Long-term survival in Hodgkin lymphoma (HL) survivors is complicated by an increased risk for coronary artery disease (CAD) due to radiation-induced endothelial damage. Our objective was to quantify total coronary artery calcium (CAC) in long-term HL survivors who had survived ≥15 years after treatment and relate it to the presence of verified CAD. Forty-seven HL survivors 50 ± 7 years of age who had survived 22 ± 3 years after mediastinal radiotherapy underwent CAC scoring (Agatston and volume scores) in a multidetector computed tomographic scanner. Total volume score was higher in 7 patients (15%) with verified CAD (median 439, range 8 to 2,057) compared to those without (median 68, 0 to 767, p = 0.022). Ten patients had CAC scores >200. Of these 10, 5 had undergone revascularization of coronary arteries. None of the 8 patients with a CAC score 0 had symptomatic CAD. In conclusion, postirradiation CAC can be quantified by CAC score and this may be a simple and suitable method to screen for CAD in long-term HL survivors. Patients with a CAC score >200 often have clinically significant CAD, and further investigation including angiography may be justified. Lower CAC scores, however, do not exclude CAD and further studies should be undertaken to define the best algorithm for follow-up of this patient group.
Asymptomatic survivors of Hodgkin lymphoma (HL) are in need of regular follow-up. Mediastinal radiotherapy and anthracycline-containing chemotherapy are associated with premature cardiac disease. Calcium deposits in coronary arteries correlate closely with overall burden of atherosclerotic plaques. A simple, noninvasive screening test with the ability to identify HL survivors at increased risk for cardiac events would be of interest. The purpose of the present study was to quantify coronary artery calcium (CAC) and relate it to confirmed coronary artery disease (CAD), and the absence of the same, in long-term HL survivors.
Methods
Forty-seven patients (31 women) 50 ± 7 years of age were examined on follow-up from 2005 to 2007. They were treated for HL at Oslo University Hospital (Norwegian Radium Hospital), Oslo, Norway, from 1980 to 1988, being on average 27 ± 6 years of age at time of disease debut. All patients had received mediastinal radiotherapy delivered in daily fractional doses of 1.8 or 2.0 Gy 5 days a week, with a total mean dose of 40.6 ± 2.3 Gy. No subcarinal blocks or cardiac shields were used. Anthracycline containing chemotherapy was given to 27 patients. Information about cardiovascular events and aspects regarding treatment of cancer was obtained from medical records ( Table 1 ). CAD was diagnosed with coronary angiography after occurrence of myocardial infarction, angina, or after preoperative angiography for aortic stenosis. Serum levels of cholesterols, triglycerides, C-reactive protein, and pro–B-type natriuretic peptide were measured. All participants gave their informed consent. The study protocol was approved by the institutional review board.
| Variable | |
|---|---|
| Age (years) at follow-up | 50 ± 7 |
| Observation time (years) (from radiation therapy) | 22 ± 3 |
| Cancer stages 1 and 2 | 36 (77%) |
| Cancer stages 3 and 4 | 11 (23%) |
| Relapses | 6 (13%) |
| Radiation dose (Gy) | 40.6 ± 2.3 |
| Chemotherapy ⁎ | 35 (74%) |
| Received anthracyclines | 27 (57%) |
| Dose of anthracyclines (mg) ⁎ | 313 ± 92 |
| Current smoker | 14 (30%) |
| Clinical findings | |
| Systolic blood pressure (mm Hg) | 122 ± 17 |
| Diastolic blood pressure (mm Hg) | 71 ± 10 |
| Hypertension † | 13 (28%) |
| Body mass index (kg/m 2 ) | 23.8 ± 3.7 |
| History of hypercholesterolemia | 10 (21%) |
| Diabetes | 1 (2%) |
| Blood samples | |
| Total cholesterol (mg/dl) | 205 ± 31 |
| High-density lipoprotein cholesterol (mg/dl) | 54 ± 15 |
| Low-density lipoprotein cholesterol (mg/dl) | 128 ± 27 |
| Triglycerides (mg/dl) | 115 ± 53 |
| C-reactive protein (mg/dl) | 0.22 (0.02–4.30) |
| Pro–B-type natriuretic peptide (ng/dl) | 29 (3–174) |
| Ongoing medical treatment | |
| Platelet inhibitors/anticoagulant | 8 (17%) |
| Statins | 8 (17%) |
| β blocker | 11 (23%) |
| Angiotensin-converting enzyme inhibitor/angiotensin II-inhibitor | 8 (17%) |
| Calcium antagonist | 3 (6%) |
⁎ Also including chemotherapy for relapses.
† Systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg or use of antihypertensive medication to lower blood pressure.
All patients were examined in a 64-detector row computed tomographic unit (GE LightSpeed 64 VCT, GE Healthcare, Milwaukee, Wisconsin) including a dedicated workstation (Advantage Window 4.3.3) for quantification of CAC by a computerized program (SmartScore 3.5, GE Medical Systems, Milwaukee, Wisconsin) that provided the CAC score as an Agatston score and a volume score. Assignment of segments to coronary arterial territories was done in accordance with clinical recommendations. Scoring was carried out independently by 2 experienced radiologists (RA and AG). Three patients underwent percutaneous coronary intervention with implantation of a stainless steel stent in 1 coronary artery. The arterial segment with stent was excluded from calcium score calculation.
Statistical analyses were performed with SPSS 14.0 for Windows (SPSS, Inc., Chicago, Illinois). Data are presented as mean ± SD or percentage. Median and range are presented for C-reactive protein, pro–B-type natriuretic peptide, and CAC volume score. Total CAC volume score were calculated as the sum of scores in the left main, left anterior descending, circumflex, and right coronary arteries. We categorized patients according to the following ranges for volume score: 0, 1 to 199, 200 to 999, and ≥1,000. Chi-square test was performed to compare categorical data between patients with and without verified CAD. Mann-Whitney test was used to compare continuous variables including CAC volume score in HL survivors with and without CAD. Multiple logistic regression analyses were performed with the presence of CAD as a dependent variable and total CAC volume score, presence of aortic stenosis, pathologic pro–B-type natriuretic peptide value, gender, and age at HL diagnosis (all with p <0.20) as independent variables. A 2-tailed p value ≤0.05 was considered statistically significant.
Results
Seven of 47 patients had verified CAD, 4 with myocardial infarction, 2 with angina, and 1 with silent CAD detected by invasive angiography preoperatively before aortic valve replacement. All 7 had undergone revascularization. Three other patients had stroke or transitory ischemic attack. Additional patient characteristics and measurements are listed in Table 1 .
Total volume score was higher in patients with verified CAD than in those without evidence of CAD (439, range 8 to 2,057, and 68, range 0 to 767, respectively, p = 0.022). The left main, left anterior descending, and circumflex coronary arteries had a higher CAC volume score in patients with verified CAD compared to patients without, whereas the volume score for the right coronary artery was comparable in the 2 groups ( Figure 1 ). Two of the patients who had undergone revascularization with stenting of 1 coronary artery had total volume scores of 8 and 46, respectively, after excluding the artery with stented segments from quantification of calcium.
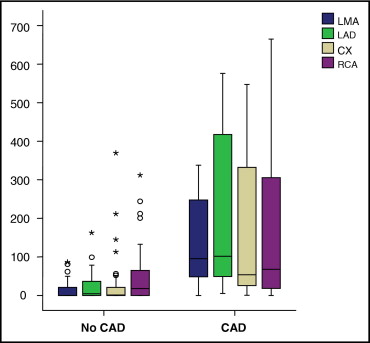
Categorization of CAC score ( Table 2 ) revealed a difference in the distribution of total volume score between patients with and without CAD (p < 0.001). Of 10 patients with a volume score >200, 5 had undergone revascularization, 4 with bypass grafting and 1 with percutaneous angioplasty. The 5 patients without a history of CAD and who had a volume score >200 had detectable calcium mainly in the right coronary and the left circumflex coronary arteries.



