Dilation of the ascending aorta (AA) is common in patients with a bicuspid aortic valve. The natural history of the aortic root and AA and the risk factors for dilation have not been characterized in patients with congenital aortic stenosis (AS) treated with balloon valvuloplasty during childhood. The present study was performed to determine the prevalence of aortic dilation in patients with congenital AS before and up to 20 years after balloon valvuloplasty performed during childhood. In patients who underwent balloon valvuloplasty for AS at age ≤18 years from 1984 to 2005, the aortic diameter measurements before intervention and at 5-year intervals afterward were recorded and the Z scores calculated. Among 156 patients (median age 1.5 years at valvuloplasty), the AA Z scores were significantly larger than normal before intervention (median Z score 1.5) and at all follow-up points (all p <0.001). Using mixed modeling, with time as a categorical variable (before intervention, 5-year window, 10-year window, and so forth), the mean AA Z score was greater at all postvalvuloplasty points than before the intervention, with mean Z score increases of 1.20 at 5 years and 2.11 at 20 years (p <0.001). Moderate or greater aortic regurgitation early after valvuloplasty was associated with greater AA Z scores than mild or less aortic regurgitation, with a progressive difference over time. More significant residual AS after valvuloplasty was associated with lower AA Z scores over time. In conclusion, AA dilation is common in children with congenital AS and continues to progress over many years after balloon valvuloplasty.
Dilation of the aortic root and ascending aorta (AA) is a common and frequently progressive finding in adults and children with a bicuspid aortic valve (BAV). Aortic dilation in the setting of a BAV tends to be more severe and to progress more rapidly in older patients and in those with hypertension; however, data are conflicting about the risks of aortic dilation and progression according to leaflet morphology and the severity of aortic valve stenosis (AS) and aortic regurgitation (AR). Although there have been inconsistent findings regarding the relations between aortic dilation and both AS and AR in patients with a BAV, no published data are available specifically concerning the natural history of the AA and aortic root in children and adolescents with important congenital AS and/or postintervention AR. The characterization of the aortic dimensions and growth in children with aortic valve disease could help inform a better understanding of how they should be evaluated and managed. Given that residual and recurrent AS and AR are relatively common after balloon valvuloplasty in children and that the valve morphology is abnormal, the relation between these factors and aortic growth in the long term could facilitate an improved understanding of this complex patient population.
Methods
We studied all patients who underwent balloon aortic valvuloplasty at Children’s Hospital Boston at ≤18 years of age from December 1984 through February 2005 (to allow ≥4 years of follow-up), had undergone precatheterization echocardiography at our institution within 6 months of the procedure, and had ≥1 follow-up echocardiogram at our institution ≥4 years after balloon valvuloplasty. These patients were drawn from a larger cohort analyzed for a study of reintervention after balloon aortic valvuloplasty. The follow-up echocardiographic data were collected at 5-year intervals, with 1- to 2-year windows on either side (4 to 6, 8 to 12, 13 to 17, and 18 to 22 years). The patients were not required to have data in consecutive follow-up windows, such that follow-up data availability varied (e.g., some patients could have had data at all points, others 10-year data only, others 5- and 20-year data). For patients with multiple echocardiograms within 1 window, the study closest to the 5-year interval that included adequate selected. For patients who underwent aortic or aortic valve surgery during follow-up, the echocardiographic data were included up to, but not after, the surgery. The patients who underwent repeat balloon aortic valvuloplasty were included.
The maximal systolic diameters of the aortic annulus, aortic root, and AA were measured off-line using a standard method, at peak flow during midsystole, from the parasternal long-axis, high left parasternal, or high right parasternal views. The AA was typically measured at the level of the right pulmonary artery, although in patients with atypical dilation, the maximum diameter of the AA was used regardless of location. The aortic annulus, aortic root, and AA Z scores were calculated on the basis of normative data obtained at our center. Valve morphology was characterized as unicommissural (unicuspid), bicommissural (bicuspid), or tricommissural (tricuspid) and by the commissures that were fused or underdeveloped. Valves with fusion or underdevelopment of 1 commissure and minor partial fusion of another were classified as bicommissural; those with complete fusion of 2 commissures or significant fusion of all 3 commissures were considered unicommissural.
