Fig. 30.1
Brachial artery bifurcation
Protocol
The examination is usually performed with the patient supine and the arm alongside the body where the radial artery can be easily assessed. A linear transducer in the 5–10-MHz range is often employed given that this probe is the same transducer used to examine the brachial artery. Otherwise, a transducer with higher frequencies above 10 MHz can improve resolution and visualization of this vessel, which is smaller and more superficial than the brachial artery. An expanded field of view along the radial artery facilitates transfer of information. It requires training and may take time if the artery is diseased or has an irregular course.
Some examinations should be performed in worst-case conditions. For example, if the radial artery is to be excised, the remaining collateral flow must be enough to feed the hand comfortably in conditions of severe vasoconstriction. The patient should be tested in a cold environment and perhaps a colder than usual central body temperature. This philosophy can be extended to other situations such as creation of an arteriovenous fistula or graft for dialysis. Potential for success or failure can be demonstrated. Testing in worst-case conditions does not preclude examination in normal conditions.
Alternatively, some examinations should be performed in best-case conditions. Arterial imaging improves if physiological and technical parameters are optimized. Arteries dilate and blood flow rates increase with heat. The patient then should be mapped while warm, in a warm environment, and after maneuvers to promote vasodilation such as exercise and immersing the hand in warm water.
Several technical factors facilitate imaging of small or diseased arteries:
High-frequency transducers improve resolution.
Low scale applied to color flow and duplex Doppler increases sensitivity.
Some instruments have special algorithms for detection of low velocity or low volume.
Proper steering improves color flow and duplex Doppler signals.
Increased persistence augments perception of color flow.
Ultrasonographic Changes in the Radial Artery in Systemic Disease
Duplex has been used to define anatomic changes in the radial artery in a wide array of systemic diseases. Thickness of the intima-media layer of the carotid artery has been recognized as a marker for atherosclerosis and a predictor of death and cardiovascular events in patients with coronary artery disease [2]. Although clinically relevant, upper extremity atherosclerosis is infrequent; intimal hyperplasia of the upper extremity arteries is thought to reflect global atherosclerosis (Figs. 30.2 and 30.3) [3, 4]. Ultrahigh-resolution ultrasound, also referred to as ultrasound biomicroscopy, using a 55-MHZ probe is a novel technique that enables the operator to define changes to the individual layers of smaller arteries such as the radial artery [5]. A study that compared prehypertensive and hypertensive patients with healthy subjects showed an increase of 12–14% in the thickness of the intimal layer of the radial artery, while there was no significant difference in the thickness of the medial layer [6]. Similar changes were documented in the radial artery in patients with coronary heart disease, with increase in the thickness of the intima of 19% compared to healthy subjects, with no significant changes to the thickness of the media [7]. Another study evaluated the changes in subjects with end-stage renal disease (ESRD) [8]. Compared with healthy subjects, nonhypertensive patients with ESRD had 39% thicker intima and 18% greater media in the radial artery.
