Brain natriuretic peptide (BNP) levels are lower in obese patients with left ventricular failure than in their comparably ill, leaner counterparts. The effect of obesity on BNP in patients with pulmonary arterial hypertension (PAH) is unknown. We reviewed our prospective PAH registry data collected from November 2001 to December 2007 for patients undergoing right heart catheterization who met the criteria for PAH and had the BNP level and body mass index determined at baseline. The median BNP level for the lean, overweight, and obese patients was 285 pg/ml (interquartile range 131 to 548), 315 pg/ml (interquartile range 88 to 531), and 117 pg/ml (interquartile range 58 to 270), respectively (p = 0.029). A greater body mass index was associated with a lower BNP level, adjusted for age, gender, New York Heart Association functional class, hypertension, coronary artery disease, and mean right atrial and pulmonary arterial pressures (p <0.001). No statistically significant differences were found among the groups in age, race, medical co-morbidities, underlying etiology of PAH, use of vasoactive medications, New York Heart Association functional class, echocardiographic parameters, or pulmonary function. Obese patients had greater right atrial and pulmonary artery pressures. Increased BNP was associated with worse survival in the lean and overweight patients only. In conclusion, the BNP levels are attenuated in obese patients with PAH despite similar or worse hemodynamics or functional class compared to lean or overweight patients and should therefore be interpreted with caution.
Increased plasma brain natriuretic peptide (BNP) levels are associated with greater hemodynamic impairment, poorer functional capacity, and reduced survival in patients with idiopathic pulmonary arterial hypertension (PAH). BNP correlates with the degree of right ventricular overload and dysfunction in patients with PAH. Thus, BNP has assumed an increasingly important clinical role in the evaluation of patients with PAH. Compared to leaner subjects, BNP levels are attenuated in obese subjects with left ventricular dysfunction, even in the presence of heart failure symptoms and increased left ventricular filling pressure. Nonetheless, in patients with left-sided heart failure, BNP remains a clinically useful predictor of exercise intolerance, hemodynamic impairment, and mortality at all levels of body mass index (BMI), although lower cutpoints appear necessary for patients with an elevated BMI. Whether a similar interaction between BNP and obesity occurs in subjects with PAH is not known. The present study investigated the relation between BNP and BMI in patients with PAH.
Methods
We reviewed a large, single-center, prospectively collected database of consecutive patients undergoing right-sided heart catheterization for evaluation of PAH from November 2001 to December 2007. Patients <18 years old, those with a diagnosis of heart failure, and those requiring dialysis were excluded. Of the 530 patients undergoing right-sided heart catheterization, 380 did not have PAH, 42 patients not have the baseline BNP measured, and 4 did not have the baseline BMI determined and were excluded, leaving a study population of 104 patients with World Health Organization category I PAH. Heart failure and PAH were defined according to the established guidelines.
We reviewed our institutional review board-approved registry for demographics, medical history, PAH classification, pulmonary vasodilator medication use, New York Heart Association (NYHA) functional class, 6-minute walk distance, serum BNP (using the Biosite assay), blood urea nitrogen, serum creatinine, pulmonary function test data, transthoracic echocardiographic data, hemodynamic data, and Social Security Death Index data. Coronary artery disease, hyperlipidemia, and hypertension were defined according to established guidelines. The included data were within 2 months of the diagnostic right-sided heart catheterization. Data were missing for the following variables: echocardiography (2% missing), creatinine (0.9% missing), NYHA functional class (0.9% missing), 6-minute walk test (16% missing). All patients had the hemodynamic data measured; however, 14% had ≥1 variable obtained using right-sided heart catheterization missing.
Patients were grouped according to their BMI as lean (<25.0 kg/m 2 ), overweight (25.0 to 29.9 kg/m 2 ), or obese (≥30.0 kg/m 2 ). The quantitative variables are summarized within the BMI group as the mean ± SD, except for the BNP levels, for which the median and interquartile range are reported. The quantitative variables were compared using the Kruskal-Wallis test and the categorical variables using chi-square tests. Within the BMI groups, comparisons with respect to dichotomized patient characteristics were performed with Wilcoxon rank sum tests. Multivariate linear regression analysis of continuous log-transformed BNP versus obesity and covariates reflective of disease severity was performed. Cox regression analysis using backward stepwise elimination of variables with Wald p >0.10 as a removal criterion was used to determine the relation of BNP in its log-transformed form to survival. Receiver operating characteristic curves were used to assess the associations between BNP and 2-year survival, with the optimal BNP cutoff values estimated within each BMI group. These cutoffs were then applied to an analysis of overall survival using Kaplan-Meier curves and log–rank tests for comparison. A Cox regression model of survival with respect to log 2 BNP, BMI, and their interaction was used to evaluate the strength of the relation between BNP and survival for the different BMI values.
