Beta blockers are empirically used in many patients with heart failure (HF) and preserved ejection fraction (HFpEF) because they allow more time for diastolic filling and because they improve outcomes in patients with systolic HF. However, recent data suggest that impaired chronotropic and vasodilator responses to exercise, which can worsen with β blockade, may play a key role in the pathophysiology of HFpEF. We prospectively examined the association between β-blocker therapy after hospitalization for decompensated HF and HF rehospitalization at 6 months in 66 consecutive patients with HFpEF (71 ± 13 years old, 68% women, 42% Black). Subjects were stratified based on receiving (BB+; 15 men, 28 women) or not receiving (BB−) β-blockers at hospital discharge. In men, HF rehospitalization occurred less frequently in the BB+ than in the BB− group, albeit nonsignificantly (20% vs 50%, p = 0.29). In women, HF rehospitalization occurred more frequently in the BB+ than in the BB− group (75% vs 18%, p <0.001). In univariate analyses, discharge β-blocker was associated with HF rehospitalization in women (odds ratio [OR] 14.00, 95% confidence interval [CI] 3.09 to 63.51, p = 0.001), but not in men (OR 0.25, 95% CI 0.03 to 1.92, p = 0.18). In a forward logistic regression model that offered all univariate predictors of HF rehospitalization, discharge β blocker remained an independent predictor of HF rehospitalization in women (OR 11.06, 95% CI 1.98 to 61.67, p = 0.006). In conclusion, this small observational study suggests that β-blocker therapy may be associated with a higher risk of HF rehospitalization in women with HFpEF. The risks and benefits of β-blocker therapy in patients with HFpEF should be evaluated in randomized, controlled trials.
We evaluated patients with heart failure (HF) and preserved ejection fraction (HFpEF) who were hospitalized for decompensated HF and stratified them based on receiving (BB+) or not receiving (BB−) β blockers at the time of hospital discharge. We compared the change in New York Heart Association (NYHA) functional class and rehospitalization at 6 months between the BB+ and BB− groups and examined the association between β-blocker therapy at the time of hospital discharge and rehospitalization.
Methods
The study population consisted of consecutive patients with HFpEF who were admitted to 2 academic, urban hospitals in Baltimore, Maryland, with a primary diagnosis of decompensated HF during a 6-month period. All patients >18 years of age who presented with signs and symptoms of HF were included if they satisfied the Framingham criteria for the diagnosis of HF and had a left ventricular ejection fraction (LVEF) ≥50%. Subjects were excluded if they presented in shock, needed intubation, or were diagnosed with acute coronary syndromes, aortic dissection, severe anemia (hemoglobin <7.5 g/dl), or acute renal failure at time of admission. Other exclusion criteria included congenital or valvular heart disease, constrictive pericarditis, restrictive or hypertrophic cardiomyopathy, noncardiac causes for HF, significant pulmonary disease, pregnancy, dialysis dependence with objective evidence of increased dry weight by >5 lbs, or a projected life expectancy <6 months due to a noncardiac disease. All subjects gave written informed consent to participate in the study, which was approved by the institutional review board of the Johns Hopkins Medical Institutions.
At index hospitalization, all subjects underwent a complete medical evaluation, including collection of medical history and demographic data, anthropometric and blood pressure measurements, and a physical examination. NYHA class at time of hospitalization was determined by the admitting physician. LVEF was measured with echocardiography or ventriculography within 72 hours of enrollment. Glomerular filtration rate was estimated using the abbreviated Modification of Diet in Renal Disease equation.
At 3 and 6 months from the index hospitalization, a single investigator (D.T.B.) interviewed participants by telephone and reassessed NYHA class using a standard set of questions. Occurrence of HF rehospitalization (primary outcome), all-cause rehospitalization, or death during the follow-up period was also ascertained during the telephone interview. The small number of deaths during follow-up (n = 3) precluded meaningful comparisons of mortality between study groups. However, mortality was analyzed as part of the secondary outcomes, which included all-cause rehospitalization and the composite of “death or HF rehospitalization.” Change in NYHA class was calculated as NYHA class at 3 or 6 months after discharge minus NYHA class on admission.
