The ability of stent implantation to improve indexes of reperfusion may depend on the time to reperfusion in acute ST-segment elevation myocardial infarction (STEMI) and may also vary with stent type. The purpose of this prespecified analysis from the randomized MGUARD for Acute ST Elevation Reperfusion trial was to evaluate the impact of delay to reperfusion on outcomes in patients with STEMI undergoing primary percutaneous coronary intervention with the MGuard embolic protection stent or standard metallic stents. A total of 431 patients were divided according to symptom-onset-to-balloon time (SBT) into 2 groups: SBT ≤3 hours (167 patients; 39%) and SBT >3 hours (264 patients; 61%). Complete ST-segment resolution (STR) after percutaneous coronary intervention was more often achieved in patients with shorter SBT (58.6% vs 47%, p = 0.02). At 1 year, the all-cause mortality rate was lower in patients with shorter SBT (0% vs 3.5%, p = 0.02). STR was achieved in 58% of MGuard patients and in 45% of the control stent patients (p = 0.008). STR was 57% in the MGuard group versus 38% in the control group (p = 0.002 for SBT >3 hours) and 60% versus 57% (p = 0.72), respectively, for SBT ≤3 hours (p for interaction = 0.11). In conclusion, longer delay to mechanical reperfusion remains an important factor negatively influencing outcomes in patients with STEMI. Use of the MGuard embolic protection stent compared with conventional metallic stents resulted in superior rates of complete STR, even in patients with longer delays to reperfusion.
Highlights
- •
We performed a prespecified analysis of the MASTER trial (patients with ST-segment elevation myocardial infarction, primary percutaneous coronary intervention [PCI]).
- •
We evaluated the impact of delay to primary PCI according to the type of stent placed.
- •
We compared the MGuard embolic protection stent and conventional stents (drug-eluting stent and bare-metal stent).
- •
Complete ST resolution after PCI was more frequent in patients with shorter delay to PCI.
- •
The MGuard stent tended to be particularly beneficial in patients with delay to PCI >3 hours.
Primary percutaneous coronary intervention (PCI) is the recommended method of reperfusion in patients with ST-segment elevation myocardial infarction (STEMI). However, extended delay from symptom onset to mechanical reperfusion has a negative impact on clinical outcomes. This may be explained by larger infarct size with more frequent transmural infarction, larger areas of microvascular dysfunction and myocardial edema, and lower procedural success. The longer time to reperfusion may promote larger and more organized thrombus formation and render both pharmacologic and mechanical (aspiration thrombectomy) strategies less effective. It is unknown if this limitation may be overcome with a novel embolic protection stent design geared to reduce distal embolization. The purpose of this analysis from the MGuard for Acute ST Elevation Reperfusion (MASTER) trial was to evaluate the impact of delay to reperfusion on outcomes in patients with STEMI undergoing primary PCI according to the type of stent placed.
Methods
MASTER was an open-label, prospective, randomized, multicenter trial comparing the MGuard embolic protection stent (InspireMD, Tel Aviv, Israel) versus conventional metallic stents in patients undergoing primary PCI for STEMI. Study design and results were previously published. In brief, patients presenting with STEMI ≤12 hours, with ≥2 mm of ST-segment elevation in ≥2 contiguous leads, and intended for primary PCI were eligible for enrollment. Angiographic eligibility required planned PCI of a single de novo lesion ≤33 mm in length and reference vessel diameter ≥3.0 to ≤4.0 mm by visual estimation, amenable to coverage by a single study stent. Patients were not eligible if a ≥50% left main stenosis was present or if the target lesion was ostial in location or involved a bifurcation with a ≥2.0-mm side branch. In the case of an occluded infarct vessel, angiographic eligibility was assessed only after restoration of Thrombolysis In Myocardial Infarction (TIMI) flow grade ≥2 by a guidewire, manual aspiration, or balloon angioplasty. Patients were then randomized 1:1 to either the MGuard stent or any commercially available bare-metal stent or drug-eluting stent (the control stent group). The primary efficacy end point was the rate of complete ST-segment resolution (STR), defined as ≥70% reduction in the summed 12-lead ST-segment elevation from the baseline to the 60- to 90-minute postprocedural electrocardiogram. Electrocardiographic analysis was performed by a blinded independent electrocardiography core laboratory.
