Hypertrophic cardiomyopathy (HC) is the most common cause of sudden death in the young but a relatively uncommon disease in clinical practice. Therefore, even the experiences of individual cardiologists and patients can be particularly instructive, by unexpectedly opening windows to this disease not previously fully appreciated. Such is the subject of this essay.
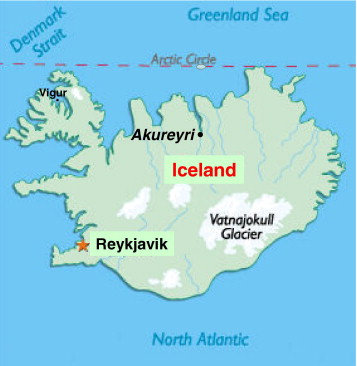
The ancestry of Gunnar Thor Gunnarsson (age 44 years; Figure 1 ) is in the Icelandic town of Akureyri, just 55 mi (90 km) south of the Arctic Circle and the northernmost and now second largest city in the country (population 30,000; Figure 2 ). In November 2001, his oldest child collapsed and died suddenly at 10 years of age while walking with her father. Although by chance, this event occurred at the entrance to a children’s hospital emergency room, and cardiopulmonary resuscitation and defibrillation were exceedingly rapid, it was not possible to restore normal heart rhythm. She had been asymptomatic, active, and healthy, and there was no family history of cardiac disease or premature sudden death. At autopsy, massive left ventricular hypertrophy (septal thickness 30 mm) was identified, diagnostic of HC, and also a risk marker for sudden death in this disease. Genetic testing revealed compound β-myosin heavy chain mutations (Arg453Cys and Cys947Arg). Because neither parent nor 2 other daughters carry this mutation, it can be assumed that this sudden death was associated with a de novo genetic defect that has now been extinguished in the family.

Returning to cardiovascular practice as 1 of 2 cardiologists in Akureyri, Dr. Gunnarsson was faced not only with a family tragedy but also a difficult professional dilemma: should he (or could he) avoid patients with HC in his practice? Would that be best for himself and his patients? Could he be objective in providing recommendations and clinical decisions in light of his own tragic personal experience? Furthermore, did he really have the necessary expertise, considering that he had previously treated only 1 patient with HC, as a cardiology trainee in Sweden (who coincidentally had died suddenly several years later)? Who among us would have been critical if he had shunted to a colleague other patients with HC, the disease that was responsible for his daughter’s death?
Dr. Gunnarsson selected another path, ultimately deciding that he knew as much as anyone about the unpredictable nature of HC, and began to recruit (and be sought out by) patients with HC in northern Iceland. Soon he was following almost 20 such patients, a number approaching the expected prevalence of the disease in that region. One of those patients was an active woman with nonobstructive HC, first evaluated at 43 years of age, who had experienced several episodes of syncope unassociated with physical exertion in the preceding days. Unexplained recent syncope is 1 of the 5 conventional HC primary prevention risk markers and is associated with a high rate of appropriate implantable cardioverter-defibrillator (ICD) interventions in patients implanted prophylactically for only 1 risk factor.
After some consideration, Dr. Gunnarsson recommended a prophylactic ICD, a somewhat unusual decision in Iceland given that it was only the sixth device implanted nationwide for HC (n = 100 currently for all diseases), in a culture that embodies considerable acceptance of the natural risks of living. Five uneventful years followed. Then, at 48 years of age, while hiking on the small, remote island of Vigur in western Iceland ( Figure 2 ), 1.5 hours by boat to the nearest hospital, this young woman experienced an episode of syncope associated with a rapid monomorphic ventricular tachycardia (rate 260 beats/min) deteriorating to ventricular fibrillation, and was immediately restored to sinus rhythm by a single defibrillation shock—that is, an aborted sudden death event. So, remarkably it had come full circle—from his very young daughter to this woman, all within the 8-year experience of 1 physician.
This story is not being told solely for its dramatic impact but rather because it is about redemption in medicine, reflects an evolving awareness of the natural history of HC, and underscores important principles of disease management, specifically the potential for the prevention of sudden death by using the power of an ICD. Also, these events link Iceland and HC, thereby underscoring the truly global nature of this disease, capable of striking unpredictably virtually anywhere in the world, as well as the far-reaching penetration of medical technology.
Gunnar Thor Gunnarsson elected to focus his energies on HC because of his personal experience with the unpredictable risk profile in this disease. Most importantly, he was open to the prevailing view that 1 major risk factor in a young patient can be sufficient to recommend the option of a prophylactic ICD. As a result, a sequence of events ultimately evolved in which a personal tragedy was translated into a lifesaving intervention for a HC patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


