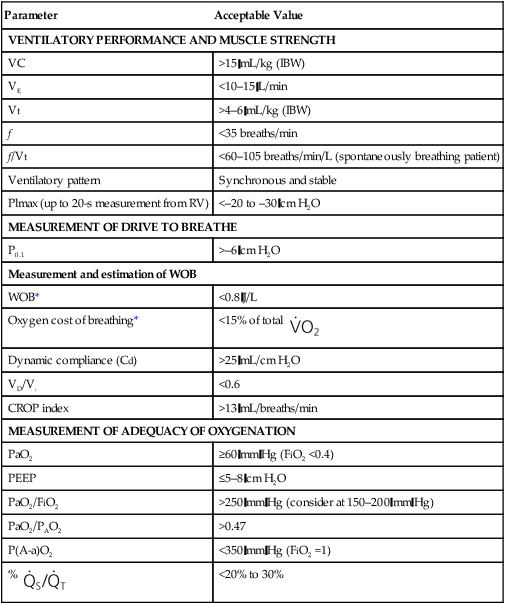
1. Evaluate a patient for readiness for a spontaneous breathing trial. 2. Perform a spontaneous breathing trial procedure. 3. Describe the guidelines for extubation. 4. List the acceptable weaning indices used to predict a patient’s readiness for discontinuation of ventilatory support. 5. Determine an appropriate weaning mode for a patient. 6. Perform the weaning procedure. 7. Describe factors that may lead to ventilator dependence. Removing a patient from ventilatory support may range from a routine procedure that takes minutes to the need for a systematic approach that takes days to weeks. However rapid or time consuming the undertaking, discontinuation of ventilatory support requires the evaluation of a patient’s physiologic and psychological status and, at times, even requires ethical considerations. Physiologic parameters for weaning and extubation are provided in Table 25-1. TABLE 25-1 Physiologic Parameters for Weaning and Extubation of Adults *Actual measure of work of breathing (WOB). (From Cairo JM: Pilbeam’s mechanical ventilation, ed 5, St. Louis, 2011, MO, Mosby.) Supporting a patient during an exacerbation of a chronic pulmonary condition or an acute pulmonary illness at times requires mechanical ventilation. It is not, however, without consequences. These could range from airway damage such as tracheal stenosis to ventilator dependence, defined as the need for ventilatory support for lengthy periods, usually longer than 2 weeks. Discontinuing ventilatory support is a complex issue. Both premature discontinuation and delayed discontinuation of ventilatory support are associated with adverse patient outcomes. A way to test a patient’s readiness for successful discontinuation of mechanical ventilatory support is a SBT. Extubation should be considered but not integrated into the SBT process. Guidelines for extubation are provided in Box 25-1. The following is the step-by-step process for a spontaneous breathing trial. 1. Review the patient’s chart. 2. Verify the physician’s order or the facility’s protocol for standard of care. 3. Obtain, clean, and inspect the appropriate equipment prior to entering the patient’s room. 4. Follow personal protective equipment (PPE) requirements, and observe standard precautions for any transmission-based isolation procedure. 5. Identify the patient using two patient identifiers. 6. Introduce yourself to the patient and to the family. 7. Explain the procedure to the patient and to the family, and acknowledge the patient’s understanding. 8. Perform proper hand hygiene, and put on gloves, mask, and protective eyewear, as appropriate for the procedure. 1. Place the patient in a comfortable position. 3. Assess the patient for SBT readiness, including the following: 4. Record the patient’s baseline values: 5. Advise the patient when the SBT will commence. 6. Change the ventilator to a spontaneous mode with zero pressure support ventilation (PSV) and zero continuous positive airway pressure (CPAP): a. Minimal CPAP settings may be used, per facility protocols. b. Minimal PSV settings may be used, per facility protocols. 7. Maintain the fractional inspired oxygen (FiO2) that the patient was receiving on mechanical ventilation. 8. Monitor and record the SBT start data, including the following:
Discontinuing Ventilatory Support
Parameter
Acceptable Value
VENTILATORY PERFORMANCE AND MUSCLE STRENGTH
VC
>15 mL/kg (IBW)
VE
<10–15 L/min
Vt
>4–6 mL/kg (IBW)
f
<35 breaths/min
f/Vt
<60–105 breaths/min/L (spontaneously breathing patient)
Ventilatory pattern
Synchronous and stable
Plmax (up to 20-s measurement from RV)
<–20 to –30 cm H2O
MEASUREMENT OF DRIVE TO BREATHE
P0.1
>–6 cm H2O
Measurement and estimation of WOB
WOB*
<0.8 J/L
Oxygen cost of breathing*
<15% of total 
Dynamic compliance (Cd)
>25 mL/cm H2O
VD/Vt
<0.6
CROP index
>13 mL/breaths/min
MEASUREMENT OF ADEQUACY OF OXYGENATION
PaO2
≥60 mm Hg (FiO2 <0.4)
PEEP
≤5–8 cm H2O
PaO2/FiO2
>250 mm Hg (consider at 150–200 mm Hg)
PaO2/PAO2
>0.47
P(A-a)O2
<350 mm Hg (FiO2 =1)
% 
<20% to 30%
» Skill Check Lists
25-1 Implementing a Spontaneous Breathing Trial
Procedural Preparation
Implementation















 , minute ventilation;
, minute ventilation;  , oxygen (O2) consumption per minute; V
, oxygen (O2) consumption per minute; V

