Described herein are certain findings in 2 male cousins who underwent cardiac transplantation for severe heart failure (HF), one of the diastolic type (ejection fraction ≈65%), and one of the systolic type (ejection fraction ≈20%), both the consequence of hypertrophic cardiomyopathy (HC), and each had identical disease-causing gene mutations. The implanted heart in one had normal-sized ventricular cavities and no grossly visible ventricular wall lesions (except in one papillary muscle) and the other patient had severely dilated ventricular cavities and multiple extensive ventricular wall scars. The heart mass and the age of onset of symptoms was similar in each patient. A number of other family members had evidence of HC.
Hypertrophic cardiomyopathy (HC) is a genetically transmitted cardiac disease with a diverse variety of clinical and morphologic manifestations. Its frequency of 1 in 500 persons is similar to that of familial hypercholesterolemia. Some patients with HC remain asymptomatic or nearly so throughout a long life; others die suddenly, usually prematurely; many have symptoms related to left ventricular outflow obstruction and once the obstruction is relieved the symptoms vanish or at least decrease in frequency, and some patients develop end-stage HF that can be relieved only by cardiac transplantation (CT). Recently, we encountered 2 male cousins with HC, both of whom underwent CT, and examination of the recipient heart disclosed nearly opposite morphologic features of the disease although both had identical disease-causing gene mutations. A description of certain findings in them is the purpose of this report.
Patient Descriptions
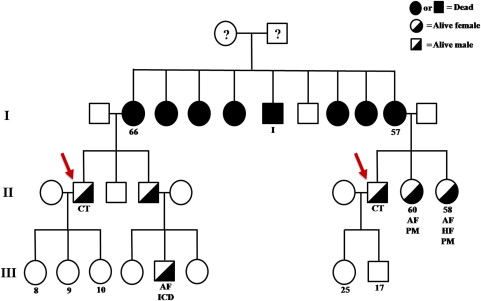
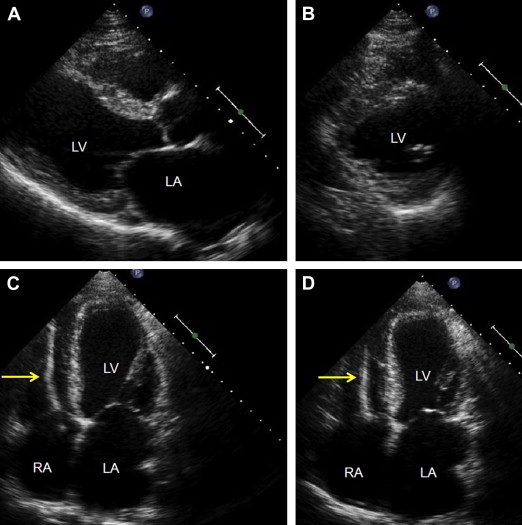
Pertinent clinical and morphologic findings in the 2 patients are tabulated in Table 1 . The pedigrees of the family are illustrated in Figure 1 . Both were African American men, one had CT at age 45 and the other, at age 48 years. One became symptomatic from HF about 6 years before CT, the other 7 years, before CT. Both had class IV HF. Each also had one or more episodes of syncope, atrial fibrillation, and runs of ventricular tachycardia. Neither had a precordial murmur. Neither had obstruction to outflow from either the right or left ventricle. Both had normal epicardial coronary arteries. The left ventricular ejection fractions were strikingly different. In case #1 it was ≈65%, and in case #2, ≈20%. Both patients had elevated pulmonary arterial pressures. Both had cardiac defibrillators implanted several years before CT. Patient #2 had a left ventricular assist device. Echocardiograms before CT are shown in Figures 2–4 .
| Variable | Case #1 | Case #2 |
|---|---|---|
| Age (yrs) at cardiac transplantation | 45 | 48 |
| Age (yrs) onset symptoms | 39 | 41 |
| Heart failure class IV | + | + |
| Chest pain | 0 | + |
| Syncope | + | + |
| Precordial murmur | 0 | 0 |
| Atrial fibrillation | + | + |
| Ventricular tachycardia | + | + |
| Body mass index (Kg/m²) | 26.5 | 30.6 |
| Left ventricular ejection fraction | 65% | 20% |
| Cardiac index (l/min/m²) | 1.3 | 1.8 |
| Pulmonary artery peak systolic pressure (mm Hg) | 82 | 56 |
| Coronary narrowing by angiogram | 0 | 0 |
| Left ventricular assist device inserted | 0 | + |
| Heart weight (g) | 410 | 410 |
| Scars (0-4+), left ventricular wall and ventricular septum | 0 ∗ | +(4+) |
| Dilated right ventricle | 0 | + |
| Dilated left ventricle | 0 | + |
| Mitral valve | normal | normal |
| Mural endocardial thickening in the left ventricular outflow tract in apposition to anterior mitral leaflet | 0 | 0 |
| Mitral annular calcium | 3+/4+ | 0 |
| Abnormal intramural coronary arteries | 0 | + |