The objectives of this study were to determine the causes and impact of anemia and hemoglobin level on functional status, physical performance, and quality of life in the preprocedural evaluation and follow-up of transcatheter aortic valve replacement (TAVR) candidates. A total of 438 patients who underwent TAVR were included. Anemia was defined as a hemoglobin level <12 g/dl in women and <13 g/dl in men. Before TAVR, anemia was encountered in 282 patients (64.4%). A potential treatable cause of anemia was detected in 90.4% of patients and was attributed to iron deficiency in 53% of them. The occurrence of anemia was an independent predictor of poorer performance in the 6-minute walk test (6MWT), a lower Duke Activity Status Index score, and Kansas City Cardiomyopathy Questionnaires overall, clinical, and social limitation scores (p <0.05 for all). A lower hemoglobin level was associated with a higher prevalence of New York Heart Association class III to IV (p <0.001) and correlated negatively with the results of all functional tests (p <0.02 for all). At follow-up, anemia was found in 62% of patients and was associated with poorer performance in the 6MWT (p = 0.023). A lower hemoglobin level after TAVR was a predictor of poorer New York Heart Association class (p = 0.020) and correlated negatively with the distance walked in the 6MWT (r = −0.191, p = 0.004) and Duke Activity Status Index score (r = −0.158, p = 0.011) at 6-month follow-up. In conclusion, anemia was very common in TAVR candidates and was attributed to iron deficiency in more than half of them. The presence of anemia and lower hemoglobin levels determined poorer functional status before and after the TAVR procedure. These results highlight the importance of implementing appropriate measures for the diagnosis and treatment of this frequent co-morbidity to improve both the accuracy of preprocedural evaluation and outcomes of TAVR candidates.
Transcatheter aortic valve replacement (TAVR) has been associated with reduced mortality and improved overall functional status and quality of life compared with medical treatment. However, a substantial proportion of patients fail to improve their functional status and quality of life after TAVR. This may, indeed, be of greater relevance than mortality in a population with limited life expectancy because of advanced age and severe co-morbidities. TAVR candidates are usually elderly subjects with several co-morbid conditions, including the presence of anemia in up to 50% of these patients. Nonetheless, the impact of hemoglobin levels and anemia on functional status and quality of life in patients who underwent TAVR is unknown. Furthermore, the causes of anemia and its potential treatment in TAVR candidates have not been elucidated to date. Thus, the aims of this study were to determine the causes of anemia in TAVR candidates (with special focus on potentially treatable causes) and to evaluate the impact of the presence of anemia; hemoglobin level; and its changes on functional status, physical performance, and quality of life before the procedure and at follow-up in TAVR candidates.
Methods
The study included a total of 438 consecutive patients who underwent TAVR from May 2007 to December 2013 at a single institution. All patients were considered eligible for TAVR as evaluated by the Heart Team. TAVR procedures have been described elsewhere. Data were prospectively collected and entered into a dedicated database. Clinical outcomes were defined according to the definitions of the Valve Academic Research Consortium-2.
Blood samples were obtained, and hemoglobin levels were determined within 2 weeks before TAVR (all patients), daily during at least 72 hours after the procedure (all patients alive), at hospital discharge (all patients at risk), and at 6-month follow-up in 77% of the patients at risk (because of logistic reasons). Anemia was diagnosed according to the definition of the World Health Organization as an hemoglobin <12 g/dl in women and <13 g/dl in men. Since December 2011, the causes of anemia were systematically assessed in TAVR candidates. The following parameters were analyzed: serum ferritin, serum iron, transferrin saturation, estimated glomerular filtration rate (eGFR), creatinine, vitamin B12, and folic acid. The cause of anemia was classified according to the Network for Advancement of Transfusion Alternatives guidelines and the recommendations for the evaluation of anemia in elderly population. Iron deficiency was confirmed if serum ferritin was <30 μg/L and/or transferrin saturation was <20%. If serum ferritin was 30 to 100 μg/L and/or transferrin saturation <20%, anemia was attributed to possible iron deficiency. In patients with normal iron parameters and eGFR <60 ml/min, anemia was attributed to chronic renal failure. Anemia was associated with deficiency of vitamin B12 or folic acid in patients with normal iron parameters, eGFR >60 ml/min and vitamin B12 <145 pmol/L or folic acid <9.5 nmol/L, according to the local laboratory cutoff. All other anemic patients were classified as having unexplained anemia. No specific recommendations were given regarding therapeutic strategies for patients with newly diagnosed anemia at baseline or hospital discharge.