Survival was estimated from the date of right heart catheterization until cardiopulmonary death or until September 2009 using the patient medical records, pulmonary hypertension database, and the Social Security Death Index. None of the 104 patients included in the present study received a lung or a heart-lung transplant during the study period.
Results
The mean age of the study population at the baseline diagnostic right heart catheterization was 51 ± 3 years; 85% were women, 85% were European American, and 14% were African American. The etiology of PAH was idiopathic in 48%, connective tissue disease in 27%, portal hypertension in 13%, congenital heart disease in 10%, human immunodeficiency virus related in 1, and drug related in 1. The medications used included prostanoids (50%), endothelin receptor blockers (23%), phosphodiesterase V inhibitors (20%), 11% were not taking pulmonary vasoactive medications, and 5% were receiving combination therapy. The patient characteristics according to the BMI groups are listed in Table 1 . No statistically significant differences were found between groups in terms of age, race, medical co-morbidities, underlying PAH etiology, use of vasoactive medications, NYHA functional class, echocardiographic parameters studied, or pulmonary function. Obese patients had greater right atrial and mean pulmonary artery pressures.
| Variable | BMI (kg/m 2 ) | |||
|---|---|---|---|---|
| <25 (n = 26) | 25–30 (n = 38) | >30 (n = 40) | p Value | |
| Age (years) | 51 ± 3 | 56 ± 2 | 55 ± 2 | 0.44 |
| Women | 85% | 60% | 82% | 0.038 |
| Coronary artery disease | 8% | 3% | 10% | 0.47 |
| Diabetes mellitus | 4% | 13% | 18% | 0.29 |
| Hyperlipidemia | 8% | 18% | 10% | 0.42 |
| Hypertension | 35% | 45% | 43% | 0.71 |
| Chronic kidney disease | 8% | 10% | 0 | 0.10 |
| Smoker | 50% | 55% | 38% | 0.27 |
| Medication | ||||
| Prostanoids | 50% | 40% | 60% | 0.19 |
| Endothelin receptor blockers | 27% | 28.9% | 15% | 0.30 |
| Phosphodiesterase V inhibitors | 19% | 24% | 18% | 0.79 |
| No vasodilators | 4% | 16% | 12% | 0.34 |
| Combination | 4% | 8% | 3% | 0.53 |
| New York Heart Association functional class | 3.1 ± 0.1 | 3.1 ± 0.1 | 3.2 ± 0.1 | 0.83 |
| Six-minute walk distance (m) | 312 ± 28 | 303 ± 22 | 272 ± 17 | 0.40 |
| Hemodynamics | ||||
| Mean right atrial pressure (mm Hg) | 9 ± 1 | 9 ± 1 | 12 ± 1 | 0.05 |
| Mean pulmonary artery pressure (mm Hg) | 51 ± 3 | 44 ± 2 | 52 ± 2 | 0.017 |
| Pulmonary vascular resistance (Wood units) | 12 ± 1 | 10 ± 1 | 10 ± 1 | 0.5 |
| Pulmonary capillary wedge pressure (mm Hg) | 8.7 ± 0.8 | 9.5 ± 0.5 | 10 ± 0.6 | 0.13 |
| Cardiac index (L/min/m 2 ) | 2.3 ± 0.1 | 2.4 ± 0.1 | 2.5 ± 0.2 | 0.76 |
| Ejection fraction (%) | 55 ± 1 | 57 ± 1 | 56 ± 1 | 0.35 |
| Right ventricular systolic pressure (mm Hg) | 86 ± 6 | 78 ± 4 | 82 ± 3 | 0.30 |
| Pericardial effusion | 29% | 26% | 18% | 0.57 |
| Forced expiratory lung volume in 1 s (L) | 2.1 ± 0.1 | 2.2 ± 0.1 | 2.0 ± 0.1 | 0.76 |
| Carbon monoxide diffusion capacity | 12 ± 2 | 15 ± 2 | 15 ± 2 | 0.62 |
| Blood urea nitrogen (mg/dl) | 22 ± 2 | 20 ± 2 | 19 ± 1 | 0.17 |
| Creatinine (mg/dl) | 1.0 ± 0.2 | 1.0 ± 0.1 | 0.9 ± 0.1 | 0.82 |
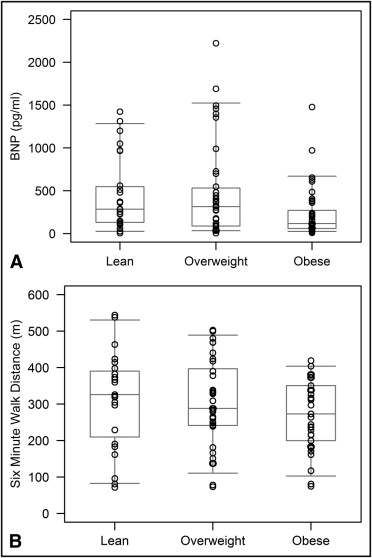
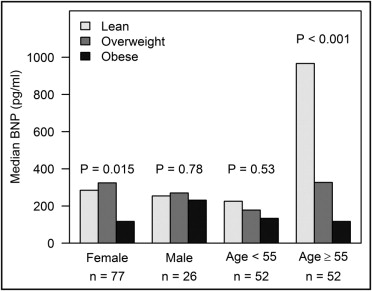
The plasma BNP was significantly lower in obese patients with PAH compared to that in the overweight or lean patients. The median value for lean, overweight, and obese patients was 285 pg/ml (interquartile range 131 to 548), 315 pg/ml (interquartile range 88 to 531), 117 pg/ml (interquartile range 58 to 270), respectively (p = 0.029). This was true despite a 6-minute walk distance that was not significantly different among the BMI categories (p = 0.40; Figure 1 ). The degree of BNP attenuation among obese subjects was more pronounced in patients aged ≥55 years (p <0.001) and in women (p = 0.015; Figure 2 ).