Study groups were compared with Student’s t test for continuous variables and with chi-square or Fisher’s exact tests for categorical variables. Univariate and multivariate-adjusted associations between β-blocker therapy at time of hospital discharge (“discharge β blocker”) and study outcomes were assessed with logistic regression analyses. Goodness of fit was verified in all models with the Hosmer-Lemeshow test. All analyses were performed with SPSS 14.0 (SPSS, Inc., Chicago, Illinois). Unless specified otherwise, summary statistics are presented as mean ± SEM or proportions. Statistical significance was inferred for a p value <0.05.
Because our study was not a randomized trial, we computed propensity scores from baseline variables that might have influenced the decision to prescribe discharge β blockers, including age, gender, race, body mass index, smoking, study site, primary admitting service, coronary artery disease, hypertension, diabetes mellitus, new-onset HF, heart rate, systolic and diastolic blood pressures, and cardiac rhythm on admission. We then repeated the analyses while adjusting for these propensity scores in the final model.
Results
LVEF was available in 153 of 154 patients with HF who were hospitalized during the study period. Seventy subjects (46%) had HFpEF, including 22 men and 48 women. Six-month follow-up was completed in 21 men and 45 women, who were included in the analyses.
Subjects were evenly distributed between the 2 study sites ( Table 1 ). In men, there were no significant differences between the BB+ and BB− groups with respect to demographics, NYHA class, co-morbidities, or clinical or laboratory findings ( Table 1 ). In women, subjects in the BB+ group had a slightly better overall NYHA class than those in the BB− group, although they were less likely to present in sinus rhythm and tended to be older and have a lower estimated glomerular filtration rate than those in the BB− group ( Table 1 ).
| Variable | Men | Women | ||||
|---|---|---|---|---|---|---|
| BB− | BB+ | p Value | BB− | BB+ | p Value | |
| (n = 6) | (n = 15) | (n = 17) | (n = 28) | |||
| Age (years) | 66 ± 4 | 68 ± 4 | 0.83 | 67 ± 4 | 75 ± 2 | 0.07 |
| Body mass index (kg/m 2 ) | 33 ± 4 | 37 ± 4 | 0.55 | 34 ± 3 | 34 ± 2 | 0.98 |
| Black race | 2 (33%) | 10 (67%) | 0.33 | 6 (35%) | 10 (36%) | 0.59 |
| Never smoker | 1 (17%) | 3 (20%) | 1.00 | 5 (29%) | 11 (39%) | 0.50 |
| Study site | 1.00 | 0.37 | ||||
| Johns Hopkins Hospital | 3 (50%) | 9 (60%) | 9 (53%) | 11 (39%) | ||