For the purpose of this prespecified analysis, the MASTER trial patient cohort was divided according to the symptom-onset-to-balloon time (SBT) into 2 groups: SBT ≤3 hours and SBT >3 hours. Clinical outcomes at 30 days and 1 year were analyzed for the occurrence of major adverse cardiovascular and cerebral events (the composite of all-cause death, reinfarction, stroke, or ischemia-driven target lesion revascularization), major adverse cardiovascular events (the composite of cardiac death, reinfarction, or ischemia-driven target lesion revascularization), ischemia-driven target vessel revascularization, stroke, stent thrombosis (Academic Research Consortium definition), and bleeding (TIMI classification). All events were adjudicated by an independent clinical events committee. The influence of stent type (MGuard vs control) on STR and clinical outcomes was assessed in the 2 SBT groups.
Data are presented as percentage or median with interquartile range, as applicable. Differences in categorical variables were analyzed using the chi-square test or Fisher’s exact test, as appropriate. Continuous variables were compared using Wilcoxon rank sum test. All tests were 2 tailed, and a p value <0.05 was considered statistically significant. All statistical analyses were performed using SAS, version 9.2 (SAS Institute Inc., Cary, North Carolina).
Results
A total of 431 patients were included in this analysis. SBT was ≤3 hours in 167 patients (39%) and >3 hours in 264 patients (61%). Patients with SBT ≤3 hours were younger and had higher rates of previous smoking ( Table 1 ). Pharmacologic treatment, target vessel location, and preprocedural TIMI flow grade were similar in both groups. Patients with shorter SBT were more likely to be treated with stent implantation without balloon predilation after thrombus aspiration. There was no difference in the type of implanted stent (MGuard vs control) between groups ( Table 2 ).
| Variable | Symptom Onset to Balloon Time (hours) | p-Value | |
|---|---|---|---|
| ≤3 (n = 167) | >3 (n = 264) | ||
| Age (years) | 57 [50, 65] | 60 [51, 67] | 0.02 |
| Male | 81% | 73% | 0.055 |
| Body mass index (kg/m 2 ) | 27.2 [24.7, 30.3] | 26.9 [24.4, 30.3] | 0.10 |
| Medically treated hypertension | 46% | 45% | 0.88 |
| Medically treated hyperlipidemia | 27% | 28% | 0.84 |
| Diabetes mellitus | 15% | 15% | 0.96 |
| Insulin-treated | 4.5% | 4.4% | 0.86 |
| Previous angina | 9% | 13% | 0.18 |
| Previous myocardial infarction | 7% | 5.7% | 0.53 |
| Previous percutaneous coronary intervention | 5.4% | 4.2% | 0.56 |
| Previous coronary artery bypass grafting | 0% | 0% | – |
| Smoker | 71% | 61% | 0.03 |
| Current | 59% | 47% | 0.02 |
| Former | 12% | 13% | 0.67 |
| Symptom onset to balloon time (minutes) | 135 [114, 159] | 305.5 [241.5, 427.5] | <0.0001 |
| Variable | Symptom Onset to Balloon Time (hours) | p-Value | |
|---|---|---|---|
| ≤3 (n = 167) | >3 (n = 264) | ||
| Aspirin | 99% | 99% | 1.00 |
| Adenosine diphosphate antagonist | 97% | 96% | 0.53 |
| Clopidogrel | 70% | 72% | 0.80 |
| Ticlopidine | 0% | 0.4% | 1.00 |
| Prasugrel | 23% | 21% | 0.65 |
| Ticagrelor | 6.2% | 7.5% | 0.60 |
| Glycoprotein IIb/IIIa receptor inhibitors | 87% | 81% | 0.12 |
| Bivalirudin | 8.4% | 14% | 0.08 |
| Target coronary artery | |||
| Left anterior descending | 37% | 42% | 0.31 |
| Left circumflex | 8.4% | 8.7% | 0.91 |
| Right | 55% | 49% | 0.29 |
| TIMI grade flow pre- percutaneous coronary intervention | |||
| 0/1 | 72% | 70% | 0.62 |
| 2 | 14% | 17% | 0.36 |
| 3 | 15% | 13% | 0.75 |
| Procedure(s) before stenting | |||
| None | 9.0% | 13% | 0.26 |
| Only aspiration | 50% | 36% | 0.004 |
| Only predilatation | 20% | 23% | 0.41 |
| Any aspiration performed | 71% | 64% | 0.12 |
| Stents implanted | |||
| Any stent | 100% | 99.6% | 1.00 |
| >1 stent | 12% | 12% | 0.94 |
| Stent Type | |||
| MGuard | 50% | 48% | 0.66 |
| Bare metal stent | 28% | 32% | 0.29 |
| Drug-eluting stent | 23% | 20% | 0.52 |
| Stent implantation without balloon predilatation | 59% | 49% | 0.04 |
Complete STR after PCI was more often achieved in patients with shorter SBT. There was no significant difference in epicardial flow (TIMI grade) after PCI between groups; however, a significant difference was found in both corrected TIMI frame counts and myocardial reperfusion (myocardial blush grade) favoring patients with shorter SBT ( Table 3 ).
| Variable | Symptoms Onset to Balloon Time (hours) | p Value | |
|---|---|---|---|
| ≤3 (n = 167) | >3 (n = 264) | ||
| ST-segment resolution | |||
| Complete (≥70%) | 59% | 47% | 0.02 |
| Partial (30–70%) | 24% | 36% | 0.01 |
| Absent (≤30%) | 21% | 22% | 0.90 |
| Median [IQR] | 78.81 [46.44, 92.74] | 66.17 [39.61, 86.75] | 0.007 |
| TIMI grade flow after PCI | |||
| 0/1 | 3.0% | 4.2% | 0.65 |
| 2 | 6.6% | 11% | 0.16 |
| 3 | 90% | 85% | 0.12 |
| Corrected TIMI frame count after PCI | 15.0 [12.0, 20.0] | 18.0 [12.0, 24.0] | 0.005 |
| Final myocardial blush grade | |||
| 0 | 0.6% | 1.9% | 0.41 |
| 1 | 9.6% | 17% | 0.03 |
| 2 | 10% | 12% | 0.53 |
| 3 | 80% | 69% | 0.01 |
| 2/3 | 90% | 81% | 0.01 |
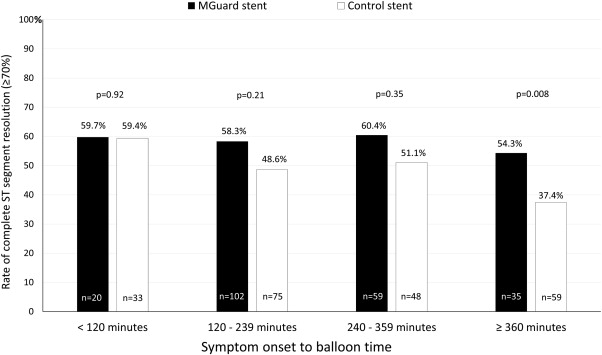
Complete STR was observed more often in patients receiving the MGuard than control stent (58% vs 45%, p = 0.008). When analyzing the effect of randomized stent type on STR according to SBT, as delay to reperfusion increased, the MGuard stent achieved relatively greater rates of STR than conventional stents ( Figure 1 ). A formal test for interaction did not reach statistical significance, however (p for interaction = 0.11). Similar relations were observed when analyzing TIMI flow grade after PCI according to stent type and SBT (p for interaction = 0.67).
