The neutrophil/lymphocyte (N/L) ratio integrates information on the inflammatory milieu and physiologic stress. It is an emerging marker of prognosis in patients with cardiovascular disease. We investigated the relation between the N/L ratio and postoperative atrial fibrillation (AF) in patients undergoing coronary artery bypass grafting. In a prospective cohort study, 275 patients undergoing nonemergency coronary artery bypass grafting were recruited. Patients with previous atrial arrhythmia or requiring concomitant valve surgery were excluded. The N/L ratio was determined preoperatively and on postoperative day 2. The study end point was AF lasting >30 seconds. Patients who developed AF (n = 107, 39%) had had a greater preoperative N/L ratio (median 3.0 vs 2.4, p = 0.001), but no differences were found in the other white blood cell parameters or C-reactive protein. The postoperative N/L ratio was greater in patients with AF (day 2, median 9.2 vs 7.2, p <0.001), and in multivariate models, a greater postoperative N/L ratio was independently associated with a greater incidence of AF (odds ratio 1.10 per unit increase, p = 0.003: odds ratio for N/L ratio >10.14 [optimal postoperative cutoff in our cohort], 2.83 per unit, p <0.001). Elevated pre- and postoperative N/L ratios were associated with an increased occurrence of AF after coronary artery bypass grafting. In conclusion, these results support an inflammatory etiology in postoperative AF but suggest that other factors are also important.
Population studies have suggested a link between inflammation and atrial fibrillation (AF). The inflammatory response might also be associated with new-onset AF after coronary artery bypass grafting. In this setting, a more pronounced increase in the postoperative white blood cell count (WCC) has been associated with a greater risk of AF. However, the total WCC is a composite variable and a relatively crude marker of inflammation. More recently, the neutrophil/lymphocyte (N/L) ratio, which can be easily derived from the differential WCC and integrates the detrimental effects of neutrophilia (reflecting inflammation) and lymphopenia (a marker of poorer general health and physiologic stress), has emerged as a potentially useful prognostic parameter. The N/L ratio is more closely associated with mortality than the WCC in patients undergoing coronary angiography and angioplasty, in those with stable and unstable coronary heart disease, and in patients undergoing coronary artery bypass grafting. However, the relation between the N/L ratio and postoperative AF has not been assessed. We hypothesized that an elevated preoperative N/L ratio would be associated with an increased incidence of AF after coronary artery bypass grafting. In addition, we aimed to determine the relative utility of the preoperative N/L ratio, WCC, and C-reactive protein (CRP) in predicting postoperative AF and to assess the relation between the postoperative N/L ratio and the incidence of AF.
Methods
The Grampian Research Ethics Committee approved the study, and all patients provided written consent. From October 2005 to June 2007, 275 patients who were undergoing isolated coronary artery bypass grafting at our institution were recruited. Patients with previous atrial arrhythmia and those undergoing emergency or valve surgery were excluded. The baseline clinical data were obtained prospectively. The data included cardiovascular risk factors, cardiac medication, medical history, and estimates of operative risk (Parsonnet score and the European System for Cardiac Operative Risk Evaluation [EuroSCORE]). All preoperative analyses used the blood sample obtained immediately before surgery. An additional sample was obtained on postoperative day 2. The differential leukocyte count was obtained using an Advia 2120 Hematology System (Bayer HealthCare, Tarrytown, New York). This system has an excellent correlation with manual cell counts, with coefficients of variation of <2.5% for the WCC, <1.5% for the neutrophil count, and <2.9% for the lymphocyte count. The total WCC and neutrophil, lymphocyte, and monocyte counts were recorded, and the N/L ratio was calculated from these parameters. The high-sensitivity CRP levels were measured using the Siemens Prospec analyzer (Siemens Healthcare Diagnostics, Deerfield, Illinois), and the preoperative glomerular filtration rate was estimated using standard methods.
Electrocardiographic monitoring began immediately postoperatively and continued for 72 hours using 2-lead Holter monitors (Spiderview and Syneflash, ELA Medical, Plymouth, Minnesota). Subsequent 12-lead electrocardiograms were obtained daily from each patient until discharge or for 7 days postoperatively (if hospitalized >1 week). The Holter monitor recordings were analyzed by an experienced cardiac technician and a cardiologist, blinded to other study data, using Synescope software (ELA Medical). The primary end point was the development of postoperative AF, defined as an irregular rhythm in the absence of identifiable P waves, lasting for >30 seconds on Holter monitoring or on a 12-lead electrocardiogram, during the first week after surgery.
