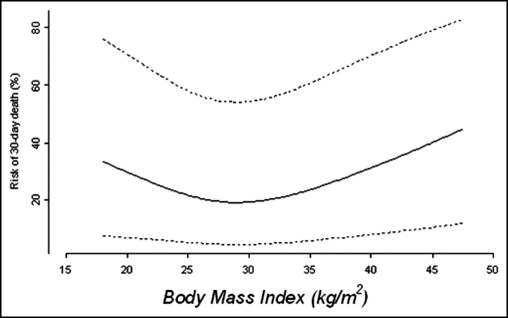
The purpose of this report is to describe the effect of body mass index (BMI) on 30-day and late outcome in patients having aortic valve replacement (AVR) for aortic stenosis (AS) with or without concomitant coronary artery bypass grafting. From January 2002 through June 2010 (8.5 years), 1,040 operatively excised stenotic aortic valves were submitted to the cardiovascular laboratory at Baylor University Medical Center at Dallas. Of the 1,040 cases 175 were eliminated because they had a previous cardiac operation. The present study included 865 adults whose AVR for AS was their first cardiac operation. Propensity-adjusted analysis showed that 30-day and late mortality were strongly and significantly associated with BMI. Decreased risk of 30-day and long-term mortality was observed for patients with BMI in the low 30s compared to patients with BMI in the mid 20s or >40 kg/m 2 . In conclusion, the findings in this study indicate a strong and significant adjusted association between BMI and 30-day and long-term mortality in patients having AVR for AS with or without concomitant coronary artery bypass grafting. Better survival was observed in patients with BMIs in the low 30s compared to patients with BMIs in the mid 20s and >40 kg/m 2 .
Most adults currently living in the United States are overweight. This report examines the effect of body mass index (BMI) on short- and long-term mortality in patients with aortic stenosis (AS) (with or without aortic regurgitation [AR]) undergoing aortic valve replacement (AVR).
Methods
The surgical pathology files of the cardiovascular laboratory—a part of the pathology department at Baylor University Medical Center (BUMC) at Dallas—were searched for patients having operatively excised aortic valves without simultaneous repair or replacement of the mitral valve or evidence of mitral stenosis. From January 2002 through June 2010 (102 months or 8.5 years) 1,040 operatively excised stenotic aortic valves were submitted to the cardiovascular laboratory at BUMC. Of the 1,040 cases 175 were eliminated from the present study because they had had a previous cardiac operation and/or an operative procedure on the mitral valve. The present study includes 865 adults whose AVR for AS was their first cardiac operation with or without a first simultaneous coronary artery bypass grafting (CABG) procedure. Clinical, echocardiographic, hemodynamic, angiographic, and operative records were sought from patients’ medical records and/or the BUMC Apollo cardiovascular database. Information on death of any patient was obtained from medical records for deaths during hospitalization at the time of AVR and from the Society of Thoracic Surgeons national database and/or from the Social Security Death Index for deaths after hospitalization. Echocardiographic data preoperatively were available to us in 426 patients and hemodynamic/angiographic data in 561 patients. These procedures also were performed in the other patients but at other institutions before their hospitalization at BUMC. The results of these studies at the referring institutions were not available to us. This study was approved by the institutional review board at BUMC and the requirement for individual patient consent was waived.
Means ± SDs and percentages were calculated to describe the study cohort. Differences in demographic, clinical, and morphologic details were tested with a Wilcoxon (for continuous factors) or a chi-square (for categorical factors) test. A Bonferroni correction was employed to account for multiplicity.
To better describe our study cohort, the crude association of BMI and the other factors considered for this study is presented by categorizing BMI into the following categories: ≤25, 26 to 30, 31 to 40, and >40 kg/m 2 . To rigorously assess the adjusted association between BMI and short-/long-term mortality and avoid bias inference regarding BMI and mortality, we modeled BMI using restricted cubic splines in the statistical models used for this analysis.
A propensity-score approach was used to assess the adjusted association between BMI and 30-day and long-term mortality. The propensity score was estimated using a linear regression model with BMI being the outcome and age, gender, race, aortic valve structure, valve weight, systemic hypertension, ascending aorta replaced, and type of implanted valve as possible confounding factors. Restricted cubic splines were used for all continuous variables. Multiple imputation using predictive mean matching was used to account for missing data regarding the independent variables in this model.
Estimates from the aforementioned propensity model were then used to adjust the effect of concomitant BMI on 30-day mortality in a logistic regression model and on long-term mortality in a Cox proportional hazards model. Possible effect modification by gender and age was investigated for the 2 models and ruled out. The Grambsch–Therneau test statistic was used to test for proportionality of hazards in the Cox model.
Results
The crude analysis showed that of the 14 factors analyzed, age, aortic valve area, 30-day mortality, and type substitute valve implanted were the only factors significantly different among the 4 BMI groups ( Table 1 ). Among the 3 age groups (21 to 50, 51 to 70, and 71 to 95 years) the oldest group had the highest percent with ideal (≤25 kg/m 2 ) BMI, and the middle-age group had the highest percent with morbid obesity (BMI >40 kg/m 2 ). Overweight (BMI >25 kg/m 2 ) was present in 46 of the 64 patients (72%) age 21 to 50 years; in 256 of the 338 patients (76%) age 51 to 70 years, and in 275 of the 463 patients (59%) age 71 to 95 years (p <0.001). Aortic valve area was inversely related to BMI (p <0.001). Type of substitute valve inserted also varied with BMI: the greater the BMI, the greater the chance that a mechanical prosthesis was used; conversely, the lower the BMI, the greater the likelihood that a bioprosthesis was used (p = 0.008). Of the 209 patients having a mechanical prosthesis, 152 (73%) were overweight (BMI >25 kg/m 2 ), and of the 649 patients having a bioprosthesis, 419 (65%) were overweight. Thirty-day and late mortality were strongly associated with the lowest and the highest BMI ( Figures 1 through 4 ).