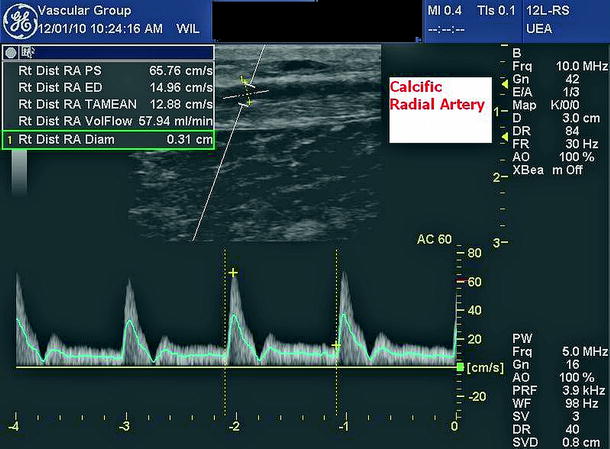
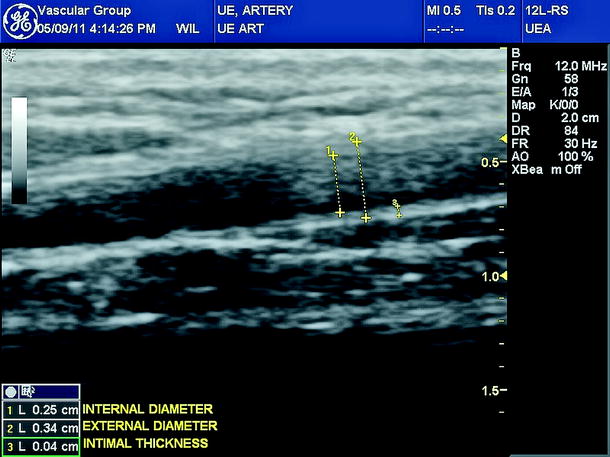
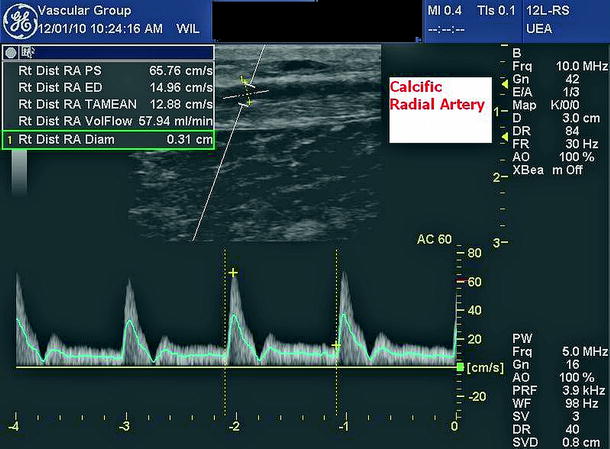
Fig. 30.2
Calcified radial artery
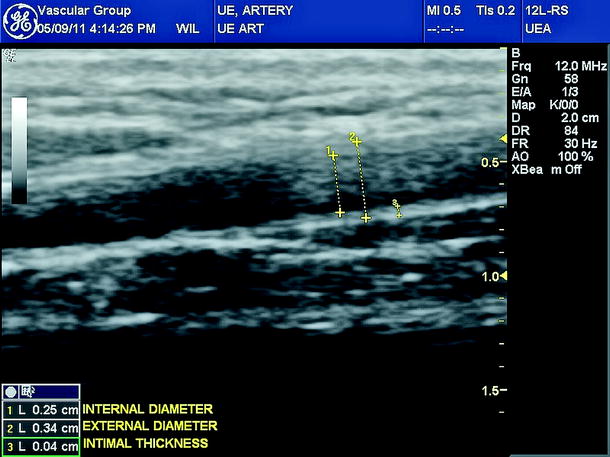
Fig. 30.3
Radial artery diameter and intimal thickness
The effect of iron overload on radial artery structure was also studied. In normotensive patients with genetic hemochromatosis, there was found an increase in radial artery wall thickness and decrease in distensibility. After iron depletion therapy, there was a decrease in wall thickness and increase in distensibility similar to the radial arteries of healthy subjects [9].
The clinical value of these assessments still needs to be evaluated, but the thickness of the intima may serve as a noninvasive tool for early detection of atherosclerosis.
Radial Artery Mapping for Coronary Bypass
Arterial mapping has been increasingly accepted prior to harvesting the radial artery for coronary bypass. Radial artery diameter and reactivity can be assessed (Fig. 30.4). The radial artery has several favorable features as a coronary graft, including a caliber similar to that of the coronary arteries, appropriate length for complete coronary revascularization, and adequate wall thickness and resistance. Presently, several cardiovascular surgeons request that vascular laboratories perform preoperative noninvasive mapping of the forearm vessels prior to radial artery harvesting to assess the suitability of the radial artery for graft replacement and to avoid ischemic complications to the hand.