The degree of AR was measured on the first available echocardiogram within 1 year after balloon valvuloplasty according to standard methods, including vena contracta width in the orthogonal planes, the presence of left ventricular dilation, and the presence/degree of retrograde diastolic flow in the abdominal aortic Doppler pattern. AR severity was taken from the report of the interpreting noninvasive cardiologist and was collapsed into 2 categories thought to represent a clinically relevant delineation (less than moderate or moderate or greater) for the purposes of the analysis. Angiographic grading of AR was used for the analysis in 7 patients who did not have a postcatheterization echocardiogram within 1 year. The pre- and postdilation peak AS gradients, as measured in the catheterization laboratory, were used for analysis.
The aortic Z scores were compared with normal (Z = 0) using 1-sample t test. A comparison of the baseline aortic dimensions using the demographic and diagnostic features was performed using an independent samples t test. The categorical variables were compared between groups using chi-square analysis. The changes in aortic dimensions over time were characterized using linear mixed effects models, which accounted for the correlation among repeated measurements of the same subject. Individual patients were treated as random effects, and additional clinical covariates were treated as fixed effects. If changes in the aortic dimensions over time were not linear, the quadratic and piecewise relations were explored. The rates of change in the aortic Z scores using this analytic approach reflect the average change across patients over time. When statistically significant relations between the aortic dimensions and clinical covariates were identified, interaction terms were used to determine whether the trends over time differed between the patient groups. The data are presented as the mean ± SD, median (minimum to maximum), or frequencies.
Results
The study cohort included 156 patients, whose demographic, diagnostic, and procedural data are summarized in Table 1 . The median duration from the precatheterization echocardiogram to balloon valvuloplasty was 1 day (range 0 days to 6 months). An average of 1.8 ± 0.9 follow-up studies were evaluated per patient, with 112 patients studied in the 5-year window, 78 in the 10-year window, 47 in the 15-year window, and 16 in the 20-year window. Patients often had data in nonconsecutive follow-up windows; thus, a total of 95 patients had data at ≥10 years and 53 had data at ≥15 years.
| Characteristic | Value |
|---|---|
| Age at balloon aortic valvuloplasty (years) | |
| Median | 1.5 |
| Range (minimum to maximum) | 1 day to 16.4 years |
| Neonates (age <1 mo) | 49 (31%) |
| Infants (age 1–12 mo) | 77 (49%) |
| Aortic valve morphology | |
| Unicommissural | 54 (35%) |
| Left–right and right–noncommissural fusion | 50 |
| Left–right and left–noncommissural fusion | 1 |
| Substantial fusion of all 3 commissures | 3 |
| Bicommissural | 102 (65%) |
| Left–right commissural fusion | 60 |
| Right–noncommissural fusion | 42 |
| Peak aortic stenosis gradient (mm Hg) | |
| Before valvuloplasty | 66.6 ± 2.0 |
| Acutely after valvuloplasty | 29.3 ± 14.4 |
| Aortic regurgitation severity acutely after valvuloplasty | |
| None or trivial | 78 (50%) |
| Mild | 51 (33%) |
| Moderate to severe | 27 (17%) |
| Associated cardiovascular anomalies | 41 (26%) |
| Previous cardiovascular interventions | 32 (21%) |
| Surgical or balloon aortic valvuloplasty | 12 (8%) |
| Aortic arch repair | 20 (13%) |