Normally distributed continuous data are expressed as the mean and standard deviation and, where skewed, as median values with the interquartile range. Categorical variables are presented as absolute values (and percentages). To compare groups, the chi-square test was used for categorical variables and the t test or Mann-Whitney U test for continuous variables. Correlations were assessed using Spearman’s rank test. Receiver operating characteristic curve analysis was used to determine the optimum cutoff levels of N/L ratio to predict the occurrence of AF. Forward stepwise (entry 0.05, retention 0.10) multivariate logistic regression models were created to identify independent predictors of postoperative AF. A 2-sided p value of <0.05 was considered statistically significant.
Results
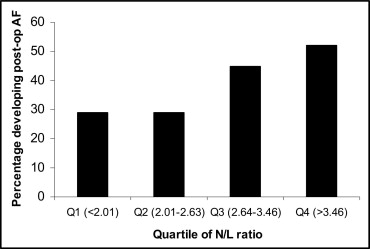
The study cohort was predominantly male (n = 230, 83.6%), with a median age of 65 years (interquartile range 58 to 70). Four patients (1.5%) were of Asian origin, and the remaining patients were white. Of the 275 patients, 3 died during their hospital stay after surgery. During in-patient follow-up, 107 patients (38.9%) developed AF, with onset a median of 3 (interquartile range 2 to 3) days after surgery. The median preoperative total WCC was 7.6 × 10 9 /L (interquartile range 6.7 to 9.3 × 10 9 /L), and the median N/L ratio was 2.64 (interquartile range 2.07 to 3.47). The patients with a greater N/L ratio tended to be older and had a greater prevalence of previous myocardial infarction and hypertension. Greater ratios were also associated with increased levels of preoperative high-sensitivity CRP and estimates of operative risk ( Table 1 ). Patients in the greatest quartile of the preoperative N/L ratio were at a greater risk of developing AF (odds ratio [OR] 2.62, 95% confidence interval [CI] 1.30 to 5.29 for quartile 4 vs quartile 1, p = 0.007; Table 1 and Figure 1 ).
| Characteristic | Quartile 1 (<2.01; n = 68) | Quartile 2 (2.01–2.63; n = 69) | Quartile 3 (2.64–3.46; n = 69) | Quartile 4 (>3.46; n = 69) | p Value |
|---|---|---|---|---|---|
| Age (years) | 60 (54–68) | 62 (57–68) | 67 (61–70) | 68 (62–72) | <0.001 |
| Men | 54 (79%) | 60 (87%) | 56 (81%) | 60 (87%) | 0.42 |
| Body mass index (kg/m 2 ) | 28.4 (26.6–31.0) | 28.0 (25.8–30.3) | 29.4 (26.6–34.2) | 28.7 (26.7–31.8) | 0.31 |
| Previous myocardial infarction | 29 (43%) | 25 (36%) | 28 (41%) | 44 (64%) | 0.01 |
| Ejection fraction (%) | 50.9 ± 8.6 | 51.0 ± 7.9 | 52.0 ± 8.8 | 52.2 ± 11.3 | 0.79 |
| Diabetes mellitus | 13 (19%) | 12 (17%) | 13 (19%) | 11 (16%) | 0.67 |
| Current smoker | 7 (10%) | 9 (13%) | 6 (9%) | 11 (16%) | 0.51 |
| Hypertension | 44 (65%) | 39 (57%) | 51 (74%) | 54 (78%) | 0.02 |
| EuroSCORE (logistic) | 1.69 (1.23–2.83) | 1.51 (1.04–2.35) | 2.07 (1.49–3.99) | 2.51 (1.56–3.73) | <0.001 |
| Parsonnet score | 4 (3–9) | 4 (3–7) | 6 (3–10) | 6 (3–12) | 0.001 |
| New York Heart Association functional class III/IV | 2 (3%) | 5 (7%) | 2 (3%) | 4 (6%) | 0.80 |