| Johns Hopkins Bayview Medical Center | 3 (50%) | 6 (40%) | 8 (47%) | 17 (61%) | ||
| Primary admitting service | 0.07 | 0.56 | ||||
| General medicine | 2 (33%) | 11 (73%) | 10 (59%) | 12 (43%) | ||
| Hospitalist | 2 (33%) | 0 | 2 (12%) | 6 (21%) | ||
| Specialist | 2 (33%) | 4 (27%) | 5 (29%) | 10 (36%) | ||
| Co-morbidities | ||||||
| Previous heart failure | 3 (50%) | 10 (67%) | 0.63 | 10 (59%) | 15 (54%) | 0.73 |
| Hypertension | 5 (83%) | 15 (100%) | 0.29 | 13 (76%) | 26 (93%) | 0.18 |
| Coronary artery disease | 3 (50%) | 7 (47%) | 1.00 | 7 (41%) | 15 (54%) | 0.42 |
| Diabetes mellitus | 5 (83%) | 8 (53%) | 0.34 | 7 (41%) | 16 (57%) | 0.30 |
| Clinical findings at time of admission | ||||||
| Heart rate (min −1 ) | 78 ± 9 | 81 ± 4 | 0.73 | 84 ± 5 | 77 ± 4 | 0.27 |
| Systolic blood pressure (mm Hg) | 149 ± 9 | 137 ± 5 | 0.21 | 150 ± 10 | 154 ± 7 | 0.78 |
| Diastolic blood pressure (mm Hg) | 72 ± 7 | 76 ± 5 | 0.71 | 78 ± 5 | 75 ± 4 | 0.70 |
| Pulse pressure (mm Hg) | 77 ± 13 | 62 ± 5 | 0.32 | 73 ± 5 | 78 ± 5 | 0.49 |
| Mean blood pressure (mm Hg) | 98 ± 4 | 96 ± 4 | 0.77 | 102 ± 7 | 101 ± 5 | 0.95 |
| Sinus rhythm | 6 (100%) | 12 (80%) | 0.53 | 16 (94%) | 18 (64%) | 0.03 |
| New York Heart Association functional class | 0.61 | 0.04 | ||||
| I | 0 | 0 | 0 | 0 | 0 | |
| II | 0 | 0 | 0 | 4 (14%) | ||
| III | 1 (17%) | 6 (40%) | 3 (18%) | 11 (39%) | ||
| IV | 5 (83%) | 9 (60%) | 14 (82%) | 13 (46%) | ||
| Overall, mean ± SEM | 3.8 ± 0.2 | 3.6 ± 0.1 | 0.29 | 3.8 ± 0.1 | 3.3 ± 0.1 | 0.004 |
| Laboratory findings | ||||||
| Albumin (g/dl) | 3.9 ± 0.2 | 3.6 ± 0.2 | 0.26 | 3.7 ± 0.1 | 3.8 ± 0.1 | 0.67 |
| Sodium (mmol/L) | 136 ± 3 | 140 ± 1 | 0.18 | 137 ± 1 | 140 ± 1 | 0.007 |
| Glucose (mg/dl) | 227 ± 45 | 144 ± 18 | 0.053 | 121 ± 8 | 136 ± 11 | 0.31 |
| Hemoglobin (g/dl) | 12.2 ± 0.4 | 11.4 ± 0.5 | 0.23 | 11.9 ± 0.5 | 11.1 ± 0.4 | 0.18 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 63 ± 12 | 64 ± 8 | 0.91 | 76 ± 9 | 56 ± 6 | 0.07 |
| Propeptide of brain-type natriuretic peptide (pg/ml), median (interquartile range) ⁎ | 1,167 (120–1,333) | 2,408 (481–7,136) | 0.59 | 1,326 (131–10,065) | 5,781 (676–8,009) | 0.56 |
There were no significant differences in admission or discharge medications between men in the BB+ and BB− groups ( Table 2 ). Women in the BB+ group were more likely than those in the BB− group to receive angiotensin-converting enzyme inhibitors, nitrates, and diuretics at time of hospital admission and at discharge ( Table 2 ).