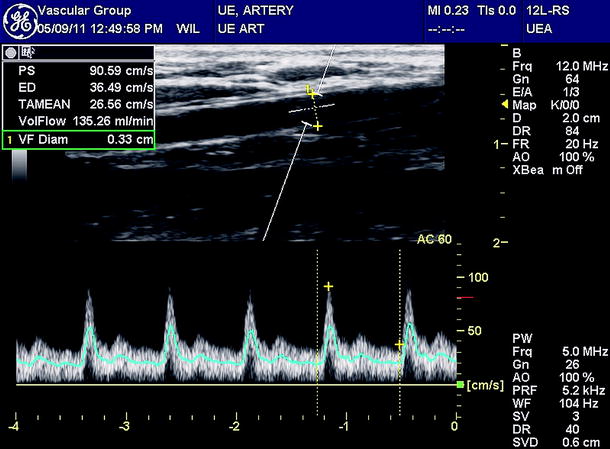
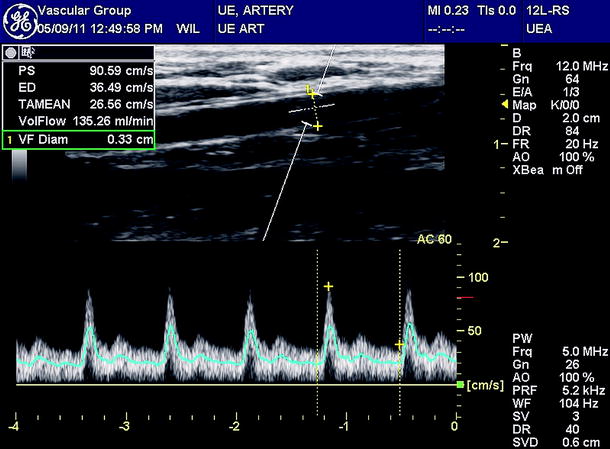
Fig. 30.4
Radial artery diameter and flow rate
Harvesting of the radial artery may occasionally lead to ischemic complications of the hand (particularly the thumb and index finger), which could be deprived of blood flow in patients with anatomical variations that do not allow adequate collateral flow across the palm. The incidence of this complication is generally low [10, 11]. There are several contraindications to using the radial artery as a graft conduit, including ischemic symptoms in the upper extremity, history of arterial trauma, and Raynaud’s syndrome. The use of the radial artery in the dominant arm is generally avoided, but this contraindication seems to be less important when adequate noninvasive evaluation conveys minimal risk. The two major objectives of this evaluation are (1) to ensure that the radial artery is free of disease and is of appropriate size and (2) to eliminate the possibility of postharvest ischemia of the hand.
The contribution of increased ulnar flow in the absence of radial artery flow has been assessed by digital pressures and other signs of increased collateral circulation. The value of increased ulnar velocities during radial artery compression remains a controversial issue [12].
The anatomic feature that permits radial artery harvesting without ischemic complications is the presence of collateral anastomosis across the palm between the radial and ulnar arteries, in the form of several arches. The most significant collateral pathway is the superficial palmar arch, which typically originates from the ulnar artery and provides the majority of arterial supply to the digits. The dorsal and deep palmar arches usually originate from the radial artery and are generally smaller than the superficial palmar arch and its branches (Fig. 30.5). Overall, if the superficial palmar arch is intact, collateral flow to the radial aspect of the hand should be adequate if the radial artery is excised. However, there are several anatomic variations that may lead to hand ischemia with radial artery harvesting, for example, incomplete superficial palmar arch, radial artery dominance of the superficial palmar arch, and absence or malformation of the ulnar artery. These variations have been reported to vary from 6% to 34% [13]. Several methods were advocated to evaluate the capability of the ulnar artery to provide adequate perfusion to the hand in the event of radial artery harvesting. These include the clinically modified Allen test, digital blood pressure measurement [14], segmental pressure measurement [15], laser Doppler flowmetry [14], pulse oximetry [16], flow measurement with photoplethysmography [16], and modified Allen test with Doppler ultrasound [10, 13, 17]. In the clinically modified Allen test, the hand is deprived of perfusion by clinching the fist and compressing the ulnar and radial arteries until the hand is exsanguinated and is then observed for return of color upon release of the ulnar artery. This test is believed to be subjective and unreliable with a significant number of false-negative and false-positive results [18]. The measurement of digital systolic blood pressure is objective, and although a pressure drop of more than 40 mmHg has been proposed as an indicator of hand ischemia, the choice of this value is somewhat arbitrary and needs validation. The measurement of oxygen saturation in the digits with radial artery compression is also objective, but substantial variations in perfusion do not always result in changes in saturation [11, 16].
