Diastolic function and E/e′ correlate with peak aerobic capacity (VO 2 ) in patients with heart failure, but the echocardiographic correlates of abnormal gas exchange in patients without heart failure are not well defined. We sought to determine the echocardiographic correlates of peak VO 2 and breathing efficiency (estimated using the ratio of minute ventilation to carbon dioxide production, or VE/VCO 2 nadir) in patients with unexplained dyspnea. We identified 232 patients with unexplained dyspnea who underwent echocardiography at rest followed by stress echocardiography with simultaneous measurement of peak VO 2 and VE/VCO 2 nadir. At baseline, 17 patients (5%) had an E/e′ of ≥15 while 31 patients (17%) had a right ventricular systolic pressure (RVSP) of >35 mm Hg. E/e′ ≥15 and RVSP >35 mm Hg were associated with lower peak VO 2 (14.1 ± 4.4 vs 21.0 ± 6.9 and 15.2 ± 3.6 vs 21.8 ± 6.8 ml/kg/min, respectively, p <0.0001). E/e′ ≥15 (sensitivity 0.13, specificity 0.99, area under the curve 0.64) and RVSP >35 mm Hg (sensitivity 0.38, specificity 0.93, area under the curve 0.76) were highly specific for predicting limited peak VO 2 . Age and RVSP at rest were independent correlates with VE/VCO 2 , but diastolic function was not. However, the risk of having abnormal VE/VCO 2 nadir was only elevated in subjects with elevated RVSP in the setting of abnormal diastolic function (hazard ratio 2.4, 95% confidence interval 1.3 to 4.6, p = 0.02). In conclusion, both E/e′ ≥15 and RVSP >35 mm Hg are highly specific markers of exercise limitation in patients without heart failure, but RVSP at rest may offer better overall diagnostic power than E/e′ to predict low peak VO 2 in this group.
Dyspnea is a frequent symptom that prompts patients to seek medical care, but identifying a cause of dyspnea is often challenging in clinical practice. Cardiopulmonary testing provides objective measurement of peak aerobic capacity (peak VO 2 ) and ventilatory efficiency (VE/VCO 2 ). Peak VO 2 correlates closely with peak cardiac output, and VE/VCO 2 (the ratio of minute ventilation to carbon dioxide production) is another important prognostic marker in patients with heart failure. Echocardiography complements cardiopulmonary testing by providing more specific information about cardiac function. The ratio of early transmitral peak velocity to mitral annular tissue velocity (E/e′) correlates with exercise capacity in patients with heart failure, but E/e′ may be less useful in the normal heart. Pulmonary hypertension may also be an important determinant of exercise performance and prognosis in patients with heart failure with preserved ejection fraction (HFpEF), but few studies have evaluated the correlation between Doppler-derived right ventricular systolic pressure (RVSP) and exercise performance in patients with unexplained dyspnea. We reviewed a cohort of subjects with unexplained dyspnea who underwent stress echocardiography with simultaneous cardiopulmonary exercise testing to determine the echocardiographic determinants of peak VO 2 and VE/VCO 2 nadir.
Methods
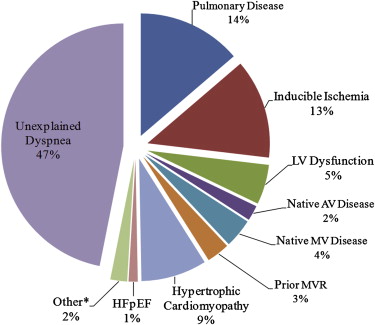
From July 2006 to December 2011, a total of 495 subjects underwent treadmill cardiopulmonary exercise testing with simultaneous stress echocardiography for the evaluation of dyspnea. We excluded subjects with moderate or greater lung disease by pulmonary function testing or an otherwise apparent cardiac cause of dyspnea ( Figure 1 ). We also excluded those with a history of mitral valve replacement or repair, because diastolic function assessment is unreliable in these groups due to alterations in transmitral and annular velocities. Three studies were technically inadequate. A total of 232 subjects with unexplained dyspnea were included in the analysis.
Each subject underwent symptom-limited graded treadmill cardiopulmonary exercise testing with continuous electrocardiographic monitoring and breath-by-breath gas exchange analysis consisting of 2-minute stages with 2-MET increases per stage. Blood pressure, heart rate, and continuous pulse oximetry were monitored during the testing period. Oxygen consumption (VO 2 ), carbon dioxide production (VCO 2 ), and minute ventilation (VE) were measured throughout the testing period. Ventilatory efficiency was calculated as the minimum ratio of VE/VCO 2 during exercise (VE/VCO 2 nadir). A VE/VCO 2 nadir of ≥33 was considered abnormal. A previous study from our institution showed a curvilinear relation between mortality and peak VO 2 and identified increased mortality for a peak VO 2 of <19 ml/kg/min in men and <15 ml/kg/min in women. Therefore, peak VO 2 <19 ml/kg/min in men and <15 ml/kg/min in women was considered “low VO 2 .” Peak VO 2 ≥19 ml/kg/min in men and ≥15 ml/kg/min in women was considered “preserved VO 2 .”
Subjects underwent a limited transthoracic echocardiography at rest, which included evaluation of left ventricular systolic and diastolic functions and estimated RVSP. E/e′, a noninvasive indicator of left ventricular filling pressure, was calculated using a ratio of the transmitral E wave and the medial mitral annular tissue velocity. Categorization of diastolic function based on E/A ratio, E/e′, and left atrial volume index (LAVI) can be found in Table 1 and has been previously described. In subjects with atrial fibrillation, those with an E/e′ of ≥15 and a LAVI of >28 ml/m 2 were graded as having elevated filling pressure. Those not meeting the criteria in Table 1 were graded as indeterminate. RVSP at rest was estimated using the simplified Bernoulli equation applied to the peak tricuspid regurgitation velocity obtained by continuous wave Doppler added to the estimated right atrial pressure. Use of saline contrast to enhance the continuous wave Doppler tricuspid regurgitation signal was at the discretion of the covering physician but was very uncommonly used. Right atrial pressure was estimated to be 5 mm Hg if the inferior vena cava (IVC) size was <20 mm and collapsed >50% with inspiration, 10 mm Hg if the IVC was <20 mm and collapsed <50% with inspiration, 15 mm Hg if the IVC was ≥20 mm and collapsed >50% with inspiration, and 20 mm Hg if the IVC was ≥20 mm and collapsed <50% with inspiration. RVSP at rest of >35 mm Hg was considered abnormal. Immediately after peak exercise, regional wall motion and ejection fraction were assessed from the parasternal and apical windows. A subset of patients had postexercise E/e′ and RVSP measured after regional wall motion assessment. A postexercise E/e′ of >13 and RVSP ≥50 mm Hg were considered abnormal.



