Ebstein Anomaly
Ebstein anomaly is a rare disease. The pathologic anatomy consists of displacement of part or all of the tricuspid valve orifice into the right ventricle. Attachments of all valve leaflets are abnormal, especially the septal and posterior leaflets, which are dysplastic and displaced downward. This gives rise to the extension of the right atrium into the right ventricle, resulting in an “atrialized” portion of the right ventricle above the valve. The anterior leaflet is large and usually has an abnormal insertion, sometimes producing obstruction in the right ventricular cavity. The atrioventricular node and conduction bundle lie within the triangle of Koch as in the normal heart, but because of the downward displacement of the valve below the true atrioventricular junction, the atrialized ventricle separates the penetrating bundle from the valve proper. An atrial septal defect or a patent foramen ovale is usually present (Fig. 28-1).
Presentation
There is a wide range of anatomic variations of Ebstein anomaly. The least severe form has a true right ventricle with adequate volume. These patients have very mild cyanosis and may be asymptomatic even as adults. The most severe form consists of nearly complete atrialization of the right ventricle. These patients present as neonates with massive cardiomegaly, severe heart failure, cyanosis, and acidosis.
Surgery for the Neonate
Neonates who demonstrate a need for mechanical ventilation and dependence on prostaglandin E1 to maintain ductal patency have a universally poor outcome with medical management. The surgical approach is designed to create a reliable source of pulmonary flow, reduce the massive cardiomegaly, and prevent severe tricuspid insufficiency. If there is a tripartite ventricle with an open right ventricular outflow tract and adequate valve tissue, a reparative procedure may be attempted. Most severely symptomatic neonates have unfavorable anatomy and marked dilation of the right side of the heart with impingement on the left ventricle and lungs. A right ventricular exclusion procedure decompresses the right side and can palliate these critically ill patients. This procedure creates a single ventricle physiology allowing for a future Fontan operation (see Chapter 31).
Technique
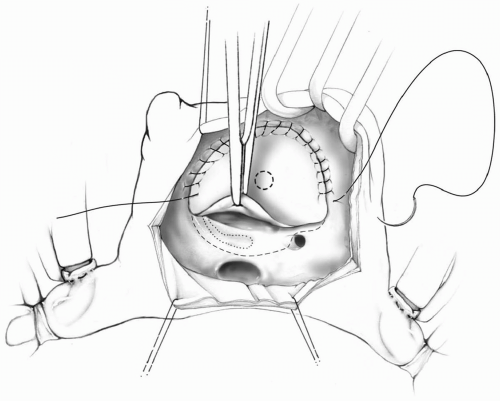
A median sternotomy is used, and standard aortic and bicaval cannulation is performed. The ductus arteriosus is ligated with the institution of cardiopulmonary bypass. Cooling to 28°C is carried out. The aorta is cross-clamped, and cold blood cardioplegic solution is administered into the aortic root. Tapes around the cavae are snared snugly and cardiopulmonary bypass is continued with low perfusion flow. The right atrium is opened through an oblique incision. A piece of autologous pericardium treated with glutaraldehyde is sewn at the anatomic level of the tricuspid valve annulus, deviating into the true right atrium in the area of the conduction system. A fenestration is created in the patch with a 4-mm coronary punch and the atrial septum is excised (Fig. 28-2).
In the past, the patch was sewn to the right atrial wall above the coronary sinus to avoid the conduction tissue. However, this resulted in increased blood flow into the excluded right ventricle and an elevated coronary venous pressure. By suturing inside the coronary sinus, injury to the conduction system can be avoided and the coronary sinus remains in the right atrium.
Before the introduction of patch fenestration, patients with pulmonic stenosis or atresia required the placement of a small pulmonary homograft between the right ventricle and pulmonary artery to decompress the right ventricle. The fenestration allows adequate decompression of the right ventricle without the use of a homograft. This simplifies and shortens the procedure, and avoids the need for reintervention on the right ventricular outflow tract.
If significant pulmonary insufficiency is present, the main pulmonary artery should be divided and the ends oversewn. This prevents the reverse flow from the systemic-pulmonary shunt into the right ventricle.
The excessively enlarged right atrium is reduced in size by excising a segment of its free wall. Depending on the extent of atrialization of the right ventricle, a plication may be performed. The atriotomy is then closed with running 6-0 Prolene sutures. The aortic cross-clamp is removed. During the rewarming phase, a 3.5- to 4.0-mm GORE-TEX interposition graft is placed from the ascending aorta to the main pulmonary artery or from the innominate to the right pulmonary artery. This shunt remains clamped until just before cardiopulmonary bypass is discontinued.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree