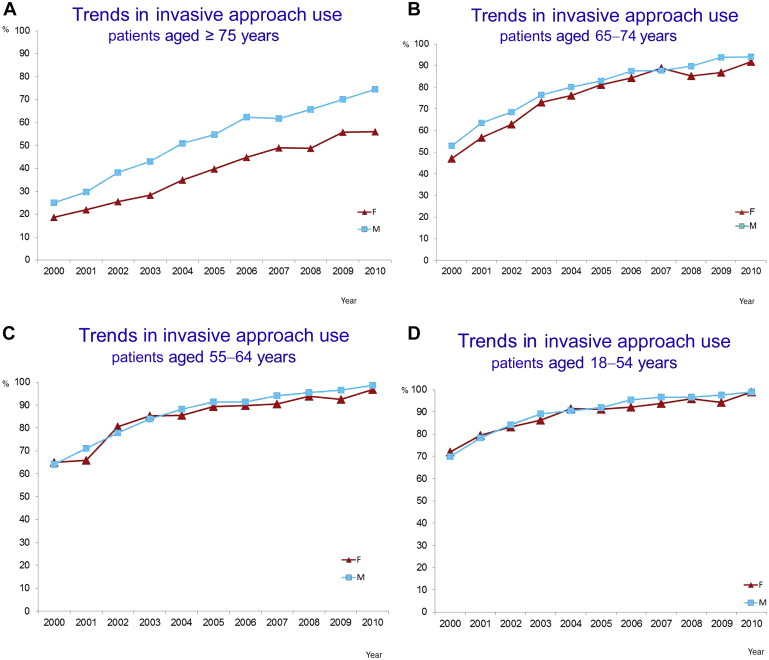
The aim of this study was to assess recent trends in hospital mortality and in the treatment techniques for patients with ST-segment elevation myocardial infarction according to gender. Data on hospitalizations for ST-segment elevation myocardial infarction from 2000 to 2010 were extracted from hospital discharge record databases ( International Classification of Diseases, Ninth Revision, Clinical Modification , codes) in the Lombardy Region of Italy. The impact of female gender on in-hospital mortality was assessed by multivariable regression after adjusting for invasive approach use (i.e., coronary angiography, angioplasty or coronary artery bypass graft), age, and co-morbidities. A total of 89,562 patients, men (66.5%) and women (33.5%), were enrolled. The use of an invasive approach increased over time in both sexes although it was higher in men (from 54.9% in 2000 to 91.9% in 2010 in men; from 36.8% in 2000 to 72.0% in 2010 in women). This pattern was driven by the subgroup of patients aged ≥75 years, whereas differences between sexes were not observed in patients <65 years and were small in patients aged 65 to 74 years. In-hospital mortality presented a small decrease from 7.6% in 2000 to 6.2% in 2010 in men (p for trend = 0.004), whereas it remained higher and substantially constant over time in women (16.6% in 2000, 15.5% in 2010, p for trend = 0.09). At multivariable regression, female gender did not emerge as an independent predictor of mortality (p = 0.13). However, a significant gender-age interaction was found, with female gender being a significant predictor of increased mortality in patients aged ≥75 years (odds ratio [OR] 1.33) while predicting a reduced mortality in patients aged <75 years (OR 0.93, p for interaction <0.0001). The use of an invasive approach was an independent predictor of mortality (OR 0.23, p <0.0001), the magnitude of mortality reduction being higher in men than in women and in patients aged <75 years than in those aged ≥75 years. In conclusion, a weak temporal trend in mortality reduction is observed in men only, which is driven by patients aged ≥75 years. In-hospital mortality remains higher in women than in men, although female gender is not a significant predictor of mortality. Despite temporal increases in the use of an invasive approach, women are more often treated conservatively.
Several studies have reported a higher mortality in women than in men after ST-segment elevation myocardial infarction (STEMI). A higher cardiovascular risk profile and older age of women have been considered to play a role in this difference. Furthermore, delayed reperfusion in women and generally undertreatment of women as compared with men have been reported in several studies. Over the past 15 years, a decrease in short-term mortality in patients with STEMI has been reported. This finding has been mainly related to an increase in myocardial reperfusion, in particular of primary percutaneous coronary intervention (PCI). Nevertheless, whether gender disparities still exist in the treatment and mortality of patients after STEMI remains controversial. The aim of this study was to assess recent trends in hospital mortality and in the treatment techniques for patients with STEMI according to gender in a population-based cohort study.
Methods
Cross-sectional data on all hospitalizations in Lombardy, a large Northern Italy region with >9.5 million subjects, during 2000 to 2010 were extracted from the regional hospital discharge record (HDR) database that covers all patient admissions to hospitals connected to the network of Italian National Health System. Briefly, all HDRs that belonged to major diagnostic category groups 1, 4, and 5, corresponding to neurologic, respiratory, and cardiovascular diseases, respectively, were extracted according to the main diagnosis on hospital discharge. Hospital admissions because of myocardial infarction (MI) were identified according to the following criteria: all admissions of patients aged >18 years, the presence of codes ( International Classification of Diseases, Ninth Revision, Clinical Modification [ ICD-9-CM ]) from 410.00 to 410.91 if MI was the primary diagnosis or if MI was reported as a secondary diagnosis, with a major cardiac complication reported as primary diagnosis and identified with the following codes (427.1, 427.41, 427.42, 427.5, 428.1, 429.5, 429.6, 429.71, 429.79, 429.81, 518.4, 780.2, 785.51, 414.10, and 423.0).
STEMI was defined according to the codes ICD-9-CM 410.00 to 410.61. The codes 410.70, 410.71, 410.8, and 410.9 were an exclusion criteria to exclude patients with NSTEMI.
All admissions with a hospital stay of ≤1 day without death or transferral to another facility as reason for discharge were excluded. Two hospital admissions of the same patient were considered related to a single infarction episode if these were separated by no >1 day. Only patients with first MI in the period considered were included in this study. Data about sex, age, date of admission, and admission ward were extracted from HRD. Admission wards were classified as (1) intensive coronary care unit (ICCU), (2) cardiology ward, and (3) noncardiac ward. Furthermore, the following data were extracted using all information available from the HDR: treatments received by the patients, in-hospital complications, and in-hospital death. The treatment techniques were classified as (a) coronary angiography alone without PCI or coronary artery bypass surgery according to the following codes (88.55, 88.56, and 88.57), (b) PCI with or without stent implantation using the following codes (36.01, 36.02, 36.05, and 36.06), and (c) coronary artery bypass surgery (code 36.1). When none of the earlier mentioned codes was found, patients were considered they had been treated by medical therapy alone. Therefore, patients were grouped in those who underwent an invasive approach (including coronary angiography alone, PCI, or coronary artery bypass) and those who underwent medical therapy alone. The following cardiac complications were extracted: arrhythmic complications according to the codes 427.1, 427.41, 427.42, 427.5, 428.1, 429.5, 429.6, 429.71, 429.79, and 780.2; mechanical complications according to the codes 429.5 to 429.6, 429.7, 414.10, and 423.0; acute heart failure according the codes 428.1, and 518.4; and cardiogenic shock according to the code 785.51. The following co-morbidities were extracted from patient hospital admissions before the index hospitalization for MI and occurring within 5 years earlier: chronic renal failure, peripheral artery disease, chronic obstructive patient disease, and neoplasms. The distribution of continuous variables was assessed by visual inspection of their frequency histograms and using the Shapiro-Wilk test. Continuous variables are expressed as mean and SD or median and twenty-fifth to seventy-fifth percentile, according to a Gaussian or non-normal distribution, respectively. Continuous variables were compared by t test. Categorical variables are expressed as percentage and were compared by chi-square or Fisher’s exact tests as appropriate. The Cochran-Armitage test was used for trend analysis. A multivariable logistic regression was performed to assess predictors of in-hospital death, and odds ratio (OR) with 95% confidence intervals (CIs) were calculated. Variables associated with death at simple logistic regression analysis (with a p-value <0.05) entered the model, that is, age, female gender, invasive approach, admission ward, time period, arrhythmic complication, mechanical complication, left ventricle failure, shock, renal failure, peripheral vascular disease, chronic obstructive disease, and neoplasm. The impact of time period on in-hospital death was assessed by entering a dichotomous variable of time coded as 1 = time period from 2006 to 2010 and 0 = time period from 2000 to 2005. The interaction between female gender and using an invasive approach was assessed by adding an interaction term: gender × invasive approach to the multivariable model. Gender-strata OR with 95% CI were reported if the interaction was statistically significant. A two-tailed p-value <0.05 was the level of statistical significance. All analyses were performed with SAS statistical package, version 9.2 (SAS Institute, Inc, Cary, NC).