| Ventricular septal defect closure | 9 (6%) |
| Subaortic stenosis resection | 7 (4%) |
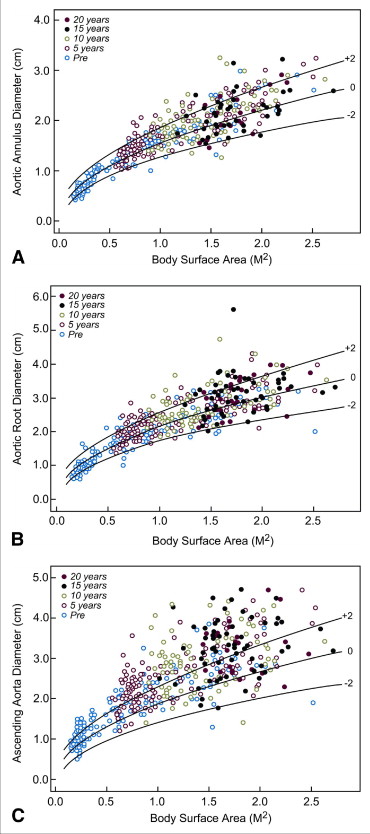
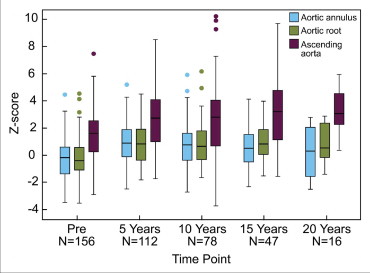
The AA Z scores were larger than normal before intervention and at all follow-up points ( Table 2 ). Although not significantly different from normal before the intervention, the aortic annulus and root Z scores were larger than normal at all follow-up points, except the 20-year window ( Table 2 ). Figure 1 depicts the aortic dimensions plotted against the body surface area, and Figure 2 shows the aortic Z scores in each of the evaluation windows. The AA was dilated (larger than normal, Z score >2) before valvuloplasty in 49 patients (31%) and became dilated during follow-up in another 48 (total 62%). The aortic root was dilated before intervention in 10 patients (6%) and progressed to a dilated state during follow-up in 28 (total 24%).
| Variable | Before Balloon Valvuloplasty (n = 156) | Follow-up Interval (years) | |||
|---|---|---|---|---|---|
| 5 (n = 112) | 10 (n = 78) | 15 (n = 47) | 20 (n = 16) | ||
| Aortic annulus Z score | |||||
| Mean ± SD | −0.3 ± 1.5 | 1.0 ± 1.5 | 0.8 ± 1.6 | 0.5 ± 1.5 | 0.3 ± 1.9 |
| Mean difference ⁎ | +1.18 | +1.05 | +0.62 | +0.70 | |
| Aortic root Z score | |||||
| Mean ± SD | −0.2 ± 1.5 | 0.8 ± 1.4 | 0.8 ± 1.6 | 0.9 ± 1.3 | 0.7 ± 1.5 |
| Mean difference ⁎ | +0.93 | +0.89 | +0.98 | +1.01 | |
| Ascending aorta Z score | |||||
| Mean ± SD | 1.5 ± 1.6 | 2.6 ± 2.2 | 2.6 ± 2.7 | 3.1 ± 2.5 | 2.6 ± 2.1 |
| Mean difference ⁎ | +1.20 | +1.21 | +1.73 | +2.11 | |
Before intervention, the patients with a unicommissural aortic valve had smaller aortic annulus Z scores than those with a bicommissural valve (−1.0 ± 1.5 vs 0.1 ± 1.3, p <0.001), and a trend was seen toward smaller aortic root Z scores (−0.5 ± 1.8 vs 0.0 ± 1.2, p = 0.07). However, no difference was found in the AA Z scores (1.6 ± 1.7 vs 1.4 ± 1.6, p = 0.5). Patients who had undergone previous aortic coarctation repair had significantly smaller AA Z scores before valvuloplasty than those without arch obstruction (0.5 ± 1.2 vs 1.6 ± 1.6, p = 0.004). However, no differences were found in the annulus or root Z scores. Among patients with a bicommissural valve, no differences were found in the aortic Z scores according to the patterns of commissural fusion. None of the other demographic or diagnostic variables assessed were associated with significant differences in the preintervention aortic annulus, aortic root, or AA Z scores.
Using mixed modeling with time as a categorical variable (before intervention, 5-year window, and so forth), the mean AA Z score was greater at all postvalvuloplasty points than before intervention (all p <0.001; Table 2 ). Quadratic and piecewise linear models fit the data better than a linear approach and showed a progressively increasing AA Z score over time. Using a piecewise model, the slope was steeper between the preintervention and 5-year window than later; however, the increase remained significant beyond 5 years (p = 0.017). The AA Z scores at all points tended to be greater in the patients with higher preintervention Z scores, but there was a significant interaction with time, such that the rate of increase was significantly greater for patients with lower preintervention Z scores. When the preintervention AA Z score was dichotomized, those with a Z score <1 had significant increases over time, and there was a very modest and statistically insignificant increase among patients with a baseline Z score of ≥1 ( Figure 3 ).