Univariate analysis of log-transformed BNP versus BMI was performed and demonstrated that a greater BMI was associated with a lower BNP (p = 0.011). This association was maintained with covariate adjustment for age, gender, NYHA class, hypertension, coronary artery disease, and mean right atrial and pulmonary arterial pressures (p <0.001).
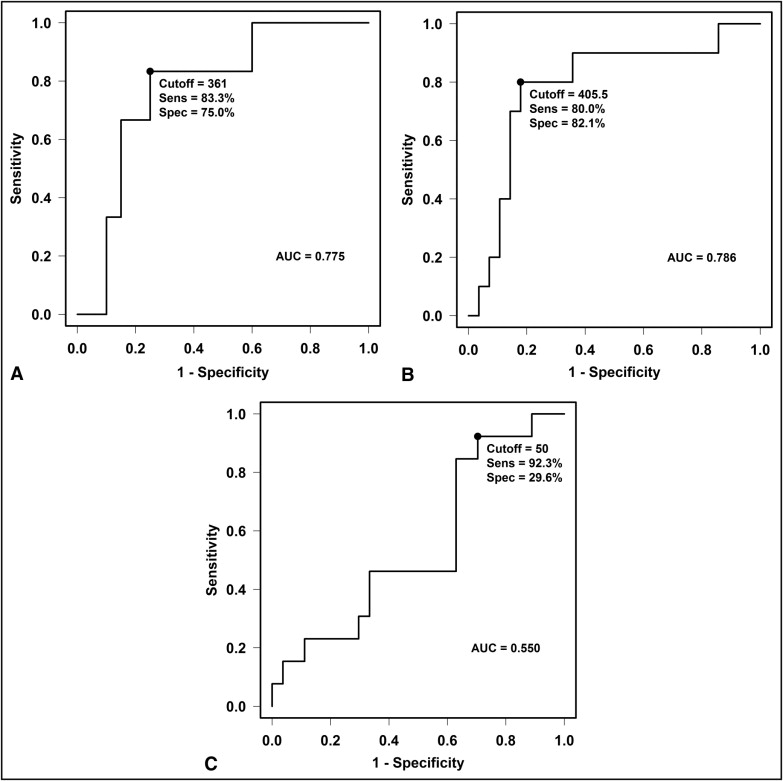
The patients were followed up for a mean of 3.0 ± 0.2 years. During follow-up, 49 patients died: 25 by 1 year and 32 by 2 years. The mean survival rate was not significantly different statistically among the BMI groups (log-rank p = 0.10), with a 2-year survival rate of 77% for lean patients, 66% for overweight patients, and 68% for obese patients. In the study population, BNP was significantly associated with survival, independent of age, BMI, creatinine, and presence of a pericardial effusion on transthoracic echocardiography (p = 0.01). Receiver operating characteristic analysis was performed in each BMI group and revealed an optimal cutoff of 361 pg/ml for lean patients, 406 pg/ml for overweight patients, and 50 pg/ml for obese patients ( Figure 3 ). However, in obese patients, the area under the curve was only 0.55, suggesting that the BNP level might not be a useful prognostic indicator in obese patients with PAH. These values were then used to construct the Kaplan-Meier curves ( Figure 4 ). The strength of the association of BNP and survival gradually weakened as the BMI increased, and, in patients with a BMI of ≥35 kg/m 2 , this relation was lost ( Figure 5 ).