Patients with obstructive hypertrophic cardiomyopathy who undergo septal myectomy are at risk for developing postoperative atrial fibrillation. Amiodarone is effective in treating this arrhythmia but is associated with multiple adverse effects, often with delayed onset. A novel case is described of a patient who developed type 2 amiodarone-induced hyperthyroidism that presented as recurrence of outflow obstruction after septal myectomy. The patient’s symptoms and echocardiographic findings of outflow obstruction resolved substantially with the treatment of the amiodarone-induced hyperthyroidism. Amiodarone-induced hyperthyroidism of delayed onset can be a subtle diagnosis, requiring a high index of suspicion. In conclusion, recognition of this diagnosis in patients with recurrence of outflow obstruction by symptoms and cardiac imaging after septal myectomy may avoid unnecessary repeat surgical intervention.
Patients with obstructive hypertrophic cardiomyopathy (HC) are treated medically with β blockers, calcium channel blockers, or disopyramide. For patients not responding to or not appropriate for medical management, symptoms of HC can be relieved with septal myectomy, with low mortality. Postoperative atrial fibrillation occurs in approximately 30% of patients with HC after septal myectomy. Amiodarone is frequently used for treatment of patients with new-onset atrial fibrillation after cardiac surgery, especially when associated with rapid ventricular response, because of its benefits of rate control, rhythm control, limited negative inotropic effect, and low risk for proarrhythmia. Amiodarone is also the treatment of choice in the setting of ventricular hypertrophy. Despite the benefits of amiodarone, this medication also has multiple associated adverse effects, including thyroid, neurologic, dermatologic, hepatic, ocular, and cardiac.
Case Report
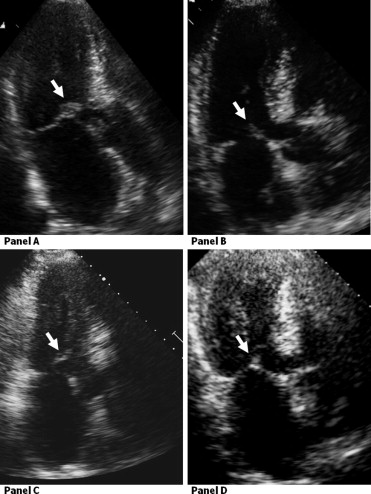
A 61-year-old man was diagnosed with HC when a murmur was heard on routine physical examination. The patient had an implantable cardioverter-defibrillator placed for primary prevention of sudden cardiac death given septal hypertrophy of 1.7 cm. He was treated medically with atenolol and verapamil until he had his first syncopal episode related to outflow obstruction. He developed progressive dyspnea on exertion, lightheadedness, and syncope. Preoperative transthoracic echocardiography (TTE) demonstrated asymmetrical septal hypertrophy, systolic anterior motion (SAM) of the mitral valve and the mitral valve chordae, and elevated peak left ventricular outflow tract gradients ( Figure 1 , Table 1 ). Cardiac catheterization demonstrated non-flow-limiting coronary artery disease. He underwent septal myectomy and division of the subvalvular chordae. The patient developed atrial fibrillation with a rapid ventricular response on the first postoperative day. He was given a loading dose of amiodarone and discharged on 200 mg/day by mouth. After the myectomy, his symptoms resolved, and TTE 3 months after surgery showed mild chordal SAM, resolution of SAM of the valve leaflets, and decreased gradients ( Figure 1 ). Amiodarone was stopped 4 months postoperatively.
| Variable | Before Myectomy | After Myectomy | 10 Months After Myectomy: Hyperthyroid | 2 Years After Myectomy: Asymptomatic |
|---|---|---|---|---|
| Peak LVOT gradient at rest (mm Hg) | 180 | 29 | 51 | 17 |
| Peak LVOT tract gradient after Valsalva maneuver (mm Hg) | 202 | 42 | 100 | 60 |
Six months after myectomy, the patient noted recurrent palpitations, dyspnea, and lightheadedness with exertion. At 10 months after myectomy, despite increasing doses of metoprolol, his symptoms worsened. Interrogation of his implantable cardioverter-defibrillator showed no episodes of atrial fibrillation or other arrhythmias. TTE now demonstrated SAM of the mitral valve with mitral-septal contact and increasing peak outflow tract gradients ( Figure 1 ). A second myectomy was considered. Thyroid function tests were obtained because of his previous exposure to amiodarone and indicated hyperthyroidism (see Table 2 ). Antithyroid test results were negative for Hashimoto’s thyroiditis and Graves’ disease, and the results of an iodine uptake scan were normal. Ultrasound of the thyroid showed an enlarged thyroid with 4 small, diffuse nodules. The patient was diagnosed with type 2 amiodarone-induced hyperthyroidism, and prednisone 40 mg/day by mouth was started. There was a gradual decrease in the free tetraiodothyronine and an increase in thyroid-stimulating hormone, while free triiodothyronine remained in the normal range. Prednisone was tapered over 2 months, and his symptoms resolved in parallel with the improvement in his thyroid function. He became asymptomatic on β blockers, with TTE showing mild chordal SAM and peak outflow tract gradients similar to postoperative levels ( Figure 1 ).
| Variable | 5/1/08 | 5/15/08 | 6/3/08 | 6/10/08 | 6/23/08 | 6/27/08 | 7/25/08 | 7/31/08 | 8/7/08 | 8/28/08 | 11/24/08 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Prednisone | — | — | Started | 40 mg | 20 mg | 10 mg | 5 mg | 2.5 mg | None | None | None |
| TSH ⁎ | 0.137 | 0.133 | 0.133 | 0.070 | 0.109 | 0.100 | 0.190 | 0.110 | 0.090 | 0.070 | 0.650 |
| Free T4 † | — | 1.26 | 1.23 | 1.13 | 1.20 | 1.15 | 0.94 | 1.19 | 1.06 | 1.07 | 0.89 |
| Free T3 ‡ | 2.94 | 3.31 | 3.10 | — | — | 2.82 | 2.96 | 3.28 | 3.51 | 3.40 | 3.20 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