Functional status and quality of life outcomes were assessed by means of the New York Heart Association (NYHA) class, the 6-minute walk test (6MWT), the Duke Activity Status Index (DASI) score, and the Kansas City Cardiomyopathy Questionnaire (KCCQ) overall summary, clinical summary, physical limitation, total symptoms, self-efficacy, quality of life, and social limitation scores. All tests and questionnaires were administered by trained personnel and/or physicians. Evaluations were performed within 2 weeks before the TAVR procedure and at 6-month follow-up. NYHA class was assessed in all patients before TAVR and at 6-month follow-up. The 6MWT was performed according to the American Thoracic Society protocol. The 6MWT was performed in 379 (87%) and 246 patients (83% of patients at risk) at baseline and at follow-up, respectively. Overall, 110 tests were not performed for logistic reasons (n = 81) or because of severely limited mobility of noncardiac origin (n = 29). Missing values attributable to the inability of patients to perform the test because of current heart failure with NYHA class IV or recent myocardial infarction were imputed as 0 and included in the analyses. The DASI questionnaires were obtained pre-TAVR and at 6-month follow-up in 420 (96%) and in 275 patients (93% of patients at risk), respectively. Beginning in March 2012, the KCCQ scores were systematically obtained and were completed in 163 patients before TAVR and in 112 patients (100% of patients at risk) at follow-up.
Qualitative variables are expressed as counts and percentage and compared with chi-square or Fisher’s exact tests as appropriate. Quantitative variables are displayed as means ± SD or median (25th to 75th percentiles) and compared with 2-sided t tests or Wilcoxon rank-sum test according to variable distribution. Skewed variables were log-transformed to fit normal distribution. Differences in number of red cell packets between study groups were analyzed using the Poisson regression model.
Analysis of covariance was used for analysis of the impact of anemia on functional and quality of life measures. Variables with p value <0.10 in the univariate analysis were included in the multivariate analysis. Baseline differences were included in the models as covariates. When assessing the impact of anemia on functional and quality of life assessment at the 6-month follow-up, procedural and 30-day outcome differences and values at baseline were also included. The association between hemoglobin levels and study measures was assessed by means of bivariate and partial correlation after adjusting for univariate predictors. A repeated-measures model was conducted to assess the changes in hemoglobin level over time. A repeated-measures model was also used to analyze the interaction between delta hemoglobin and changes in quality of life measures between baseline and 6-month follow-up. Thirty-day outcomes were assessed by means of logistic regression models. Kaplan-Meier estimates and Cox regression models were used for univariate and multivariate analyses, respectively, assessing the impact of anemia and need for blood transfusion on cumulative mortality. Further comparisons were performed using the Bonferroni adjustment for multiple testing. The results were considered significant with p values <0.05. Analyses were conducted using the statistical package SAS, version 9.2 (SAS Institute Inc., Cary, North Carolina).
Results
Before the TAVR procedure, 282 patients (64.4%) were classified as anemic with a mean hemoglobin level of 10.8 ± 1.1 g/dl versus 13.4 ± 1.0 g/dl in the no-anemia group, p <0.001. Of them, 52 patients (11.9%) had a hemoglobin level <10 g/dl. Baseline clinical and echocardiographic characteristics for overall population and according to the presence of anemia at baseline are listed in Table 1 .