The rate of clinical events was relatively low at 30 days, and no significant differences between SBT groups were found. At 1 year, mortality was lesser in patients with shorter SBT, and a trend toward fewer major adverse cardiovascular and cerebral events was also observed with shorter SBT. When results were analyzed according to stent type, a trend toward lesser mortality was found after treatment with MGuard compared with control stents at 30 days and 1 year in patients with SBT >3 hours. Conversely, no deaths through 1-year follow-up occurred with either stent in patients with SBT ≤3 hours. Higher 1-year rates of ischemia-driven target lesion revascularization and target vessel revascularization were observed in the MGuard group compared with the control stent group, regardless of SBT ( Table 4 ).
| Variable | SBT ≤3 hours (n = 167) | SBT >3 hours (n = 264) | p Value | SBT ≤3 hours | SBT >3 hours | ||||
|---|---|---|---|---|---|---|---|---|---|
| MGuard Stent (n = 86) | Control Stent (n = 81) | p Value | MGuard Stent (n = 130) | Control Stent (n = 134) | p Value | ||||
| 30 days | |||||||||
| MACCE | 1.8% | 2.7% | 0.56 | 3.5% | 0 | 0.09 | 1.5% | 3.8% | 0.26 |
| Major adverse cardiac events | 1.8% | 2.3% | 0.73 | 3.5% | 0 | 0.09 | 0.8% | 3.8% | 0.1 |
| All-cause mortality | 0 | 1.5% | 0.11 | 0 | 0 | — | 0 | 3.0% | 0.05 |
| Cardiac mortality | 0 | 1.5% | 0.11 | 0 | 0 | — | 0 | 3.0% | 0.05 |
| Reinfarction | 1.2% | 1.1% | 0.96 | 2.3% | 0 | 0.17 | 0.8% | 1.5% | 0.57 |
| TLR, ischemia-driven | 1.8% | 0.8% | 0.33 | 3.5% | 0 | 0.09 | 0.8% | 0.8% | 1 |
| TVR, ischemia-driven | 1.8% | 1.1% | 0.58 | 4.7% | 0 | 0.05 | 1.5% | 0.8% | 0.55 |
| Stent thrombosis, definite/ probable | 1.2% | 1.1% | 0.96 | 2.3% | 0 | 0.17 | 0.8% | 1.5% | 0.57 |
| Stent thrombosis, definite | 1.2% | 0.8% | 0.65 | 2.3% | 0 | 0.17 | 0.8% | 0.8% | 1 |
| Stroke | 0 | 0.4% | 0.42 | 0 | 0 | – | 0.8% | 0 | 0.32 |
| TIMI bleeding, major or minor | 1.2% | 2.7% | 0.3 | 2.3% | 0 | 0.17 | 2.3% | 3.0% | 0.73 |
| 1 year | |||||||||
| MACCE | 4.4% | 9.2% | 0.052 | 8.5% | 0 | 0.009 | 11% | 7.5% | 0.37 |
| Major adverse cardiac events | 4.4% | 7.3% | 0.19 | 8.5% | 0 | 0.009 | 9.5% | 5.3% | 0.23 |
| All-cause mortality | 0 | 3.5% | 0.02 | 0 | 0 | — | 1.6% | 5.3% | 0.1 |
| Cardiac mortality | 0 | 2.3% | 0.05 | 0 | 0 | — | 0.8% | 3.8% | 0.11 |
| Reinfarction | 1.2% | 1.1% | 0.96 | 2.3% | 0 | 0.17 | 0.8% | 1.5% | 0.57 |
| TLR, ischemia-driven | 4.4% | 5.1% | 0.68 | 8.5% | 0 | 0.009 | 8.7% | 1.5% | 0.01 |
| TVR, ischemia-driven | 5.6% | 5.9% | 0.83 | 10.5% | 0 | 0.003 | 10.3% | 1.5% | 0.003 |
| Stent thrombosis, definite/ probable | 1.2% | 1.9% | 0.57 | 2.3% | 0 | 0.17 | 2.4% | 1.5% | 0.65 |
| Stent thrombosis, definite | 1.2% | 1.6% | 0.77 | 2.3% | 0 | 0.17 | 2.4% | 0.8% | 0.31 |
| Stroke | 0 | 1.2% | 0.16 | 0 | 0 | — | 0.8% | 1.6% | 0.57 |
| TIMI bleeding, major or minor | 2.4% | 4.4% | 0.32 | 2.3% | 2.5% | 0.98 | 4.7% | 4.1% | 0.74 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