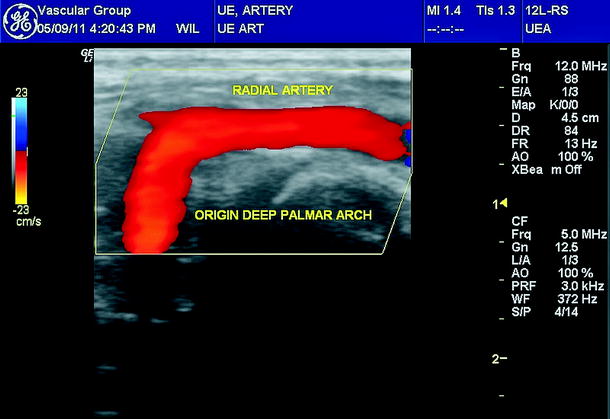
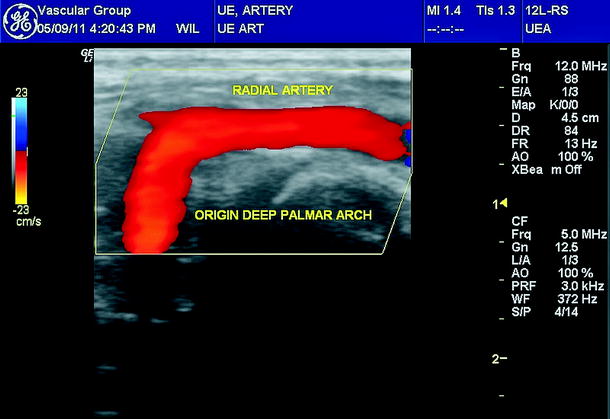
Fig. 30.5
Deep palmar arch
A Doppler ultrasound version of the clinical Allen test has been used in several studies, mostly using continuous wave Doppler ultrasound and some with color Doppler ultrasound [10, 13, 17]. This examination involves Doppler interrogation of the radial portion of the superficial palmar arch before and after radial artery compression and assessment for the presence and/or reversal of flow as an indicator of an intact arch providing adequate collateral flow [10, 13, 17]. In three previously reported studies [10, 13, 17], using the modified ultrasound Allen test with continuous-wave Doppler, in the follow-up of patients who underwent radial artery harvesting, none of the 113 patients who had negative studies (i.e., intact palmar arches) had signs of hand ischemia. Zimmerman et al. [19] examined 358 patients who underwent coronary artery bypass graft replacement, who were evaluated using modified ultrasound Allen test, and reported 53 radial arteries were harvested with no single case of hand ischemia. They began their examination with a modified ultrasound Allen test. If this test indicated that the arch was not intact, the examination was ended. If collateral flow through the ulnar artery was demonstrated, they proceeded to evaluate the radial and ulnar arteries for any evidence of obstructive disease or atherosclerosis.
The ultrasound Allen test utilizes a 7- to 10-MHz linear transducer that is placed in the crease of the proximal palm at the base of the thumb. The superficial palmar arch of the radial artery can be identified coursing anteriorly at this location. The approximate location of this vessel can generally be found by drawing a line along the longitudinal axis of the center of the index finger to the point of its intersection with the crease at the base of the thumb or the thenar eminence. Flow in this artery is normally directed toward the transducer and into the superficial palmar arch. The direction of flow in this artery can be easily determined by using color Doppler ultrasound. Color Doppler ultrasound is generally employed to locate the artery and spectral imaging to evaluate and document the change in flow direction. While the superficial palmar arch is insonated, the radial artery is compressed at the wrist, and the ultrasonographer watches for a reversal of flow, implying that the arch is complete, or lack of flow, implying that the arch is incomplete. Reversal of flow implies that the radial artery may be harvested with safety. Complete lack of flow in this artery with compression essentially precludes the use of the ipsilateral radial artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