Moderate or greater AR early after valvuloplasty was associated with greater AA Z scores than was mild or less AR, with a progressive difference over time (p = 0.04 for interaction with time; Figure 3 ). No difference was seen before valvuloplasty. In contrast, more significant residual AS early after valvuloplasty was associated with lower AA Z scores over time (for each 10-mm Hg increase in the gradient, the AA Z score was lower by −0.20 on average; p = 0.05). The AA Z scores were also lower in patients with cardiovascular anomalies, in addition to AS (mean difference −1.06, p = 0.001), and those who had undergone treatment of coarctation of the aorta (mean difference −1.19, p = 0.004) or any cardiovascular intervention before valvuloplasty (mean difference −1.34, p <0.001), consistently across all points (i.e., no interaction with time). Valve morphology, age at intervention, preintervention AS gradient, and previous balloon aortic valvuloplasty were not significantly related to the AA Z score.
Treating time as a categorical variable, the mean aortic root Z score was greater at all postvalvuloplasty points than before intervention (all p <0.001; Table 2 ). Piecewise linear modeling provided the best fit for the data, demonstrating a significant increase in the aortic root Z score from before intervention to the 5-year window (p <0.001) but a flat slope from 5 to 20 years (p = 0.8). No statistically significant relation was found between the aortic root Z score and age at balloon dilation (p = 0.3), valve morphology (p = 0.9), or severity of postvalvuloplasty AR (p = 0.2).
Treating time as a categorical variable, the mean aortic annulus diameter Z score was greater at all postvalvuloplasty evaluation windows than before intervention (p <0.001 for 5 and 10 years, p = 0.005 for 15 years, and p = 0.04 for 20 years; Table 2 ). The best fit for the data were achieved with piecewise linear modeling, which demonstrated a significant increase in the aortic annulus Z score from before intervention to the 5-year window (p <0.001) but a slightly negative slope from 5 to 20 years (p = 0.03). The mean aortic annulus Z scores were greater for patients with a bicommissural valve across all points (mean difference 0.57, p = 0.002), but no significant interaction was seen with time. The aortic annulus Z scores were also greater across time in patients with moderate or greater AR early after valvuloplasty (mean difference 0.95, p <0.001), and patients who were older at the intervention (mean difference 0.07 for each additional year of age, p <0.001). No significant interactions were found for either of these relations.
Of the 156 patients in the present cohort, none were known to develop aortic dissection or rupture or to die from suspected complications related to AA dilation or disease. However, 7 underwent surgery for a dilated or aneurysmal AA a median of 11.8 years (range 9.9 to 22.4) after balloon aortic valvuloplasty. In 5 of these patients, the primary indication for surgery was aortic valve disease (mixed disease with predominant AR). The aortic valve was repaired at AA surgery in 3 of these patients and replaced in 2. The aortic valve had been repaired 6 years earlier in the patient who underwent aneurysmorrhaphy. The AA surgery consisted of supracoronary replacement with a 21- to 30-mm Dacron tube graft in 6 (median age 16.7 years, range 9.9 to 23.6) and a vertical plication aneurysmorrhaphy without cardiopulmonary bypass in 1 (age 12 years). The median preoperative AA diameter in these 7 patients was 4.5 cm (range 3.7 to 4.9 cm), and the median AA Z score was 7.3 (range 5.9 to 11.5). No operative deaths or major adverse events were recorded. Histopathologic findings were available for the resected segment of the aorta in the 6 patients who had undergone replacement and revealed cystic medial degeneration in all cases. During a median follow-up of 4.1 years (range 0.7 to 6.9) after AA surgery, none of these patients had undergone reintervention on the aorta or valve. One patient had mild-to-moderate AR, and the others had mild or less. At a follow-up examination 6.9 years after surgery, the AA diameter was 4.1 cm ( Z score 4.6) in the patient who had undergone aneurysmorrhaphy compared to 4.5 cm ( Z score 11.5) before and 3.3 cm ( Z score 5.4) 6 months after surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