Results
Between 2000 and 2010, a total of 89,562 patients, men (66.5%) and women (33.5%), have been admitted to the hospital. Baseline clinical characteristics according to sex are listed in Table 1 . Briefly, women were older than men. The gap in mean admission patient age between sexes tended even to slightly increase over time. Women presented a higher prevalence of chronic renal failure and a lower prevalence of peripheral vascular disease and neoplasms ( Table 1 ). First admission ward was more frequently ICCU in both sexes ( Table 1 ). However, admission to ICCU was more frequent in men than in women, whereas admission to noncardiac ward was more frequent in women than in men ( Table 1 ). The use of an invasive approach increased over time in both sexes, although it remained higher in men (from 54.9% in 2000 to 91.9% in 2010 in men; from 36.8% in 2000 to 72.0% in 2010 in women) ( Figure 1 ). A similar trend in the use of an invasive approach was observed in the subgroup of patients aged ≥75 years (from 24.9% in 2000 to 74.4% in 2010 in men; from 18.7% in 2000 to 56.1% in 2010 in women, Figure 2 ), whereas in age categories <65 years the rate of invasive approach was comparable in both sexes, and small differences were observed in patients aged 65 to 74 years ( Figure 2 ). A temporal trend in increasing use of PCI was observed in both sexes, although PCI use remained higher in men (from 32.4% in 2000 to 82.4% in 2010 in men; from 21.0% in 2000 to 58.5% in 2010 in women) ( Figure 3 ). A decline in the rate of coronary angiography alone was observed mainly in men (from 17.3% in 2000 to 5.6% in 2010) and to a lesser degree in women (from 12.4% to 10.6% in 2010). In-hospital mortality presented a small decrease from 7.6% in 2000 to 6.2% in 2010 in men (p for trend = 0.004), whereas it remained higher and substantially constant over time in women (16.6% in 2000, 15.5% in 2010, p for trend = 0.09) ( Figure 4 ). This trend in the overall population pattern was driven by the subgroup of patients aged ≥75 years ( Figure 5 ). At multivariable analysis, female gender was not a significant predictor of mortality ( Table 2 ). However, a significant interaction was found between gender and age ≥75 years, with female gender being a significant predictor of increased mortality in patients aged ≥75 years (OR 1.33, 95% CI 1.20 to 1.46) while predicting a reduced mortality in patients aged <75 years (OR 0.93, 95% CI 0.87 to 0.99; p for interaction <0.0001). The use of an invasive approach was a significant predictor of reduced mortality ( Table 2 ), the magnitude of mortality reduction being slightly higher in men (OR 0.20, 95% CI 0.18 to 0.21) than in women (OR 0.28, 95% CI 0.26 to 0.31, p for interaction <0.0001) and in patients aged <75 years (OR 0.14, 95% CI 0.13 to 0.15) than in patients aged ≥75 years (OR 0.28, 95% CI 0.26 to 0.30; p for interaction <0.0001). In a subgroup analysis restricted to patients who underwent PCI, women, as compared with men, presented a significantly higher in-hospital mortality (16.3% vs 7.9%, p <0.0001; OR 2.27, 95% CI 2.17 to 2.37).
| Variable | Overall Population (n = 89562) | Men (n = 59569) | Women (n = 29993) | p |
|---|---|---|---|---|
| Age, years, mean (SD) | 67.5 (13.5) | 63.9 (12.6) | 74.9 (12.2) | <0.0001 |
| Age ≥75 years | 30375 (33.9%) | 13101 (21.9%) | 17274 (57.6%) | <0.0001 |
| Chronic renal failure | 5146 (5.7%) | 3103 (5.2%) | 2043 (6.8%) | <0.0001 |
| Peripheral vascular disease | 6191 (6.9%) | 4285 (7.2%) | 1906 (6.3%) | <0.0001 |
| Chronic obstructive pulmonary disease | 6707 (7.5%) | 4477 (7.5%) | 2230 (7.4%) | 0.6654 |
| Neoplasms | 2003 (2.2%) | 1396 (2.3%) | 607 (2.0%) | 0.0023 |
| Admission ward | <0.0001 | |||
| Intensive coronary care unit | 63888 (71.4%) | 44862 (75.4%) | 19026 (63.5%) | |
| Cardiac | 12071 (13.5%) | 7992 (13.4%) | 4079 (13.6%) | |
| Noncardiac | 13543 (15.1%) | 6671 (11.2%) | 6872 (22.9%) | |
| Arrhythmic complication | 1857 (20.7%) | 11196 (18.8%) | 7375 (24.6%) | <0.0001 |
| Mechanical complication | 1655 (1.8%) | 968 (1.6%) | 687 (2.3%) | <0.0001 |
| Left ventricular failure | 12298 (13.7%) | 6749 (11.3%) | 5549 (18.5%) | <0.0001 |
| Cardiogenic shock | 6052 (6.8%) | 3125 (5.5%) | 2927 (9.8%) | <0.0001 |