New-onset conduction disturbances are common after transcatheter aortic valve implantation (TAVI). The most common complication is left bundle branch block (LBBB). The clinical impact of new-onset LBBB after TAVI remains controversial. The aim of this study was to analyze the clinical impact of new-onset LBBB in terms of mortality and morbidity (need for pacemakers and admissions for heart failure) at long-term follow-up. From April 2008 to December 2014, 220 patients who had severe aortic stenosis were treated with the implantation of a CoreValve prosthesis. Sixty-seven of these patients were excluded from the analysis, including 22 patients with pre-existing LBBB and 45 with a permanent pacemaker, implanted previously or within 72 hours of implantation. The remaining 153 patients were divided into 2 groups: group 1 (n = 80), those with persistent new-onset LBBB, and group 2 (n = 73), those without conduction disturbances after treatment. Both groups were followed up at 1 month, 6 months, 12 months, and yearly thereafter. Persistent new-onset LBBB occurred in 80 patients (36%) immediately after TAVI; 73 patients (33%) did not develop conduction disturbances. The mean follow-up time of both groups was 32 ± 22 months (range 3 to 82 months), and there were no differences in time between the groups. There were no differences in mortality between the groups (39% vs 48%, p = 0.58). No differences were observed between the groups in re-hospitalizations for heart failure (11% vs 16%, p = 0.55). Group 1 did not require pacemaker implantation more often at follow-up (10% vs 13%, p = 0.38) than group 2. In conclusion, new-onset LBBB was not associated with a higher incidence of late need for a permanent pacemaker after CoreValve implantation. In addition, it was not associated with a higher risk of late mortality or re-hospitalization.
This study analyzes the clinical outcome of patients with persistent new-onset left bundle branch block (LBBB) after CoreValve implantation compared with those who did not develop this persistent conduction disturbance.
Methods
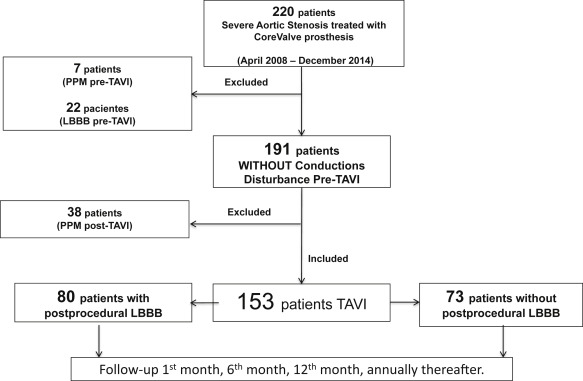
This prospective longitudinal study was conducted at a single center. The study population consisted of 220 patients who had severe degenerative aortic stenosis and underwent Medtronic CoreValve implantation from April 2008 to December 2014. Of these 220 patients, 67 were excluded from the analysis as follows: 7 patients previously had a permanent pacemaker (PPM), 22 patients had LBBB before TAVI, and 38 patients (17%) required PPM implantation within the first 72 hours after TAVI. Therefore, the final study population consisted of 153 patients. They were divided into 2 groups: group 1 comprised 80 patients (36%), who had persistent new-onset LBBB after implantation, and group 2 comprised 73 patients (33%), who did not have this conduction disorder after TAVI ( Figure 1 ). All 153 patients were followed up after TAVI at the outpatient clinic at 1 month, 6 months, 12 months, and yearly thereafter. Significant events during follow-up, including admission for heart failure and the subsequent need of a pacemaker, were prospectively collected in a dedicated database. Periprocedural events were defined according to the Valve Academic Research Consensus 2 criteria. We considered the need of a PPM at follow-up under the following circumstances: (1) when the patient developed some degree of new-onset advanced atrioventricular block (AVB) (third- or second-degree Mobitz 2 AVB) and (2) when the patient had severe disturbance of atrioventricular or intraventricular conduction and presented with a syncopal episode. The prophylactic implantation of a PPM was not considered in patients with new-onset isolated LBBB or LBBB associated with first-degree AVB, unless the patient had persistent severe bradycardia (<40 beats/min) with or without symptoms.
All patients had surface electrocardiograms with 12 leads before the procedure, at 24 hours after TAVI, at discharge, and at each follow-up review. All patients had continuous electrocardiogram monitoring during hospitalization. A new surface electrocardiogram was performed to record novel conduction disturbances produced at any time during admission (hemiblocks, right bundle branch block, LBBB, or first-, second-, or third-degree AVB). The presence of these conduction abnormalities was defined according to the diagnostic criteria for the standardization and interpretation of the surface electrocardiogram recommended by the American Heart Association.
New-onset LBBB was defined as LBBB that first appeared after TAVI and persisted at discharge. In this group of 220 patients, 14 patients (9%) developed a transient LBBB that resolved before discharge. They were not considered to have “persistent” or definitive LBBB.