| Variable | All patients (n=438) | Anemia (n=282) | No anemia (n=156) | p value |
|---|---|---|---|---|
| Age (years) | 79 ± 8 | 80 ± 8 | 78 ± 9 | 0.020 |
| Male | 214 (48.9%) | 146 (51.8%) | 68 (43.6%) | 0.101 |
| Body mass index (kg/m 2 ) | 27 ± 5 | 27 ± 5 | 27 ± 5 | 0.257 |
| Hypertension | 384 (87.7%) | 248 (87.9%) | 136 (87.2%) | 0.816 |
| Diabetes mellitus | 152 (34.7%) | 112 (39.7%) | 40 (25.6%) | 0.003 |
| Chronic obstructive pulmonary disease | 125 (28.5%) | 84 (29.8%) | 41 (26.3%) | 0.437 |
| Prior pacemaker | 73 (17.4%) | 49 (17.4%) | 24 (15.4%) | 0.592 |
| Atrial fibrillation | 136 (31.1%) | 94 (33.3%) | 42 (26.9%) | 0.165 |
| Malignancy | 92 (21.35%) | 60 (21.7%) | 32 (20.6%) | 0.790 |
| Coronary artery disease ∗ | 291 (66.4%) | 193 (68.4%) | 98 (62.8%) | 0.233 |
| Coronary artery bypass grafting | 165 (37.7%) | 106 (37.6%) | 59 (37.8%) | 0.962 |
| Prior cardiac surgery | 152 (34.7%) | 97 (34.4%) | 55 (35.3%) | 0.831 |
| Severely calcified aorta | 105 (23.8%) | 62 (21.9%) | 43 (27.6%) | 0.197 |
| Frailty (eye-ball test) | 119 (27.2%) | 82 (29.1%) | 37 (23.7%) | 0.227 |
| Estimated glomerular filtration rate (ml/min) | 58.5 ± 23.0 | 55.0 ± 22.7 | 64.7 ±22.4 | <0.001 |
| STS-PROM score (%) | 7.2 ± 4.8 | 7.9 ± 5.2 | 5.9± 3.5 | <0.001 |
| Echocardiography | ||||
| Left ventricular ejection fraction ≤40% | 72 (16.4%) | 54 (19.1%) | 18 (11.5%) | 0.040 |
| Peak pressure gradient (mmHg) | 67 ± 25 | 68 ± 25 | 67 ± 25 | 0.698 |
| Mean transaortic valve gradient (mmHg) | 41 ± 16 | 40 ± 16 | 41 ± 16 | 0.960 |
| Aortic valve area (cm 2 ) | 0.64 (0.50-0.80) | 0.63 (0.50-0.79) | 0.64 (0.52-0.80) | 0.430 |
| Systolic pulmonary artery pressure >60 mmHg | 39 (8.9%) | 29 (10.3%) | 10 (6.4%) | 0.173 |
∗ Coronary artery disease was defined as: the presence of coronary lesion(s) with a diameter of stenosis ≥50% or prior coronary revascularization (PCI or CABG) irrespective of the presence of lesions.
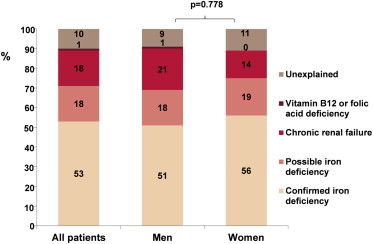
A systematic analysis of the causes of anemia was performed in 114 anemic patients. A potentially correctable cause of anemia was diagnosed in 103 patients (90.4%; Figure 1 ). Iron deficiency anemia was confirmed in 60 patients (52.6%), and 21 patients (18.4%) were diagnosed with a possible iron deficiency. The mean/median serum iron, serum ferritin, and transferrin saturation levels in patients with iron deficiency anemia were 7.4 ± 2.5 μmol/L, 68.0 μg/L (40.5 to 154.0), and 13 ± 4%, respectively. Eleven patients (13.6% of those with confirmed or possible iron deficiency) had overt bleeding events (gastrointestinal bleeding in 6 patients, hemoptysis in 2 patients, intracranial bleeding in 2 patients, and peripheral hematoma in 1 patient). In the 60 patients with iron deficiency, only 8 patients (13.3%) were receiving oral iron supplements before the TAVR procedure. In 21 patients (18.4%), anemia was associated with chronic renal failure and 1 patient (0.9%) had a vitamin B12 deficiency. In the remaining 11 patients (9.6%), anemia was considered of unexplained cause ( Figure 1 ).
Results of functional status, physical performance, and quality of life assessment at baseline according to the occurrence of anemia before TAVR are listed in Table 2 . Associations between hemoglobin level at the baseline and functional outcomes are listed in Table 3 and Supplementary Table 1 .