| Medication | Men | Women | ||||
|---|---|---|---|---|---|---|
| BB− | BB+ | p Value | BB− | BB+ | p Value | |
| (n = 6) | (n = 15) | (n = 17) | (n = 28) | |||
| Any β blocker | ||||||
| Admission | 2 (33%) | 13 (87%) | 0.03 | 2 (12%) | 24 (86%) | <0.001 |
| Discharge | 0 | 15 (100%) | — | 0 | 28 (100%) | — |
| α and β blockers | ||||||
| Admission | 1 (17%) | 1 (7%) | 1.00 | 0 | 1 (4%) | 1.00 |
| Discharge | 0 | 1 (7%) | 1.00 | 0 | 1 (4%) | 1.00 |
| Angiotensin-converting enzyme inhibitors | ||||||
| Admission | 5 (83%) | 8 (53%) | 0.34 | 4 (24%) | 19 (68%) | 0.004 |
| Discharge | 5 (83%) | 9 (60%) | 0.61 | 5 (29%) | 20 (71%) | 0.006 |
| Angiotensin receptor blockers | ||||||
| Admission | 0 | 2 (13%) | 0.57 | 3 (18%) | 3 (11%) | 0.66 |
| Discharge | 1 (17%) | 1 (7%) | 1.00 | 3 (18%) | 2 (7%) | 0.35 |
| Nitrates | ||||||
| Admission | 1 (17%) | 3 (20%) | 1.00 | 0 | 8 (29%) | 0.02 |
| Discharge | 0 | 2 (13%) | 0.57 | 1 (6%) | 11 (39%) | 0.02 |
| Diuretic | ||||||
| Admission | 4 (67%) | 12 (80%) | 0.60 | 6 (35%) | 19 (68%) | 0.03 |
| Discharge | 4 (67%) | 13 (87%) | 0.54 | 9 (53%) | 22 (79%) | 0.07 |
| Spironolactone | ||||||
| Admission | 0 | 0 | — | 0 | 1 (4%) | 1.00 |
| Discharge | 0 | 1 (7%) | 1.00 | 1 (6%) | 2 (7%) | 1.00 |
| Amiodarone | ||||||
| Admission | 0 | 1 (7%) | 1.00 | 1 (6%) | 3 (11%) | 0.66 |
| Discharge | 0 | 1 (7%) | 1.00 | 1 (6%) | 2 (7%) | 1.00 |
| Digoxin | ||||||
| Admission | 0 | 2 (13%) | 0.57 | 0 | 2 (7%) | 0.52 |
| Discharge | 0 | 1 (7%) | 1.00 | 1 (6%) | 3 (11%) | 0.66 |
| Aspirin | ||||||
| Admission | 3 (50%) | 9 (60%) | 1.00 | 4 (24%) | 15 (54%) | 0.048 |
| Discharge | 4 (67%) | 11 (73%) | 1.00 | 8 (47%) | 18 (64%) | 0.35 |
| Warfarin | ||||||
| Admission | 2 (33%) | 3 (20%) | 0.60 | 2 (12%) | 7 (25%) | 0.45 |
| Discharge | 1 (17%) | 4 (27%) | 1.00 | 2 (12%) | 8 (29%) | 0.28 |
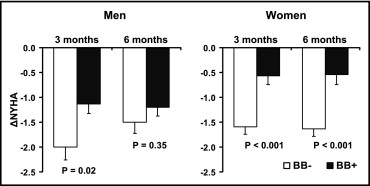
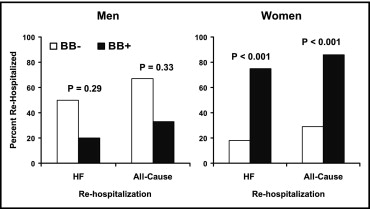
In men, change in NYHA class at 6 months did not differ between the BB+ and BB− groups (−1.20 ± 0.17 vs −1.50 ± 0.22, respectively, p = 0.35). In women, change in NYHA class at 6 months in the BB+ group was smaller than in the BB− group (−0.54 ± 0.20 vs −1.63 ± 0.15, p <0.001; Figure 1 ). At 6 months, 3 subjects died (1 man in the BB+ group and 2 women in the BB− group) and 38 subjects (29 women) had ≥1 all-cause rehospitalization. Of these, 30 subjects (24 women) had ≥1 HF rehospitalization. In men, HF rehospitalizations occurred less frequently in the BB+ group (3 of 15 subjects, 20%) than in the BB− group (3 of 6 subjects, 50%), albeit not significantly (p = 0.29), and a similar pattern was observed for all-cause rehospitalization (33% vs 67%, respectively, p = 0.33). Conversely, in women, HF rehospitalizations occurred more frequently in the BB+ than in the BB− group (75% vs 18%, p <0.001), and a similar pattern was present for all-cause rehospitalization (86% vs 29%, p <0.001; Figure 2 ).