| Canadian Cardiovascular Society angina class III/IV | 21 (31%) | 28 (41%) | 26 (38%) | 32 (46%) | 0.13 |
| Estimated glomerular filtration rate (ml/min/1.73 cm 2 ) | 65.5 (59.1–74.7) | 67.9 (58.6–73.3) | 60.8 (54.4–72.2) | 64.5 (52.2–71.1) | 0.01 |
| Aspirin/clopidogrel | 67 (99%) | 67 (97%) | 67 (97%) | 69 (100%) | 1.00 |
| β Blocker | 59 (87%) | 51 (74%) | 40 (58%) | 59 (86%) | 0.41 |
| Statin | 67 (99%) | 64 (93%) | 65 (94%) | 67 (97%) | 0.90 |
| Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker | 39 (57%) | 39 (57%) | 38 (55%) | 48 (70%) | 0.19 |
| Preoperative hemoglobin (g/L) | 145 (135–155) | 143 (136–152) | 145 (136–153) | 145 (134–152) | 0.92 |
| Preoperative total white blood cell count (×10 9 /L) | 7.5 (6.6–8.6) | 7.7 (6.9–9.2) | 7.4 (6.3–9.0) | 8.8 (7.3–10.4) | 0.05 |
| High-sensitivity C-reactive protein (mg/L) ⁎ | 1.46 (0.63–3.64) | 1.80 (0.74–3.80) | 1.71 (0.79–3.69) | 2.37 (1.19–6.48) | 0.008 |
| Off-pump procedure | 8 (12%) | 5 (7%) | 7 (10%) | 11 (16%) | 0.39 |
| Preoperative intra-aortic balloon pump | 8 (12%) | 6 (9%) | 12 (17%) | 15 (22%) | 0.05 |
| No. of bypass grafts | 3 (2–3) | 3 (2–3) | 3 (2–3) | 3 (2–3) | 0.79 |
| Internal mammary artery used | 57 (84%) | 60 (87%) | 60 (87%) | 55 (80%) | 0.71 |
| Bypass time (min) | 77 (53–97) | 73 (53–83) | 74 (60–90) | 68 (43–87) | 0.22 |
| Cross-clamp time (min) | 44 (34–53) | 38 (29–47) | 43 (33–53) | 37 (23–51) | 0.37 |
| Perioperative inotropes | 51 (75%) | 47 (68%) | 47 (68%) | 50 (72%) | 0.93 |
| Postoperative total white blood cell count (×10 9 /L) † | 12.6 (10.5–15.0) | 11.8 (10.1–14.8) | 12.1 (10.4–14.9) | 13.0 (10.7–16.1) | 0.34 |
| Postoperative C-reactive protein (mg/L) ‡ | 173 (142–194) | 157 (136–206) | 162 (139–199) | 167 (133–208) | 0.80 |
| Postoperative troponin I at 48 hours (ng/ml) § | 5.12 (2.16–7.81) | 5.11 (2.91–8.43) | 4.98 (2.50–8.31) | 3.80 (2.22–7.12) | 0.22 |
| Postoperative atrial fibrillation | 20 (29%) | 20 (29%) | 31 (45%) | 36 (52%) | 0.001 |
⁎ Not available for 5 patients.
† Not available for 4 patients.
‡ Not available for 11 patients.
The patients who developed AF were significantly older and had greater preoperative risk scores than those who maintained sinus rhythm ( Table 2 ). The patients in both groups were prescribed similar medical therapy, although a lower percentage of patients who developed postoperative AF were taking a β blocker preoperatively. No patients were using sotalol preoperatively, but 1 patient had been prescribed amiodarone. None were treated with other antiarrhythmic medication preoperatively. No differences in the perioperative variables were found between the 2 groups. The preoperative N/L ratio was greater in the patients who developed AF, but no difference was found in the total WCC. Although the preoperative lymphocyte count was lower in patients with AF, no differences were found in the neutrophil count or high-sensitivity CRP.