| Variable | All patients | Anemia | No anemia | p value | Adjusted ∗ Odds Ratio (95%CI)/Mean difference (95% CI) | p value |
|---|---|---|---|---|---|---|
| NYHA class III or IV | ||||||
| Patients evaluated | 438 | 282 | 156 | |||
| Number of patients | 331 (75.6%) | 226 (80.1%) | 105 (67.3%) | 0.003 | 1.57 (0.98-2.53) | 0.063 |
| 6-Minute Walk Test | ||||||
| Patients evaluated | 379 | 242 | 137 | |||
| Distance (meters) | 186.8 ± 121.6 | 167.8 ± 120.5 | 220.5 ±116.5 | <0.001 | – 30.39 (-55.64 to -5.15) | 0.018 |
| Duke Activity Status Index | ||||||
| Patients evaluated | 420 | 268 | 152 | |||
| Score | 17.8 ± 11.2 | 12.5± 8.8 | 14.8 ± 9.5 | 0.006 | -0.06 (-0.12 to -0.01) | 0.034 |
| Kansas City Cardiomyopathy Questionnaire | ||||||
| Patients evaluated | 163 | 100 | 63 | |||
| Overall summary | 47.8 ± 19.2 | 44.6 ± 19.3 | 52.5 ± 19.1 | 0.011 | -8.38 (-14.98 to -1.78) | 0.013 |
| Clinical summary | 64.3 ± 21.5 | 58.3 ± 22.3 | 66.8 ± 21.3 | 0.017 | -7.94 (-15.59 to -0.29) | 0.042 |
| Physical limitation | 59.3 ± 23.8 | 54.3 ± 26.9 | 62.6 ± 27.2 | 0.030 | -7.87 (-16.51 to 0.76) | 0.074 |
| Symptoms | 67.6 ± 20.4 | 65.0 ± 21.3 | 69.3 ± 20.9 | 0.202 | -4.42 (-11.82 to 2.97) | 0.239 |
| Self-efficacy | 63.7 ± 29.9 | 59.8 ± 31.0 | 66.9 ± 27.2 | 0.137 | -7.35 (-17.94 to 3.24) | 0.172 |
| Quality of life | 47.1 ± 22.9 | 43.8 ± 23.3 | 51.6 ± 21.8 | 0.035 | -7.12 (-15.07 to 0.82) | 0.078 |
| Social limitation | 56.3 ± 28.8 | 58.3 ± 22.3 | 66.9 ± 27.6 | 0.015 | -12.67 (-22.84 to -2.50) | 0.015 |
∗ Adjusted for baseline differences: Age, diabetes, estimated glomerular filtration rate, left ventricular ejection fraction<40% and STS-PROM score.
| Variable | Odds Ratio (95% CI)/ Pearson’s Correlation Coefficient | p value | Adjusted ∗ Odds Ratio (95%CI)/Correlation Coefficient | p value |
|---|---|---|---|---|
| NYHA class III or IV | 0.97 (0.95-0.98) | <0.001 | 0.97 (0.96-0.99) † | <0.001 |
| 6-Minute Walk Test | 0.307 | <0.001 | 0.207 ‡ | <0.001 |
| Duke Activity Status Index | 0.215 | <0.001 | 0.151 § | 0.003 |
| Kansas City Cardiomyopathy Questionnaire | ||||
| Overall summary | 0.278 | <0.001 | 0.253 ‖ | 0.002 |
| Clinical summary | 0.266 | 0.001 | 0.252 ¶ | 0.002 |
| Physical limitation | 0.257 | 0.001 | 0.239 # | 0.004 |
| Symptoms | 0.183 | 0.019 | 0.186 ∗∗ | 0.021 |
| Self-efficacy | 0.200 | 0.010 | 0.203 †† | 0.011 |
| Quality of life | 0.169 | 0.031 | 0.168 ‡‡ | 0.038 |
| Social limitation | 0.223 | 0.005 | 0.187 §§ | 0.025 |
∗ Adjusted for univariate predictors with p<0.10 ( Supplementary Table 1 ).
† Adjusted for: age, chronic obstructive pulmonary disease, prior pacemaker, history of atrial fibrillation, history of malignancy, porcelain aorta, STS-PROM score, aortic valve area, systolic pulmonary artery pressure>60mmHg.
‡ Adjusted for: age, gender, history of atrial fibrillation, coronary artery bypass grafting, prior cardiac surgery, frailty, estimated glomerular filtration rate, STS-PROM score, mean aortic transvalvular gradient, aortic valve area, systolic pulmonary artery pressure>60mmHg.
§ Adjusted for: age, gender, history of atrial fibrillation, prior cardiac surgery, frailty, STS-PROM score, aortic valve area, systolic pulmonary artery pressure>60mmHg.
¶ Adjusted for: body mass index, chronic obstructive pulmonary disease, history of atrial fibrillation, frailty, STS-PROM score, aortic valve area, systolic pulmonary artery pressure>60mmHg.