Transthoracic echocardiography was performed in all patients with the same echocardiograph (Philips iE33) to assess valvular function and estimate left ventricular ejection fraction (LVEF). This was determined using 2-dimensional echocardiography by the Simpson biplane method in the apical 2- and 4-chamber views. The calculation of LVEF for both intervention groups was conducted at baseline, at discharge, 1 year after TAVI, after 3 and 5 years of follow-up, and whenever symptoms appeared.
The primary end points were the incidence of major clinical events in both groups and the time to their occurrence. The major clinical events were (1) all-cause mortality, (2) admission for heart failure, and (3) need of a PPM. The secondary end points of this study were changes in LVEF in both groups of patients, from baseline to long-term follow-up.
Continuous variables with normal distributions are presented as the mean ± SD and compared by Student’s unpaired t test for comparisons between groups. Variables that did not follow a normal distribution were compared with a Mann-Whitney U test for comparisons between groups. Categorical variables were presented as counts and percentages and were compared with a chi-square test or Fisher’s exact test, as appropriate. The cumulative incidences of clinical events at follow-up were assessed by the Kaplan-Meier method and long-rank test. The results obtained with a value of p <0.05 were accepted as statistically significant. All data were processed with the Statistical Package for Social Sciences, version 18.
Results
Table 1 lists the baseline clinical, electrocardiographic, echocardiographic, and periprocedural data for both groups. There were no statistically significant differences between the groups in terms of residual gradient, depth of valve implantation, or femoral complications after aortic valve implantation. There were no differences in the development of mitral or periprosthetic aortic regurgitation after TAVI. The only difference between groups was the width of the QRS interval post-TAVI, which was significantly longer in patients with new-onset LBBB. The procedure was considered successful in all patients.
| Variable | LBBB afer TAVI | |
|---|---|---|
| Yes (N = 80) | No (N=73) | |
| Age (years) | 78±5 | 77±6 |
| Women | 44 (55%) | 30 (41%) |
| Euroscore Log % | 15.2±8.7 | 17.6±13.3 |
| STS score % | 9.5±11 | 12.0±11 |
| Hypertension | 50 (60%) | 34 (47%) |
| Diabetes mellitus | 21 (26%) | 19 (26%) |
| Dyslipidemia | 35 (44%) | 32 (44%) |
| Dyspnea FC III-IV | 67 (83%) | 52 (71%) |
| Angina pectoris FC III-IV | 22 (28%) | 18 (25%) |
| Syncope | 7 (9%) | 4 (5%) |
| LVEF (%) | 58±15 | 56±13 |
| Peak Gradient postTAVI (mmHg) | 2.3±4.0 | 2.3±4.2 |
| PR interval widht postTAVI (msec) | 199±61 | 190±54 |
| QRS width postTAVI (msec) | 138±13 ∗ | 106±22 ∗ |
The mean follow-up time was 32 ± 22 months (range 1 to 82 months). Twenty-nine patients (19%) were followed up for >54 months, 58 patients (38%) were followed up between 27 and 54 months, and 66 patients (43%) were followed up for <27 months.
Of the 153 patients included in the study, only 6 patients died of cardiovascular causes during follow-up. One patient died 40 days after TAVI due to dissection of the ascending aorta. One patient died due to acute myocardial infarction within 72 hours after TAVI. One patient died from an arrhythmic storm, 6 hours after the procedure. Two patients died of heart failure after 5 and 22 months of follow-up. One patient died suddenly at 1 month of follow-up. He had new-onset LBBB at discharge. The remaining causes of death were mainly respiratory infections, neoplastic processes, hip fractures, hemorrhagic stroke, or pancreatitis. The probability of survival between the 2 groups was compared, and mortality among the patients with persistent new-onset LBBB did not differ from that among those in group 2, at 60 months of follow-up (61% vs 52%, log-rank p = 0.58; Figure 2 ).
No significant differences were found at 60 months of follow-up in terms of re-admissions for heart failure (11% vs 16%, log-rank p = 0.43; Figure 3 ). In 80% of cases (n = 21), admission for heart failure was due to a paroxysmal or persistent atrial fibrillation. No statistically significant differences were observed in mitral or periprosthetic aortic regurgitation after implantation, as possible factors that may favor re-admission for heart failure after TAVI. No significant difference was observed in the need for PPM at 60 months of follow-up in both intervention groups (13% vs 10%, log-rank p = 0.99; Figure 4 ). In group 1, 7 patients required PPM implantation at follow-up (7 ± 7 months). Two of them required implantation in the first month of follow-up because of the development of sinus node dysfunction associated with syncopal episodes. In the remaining 5 patients, admission was because of the development of complete AVB at different time points of evolution ( Table 2 ). In group 2, 6 patients required a PPM at follow-up (13 ± 15 months), including 5 who developed complete AVB. The remaining patient exhibited severe conduction disturbances associated with presyncopal episodes (bifascicular block with first-degree AVB; Table 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