| Variable | AF | p Value | |
|---|---|---|---|
| No (n = 168) | Yes (n = 107) | ||
| Patient characteristics | |||
| Age (years) | 63 (58–69) | 68 (60–71) | <0.001 |
| Men | 136 (81%) | 94 (87.9%) | 0.132 |
| Body mass index (kg/m 2 ) | 28.2 (26.1–31.1) | 29.2 (26.9–32.3) | 0.140 |
| Previous myocardial infarction | 70 (42%) | 56 (52%) | 0.083 |
| Ejection fraction (%) | 51.5 (±9.0) | 51.6 (±9.5) | 0.930 |
| Diabetes mellitus | 26 (15%) | 23 (21%) | 0.198 |
| Current smoker | 21 (12.5%) | 12 (11%) | 0.723 |
| Hypertension | 115 (68.5%) | 73 (68%) | 0.968 |
| EuroSCORE (logistic) | 1.70 (1.22–3.30) | 2.20 (1.51–3.35) | 0.021 |
| Parsonnet score | 4 (3–8) | 6 (3–11) | 0.012 |
| New York Heart Association functional class III/IV | 8 (5%) | 5 (5%) | 0.938 |
| Canadian Cardiovascular Society angina class III/IV | 60 (37%) | 47 (44%) | 0.242 |
| Estimated glomerular filtration rate (ml/min/1.73 cm 2 ) | 65.0 (55.5–72.8) | 65.3 (54.5–72.7) | 0.797 |
| Preoperative medications | |||
| Aspirin/clopidogrel | 164 (99%) | 106 (99%) | 0.834 |
| β Blocker | 134 (80%) | 75 (70%) | 0.067 |
| Statin | 162 (96%) | 101 (94%) | 0.420 |
| Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker | 97 (58%) | 67 (63%) | 0.421 |
| Preoperative blood results | |||
| Hemoglobin (g/L) | 143 (136–151) | 146 (135–154) | 0.178 |
| Total white cell count (×10 9 /L) | 7.6 (6.7–9.1) | 7.7 (6.8–9.6) | 0.589 |
| Neutrophil count (×10 9 /L) | 4.7 (3.9–5.9) | 5.1 (4.2–6.2) | 0.101 |
| Lymphocyte count (×10 9 /L) | 2.0 (1.5–2.5) | 1.7 (1.4–2.2) | 0.015 |
| Monocyte count (×10 9 /L) | 0.5 (0.4–0.6) | 0.5 (0.4–0.6) | 0.036 |
| Neutrophil/lymphocyte ratio | 2.42 (1.94–3.23) | 3.00 (2.30–3.85) | 0.001 |
| High-sensitivity C-reactive protein (mg/L) ⁎ | 1.58 (0.74–3.75) | 1.95 (0.85–5.03) | 0.317 |
| Perioperative data | |||
| Off-pump procedure | 16 (10%) | 15 (14%) | 0.251 |
| Preoperative intra-aortic balloon pump | 23 (14%) | 18 (17%) | 0.457 |
| No. of bypass grafts | 3 (2–3) | 3 (2–3) | 0.460 |
| Internal mammary artery used | 139 (83%) | 93 (88%) | 0.263 |
| Bypass time (min) | 73 (54–90) | 73 (52–90) | 0.962 |
| Cross-clamp time (min) | 40 (32–51) | 42 (29–51) | 0.782 |
| Perioperative inotropes | 122 (73%) | 73 (72%) | 0.852 |
| Postoperative blood results | |||
| Hemoglobin (g/L) † | 99 (91–109) | 100 (91–109) | 0.824 |
| Total white cell count (×10 9 /L) † | 12.1 (10.1–14.4) | 13.9 (10.9–16.2) | 0.005 |
| Neutrophil count (×10 9 /L) † | 9.7 (7.8–12.1) | 11.2 (8.8–14.0) | 0.002 |
| Lymphocyte count (×10 9 /L) † | 1.3 (1.0–1.6) | 1.2 (1.0–1.6) | 0.114 |
| Monocyte count (×10 9 /L) † | 0.7 (0.6–0.9) | 0.7 (0.6–1.0) | 0.312 |
| C-reactive protein (mg/L) ‡ | 163 (137–190) | 172 (138–220) | 0.123 |
| Neutrophil/lymphocyte ratio † | 7.25 (5.33–9.80) | 9.21 (6.31–12.04) | <0.001 |
| Troponin I at 48 hours (ng/ml) § | 4.6 (2.6–7.7) | 5.0 (2.4–9.1) | 0.581 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