‖ Adjusted for: body mass index, frailty, STS-PROM score, aortic valve area.
# Adjusted for: body mass index, chronic obstructive pulmonary disease, STS-PROM score, aortic valve area, systolic pulmonary artery pressure>60mmHg.
∗∗ Adjusted for: body mass index, chronic obstructive pulmonary disease, history of atrial fibrillation, aortic valve area.
†† Adjusted for: history of atrial fibrillation, frailty, aortic valve area.
‡‡ Adjusted for: body mass index, chronic obstructive pulmonary disease, frailty, aortic valve area.
§§ Adjusted for: age, body mass index, frailty, STS-PROM score, aortic valve area, systolic pulmonary artery pressure>60mmHg.
Procedural characteristics and 30-day outcomes according to the presence of baseline anemia are listed in Supplementary Table 2 . Anemic patients were more frequently transfused (39.7% vs 20.0%, p <0.001) and required a higher number of red cell packets (3.4 ± 2.9 vs 2.4 ± 1.8, p <0.001). The need for blood transfusion was independently associated with an increased risk of 30-day acute kidney injury (OR 2.46; 95% CI 1.31 to 4.63, p = 0.005), 30-day mortality (OR 3.98; 95% CI 1.51 to 10.47, p = 0.005), and cumulative mortality at 6-month follow-up (HR 1.88; 95% CI 1.03 to 3.45, p = 0.040; Supplementary Tables 3 and 4 ).
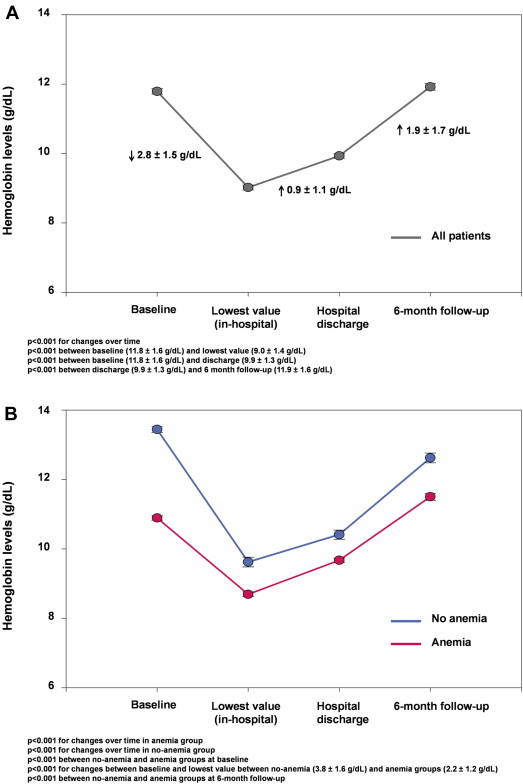
Changes in hemoglobin levels over time, overall and according to the presence of anemia before TAVR are showed in Figure 2 . Up to 391 patients (96.1% of the population at risk) were discharged with some degree of anemia. A total of 217 patients (53.3% of patients at risk) had a hemoglobin level <10 g/dl at hospital discharge, and 162 patients (41.4% of patients at risk) received oral iron therapy (oral ferrous sulfate, 300 mg/day) at hospital discharge. At 6-month follow-up, a total of 52 patients (11.9%) had died. An increased risk of mortality was observed in patients with severe anemia at baseline but not in the entire anemia group (p = 0.005 and p = 0.642, respectively; Figure 3 ). An assessment of the hemoglobin level was performed in 297 patients at 6-month follow-up (77% of the patients at risk). Of them, 183 patients (61.6%) were anemic, and 29 (9.8%) had a hemoglobin level <10 g/dl. Baseline characteristics, procedural findings, and 30-day outcomes according to the presence of anemia at follow-up are listed in Supplementary Table 5 . Results of functional outcomes after TAVR according to the occurrence of anemia at 6-month follow-up are listed in Table 4 . A lower hemoglobin level was a predictor of NYHA class III or IV (OR 1.03; 95% CI 1.01 to 1.06; p = 0.020) and independently correlated (negatively) with the distance covered in the 6MWT (r = −0.191, p = 0.004) and DASI score (r = −0.191, p = 0.011). No differences were encountered in KCCQ scores between groups (p >0.10 for all; Supplementary Tables 6 and 7 ).