| Variable | Total (n = 865) | Body Mass Index (kg/m 2 ) | p Value | |||
|---|---|---|---|---|---|---|
| ≤25 (n = 288, 33%) | 26–30 (n = 292, 34%) | 31–40 (n = 245, 28%) | >40 (n = 40, 5%) | |||
| Age group (years) | <0.001 | |||||
| 21–50 | 64 | 18 (28%) | 24 (38%) | 17 (27%) | 5 (8%) | |
| 51–70 | 338 | 82 (24%) | 102 (30%) | 126 (37%) | 28 (8%) | |
| 71–95 | 463 | 188 (41%) | 166 (36%) | 102 (22%) | 7 (2%) | |
| Gender | 0.913 | |||||
| Men | 517 | 162 (31%) | 192 (37%) | 144 (28%) | 19 (4%) | |
| Women | 348 | 126 (36%) | 100 (29%) | 101 (29%) | 21 (6%) | |
| Race | 0.834 | |||||
| White | 715 | 243 (34%) | 237 (33%) | 199 (28%) | 36 (5%) | |
| Black | 46 | 12 (26%) | 17 (37%) | 15 (33%) | 2 (4%) | |
| Hispanic | 35 | 8 (23%) | 14 (40%) | 13 (37%) | 0 | |
| Other | 69 | 25 (36%) | 24 (35%) | 18 (26%) | 2 (3%) | |
| Coronary bypass grafting | 426 | 148 (35%) | 156 (37%) | 104 (24%) | 18 (4%) | 0.872 |
| Number of major coronary arteries narrowed ≥50% | (n = 473) | (n = 155) | (n = 162) | (n = 131) | (n = 25) | 0.33 |
| 0 | 266 | 83 (31%) | 87 (33%) | 80 (30%) | 16 (6%) | |
| 1 | 88 | 29 (33%) | 32 (36%) | 25 (28%) | 2 (2%) | |
| 2 | 74 | 29 (39%) | 26 (35%) | 14 (19%) | 5 (9%) | |
| 3 | 34 | 10 (29%) | 12 (35%) | 10 (29%) | 2 (6%) | |
| 4 | 11 | 4 (36%) | 5 (45%) | 2 (18%) | 0 | |
| Left ventricular-aorta peak systolic gradient (mm Hg) (mean) [median] (n = 475) | 11–154 (50) [46] | 11–130 (50) [49] | 11–125 (50) [45] | 11–154 (49) [46] | 23–114 (57) [50] | 0.577 |
| Aortic valve area (cm 2 ) (n = 474) | ||||||
| Mean ± SD | 0.81 ± 0.28 | 0.76 ± 0.26 | 0.78 ± 0.25 | 0.89 ± 0.32 | 0.95 ± 0.34 | <0.001 |
| Aortic valve structure | 0.863 | |||||
| Unicuspid | 59 | 24 (41%) | 21 (36%) | 13 (22%) | 1 (2%) | |
| Bicuspid | 382 | 119 (31%) | 130 (34%) | 111 (29%) | 22 (6%) | |
| Tricuspid | 424 | 145 (34%) | 141 (33%) | 121 (29%) | 17 (4%) | |
| Aortic valve weight (g) | 0.869 | |||||
| Unicuspid (mean) [median] | 1.19–7.15 (3.37) [3.19] | 1.19–5.87 (3.39) [3.41] | 1.20–7.15 (3.00) [2.70] | 1.72–6.40 (3.76) [3.77] | 5.84 | |
| Bicuspid (mean) [median] | 0.67–18.38 (3.11) [2.79] | 0.79–18.38 (3.21) [2.87] | 0.67–9.68 (3.08) [2.82] | 0.73–8.51 (3.08) [2.71] | 1.61–7.17 (2.98) [2.71] | |
| Tricuspid (mean) [median] | 0.43–6.40 (2.03) [1.91] | 0.55–6.40 (1.85) [1.67] | 0.43–5.50 (2.07) [1.99] | 0.69–5.63 (2.21) [2.19] | 0.82–3.66 (2.10) [1.85] | |
| Systemic hypertension by history | 613 | 195 (32%) | 204 (33%) | 182 (30%) | 32 (5%) | 0.356 |
| Days in hospital postoperatively in patients living >30 days (mean) [median] | 3–71 (9) [7] | 3–53 (9) [7] | 3–47 (9) [7] | 3–71 (9) [7] | 4–27 (8) [7] | 0.84 |
| Died ≤30 days postoperatively | 47 | 20 (43%) | 14 (30%) | 6 (13%) | 7 (15%) | 0.001 |
| Ascending aorta replaced | 37 | 8 (22%) | 13 (35%) | 16 (43%) | 0 | 0.758 |
| Implanted valve type | ||||||
| Mechanical | 209 | 57 (27%) | 64 (31%) | 68 (33%) | 20 (10%) | 0.008 |
| Bioprosthetic | 649 | 230 (35%) | 225 (35%) | 174 (27%) | 20 (3%) | |
| Ross procedure | 7 | 1 | 3 | 3 | 0 | |