
FIGURE 33.1. A,Polytetrafluoroethylene tubing used in early Scribner shunts. One side was placed in an artery (typically the radial or posterior tibial artery) and the other into an accompanying vein. The tubes exited the skin where they were connected to the dialysis machine or to each other when not in use. B,A Scribner shunt in place at the ankle.
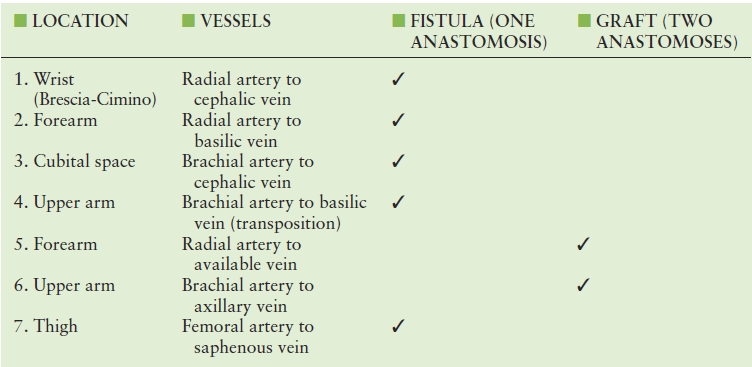
TABLE 33.1 Common Hemodialysis Access Types
When prosthetic grafts were developed for arterial bypass, it became obvious that these devices could substitute for veins as sites for access to the circulation. Most materials used for bypass grafts, such as Dacron, ePTFE, umbilical veins, and bovine carotid arteries, have been used for dialysis access. Of these, ePTFE has become the material of choice owing to its ease of placement and puncture and its relative durability.5 Despite the many advantages of prosthetic grafts (Table 33.2), they are more prone to infection than native vessels and half fail within 1 year of placement. Native arteriovenous fistulas are preferred to prosthetic grafts not only because they have better patency rates and fewer infections but also because they require fewer secondary procedures to maintain patency. Traditionally, the United States has had particularly low rates for placement of native arteriovenous fistulas. In 2002, the percentage of new access sites that used native fistulas was only 32% in the United States whereas it was 80% in Japan and 70% in Europe. The factors that influenced the preference for ePTFE include a high rate of maturation failure in native fistulas, late referral to the surgeon, urgent need for dialysis, inadequacy of upper extremity veins, and reimbursement incentives.
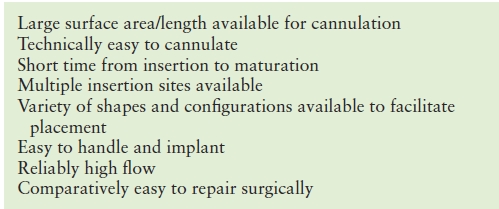
TABLE 33.2 Advantages of Prosthetic Grafts for Dialysis Access
Patients who are referred late in the course of their illness often need dialysis urgently and frequently do not have suitable veins for arteriovenous fistula creation because no one has thought to preserve their superficial upper extremity veins. Prosthetic grafts are favored in this situation because they do not require the lengthy maturation times of native fistulas; some of these devices can be accessed on the day of surgery. Reimbursement patterns also favor prosthetic grafts because their placement is reimbursed at a higher rate than creation of most arteriovenous fistulas. Prosthetic grafts are now being considered as a reasonable option in elderly patients and for use before resorting to the upper arm basilic vein transposition, which has increased morbidity compared with simpler native fistulas.6
For the reasons given previously, there has been a major initiative by the National Kidney Foundation (NKF) to encourage greater use of native arteriovenous fistulas for dialysis access in the United States. The Kidney Disease Outcomes Quality Initiative (KDOQI) by the NKF and the Fistula First initiative by the Centers for Medicaid and Medicare Services have been successful in improving these numbers. Their goal is at least 65% use of native arteriovenous fistulas. One of the prime components of this initiative is the use of preoperative duplex scanning. The use of native vessels for creation of dialysis access has improved in the United States from 31% in 2003 to 44% by the end of 2006, and some centers are reporting rates up to 90%. These improvements have been attributed to many practice and educational factors such as encouraging early referral of patients with kidney disease before their veins have been depleted by multiple phlebotomies, awareness of the advantages of native fistulas by surgeons, use of deep veins that require transposition to a more superficial location (primarily basilic vein transposition), and improved reimbursement for creation of complex arteriovenous fistulas. The use of preoperative duplex scanning has also facilitated the placement of native fistulas by identifying suitable veins that are not evident on physical examination, confirming the patency of the central veins, and ensuring the adequacy of arterial inflow.
PREDIALYSIS ACCESS PLANNING
The main principle of access planning is to preserve as many veins as possible for subsequent use when the access fistula or device stops working, which inevitably will happen if the patient lives long enough. Thus, the surgeon works from the most distal location possible to more central locations, starting with the nondominant upper extremity, then the dominant upper extremity, then more unusual locations such as the femoral or axillary arteries. Native arteriovenous fistulas are used first whenever possible, then prosthetic material at each level. The order of preferred access procedures is typically a wrist or snuffbox fistula between the radial artery and the cephalic vein (the snuffbox is the space between the extensor hallucis longus and the extensor pollicis brevis at the base of the thumb, where a distal branch of the radial artery and the cephalic vein lie in close proximity), a brachial artery-to-cephalic vein fistula at the elbow, and finally a transposition of the basilic vein in the arm to the brachial artery (note that the “arm” is the proper anatomic term for what is frequently referred to as the “upper arm”). There are many variations on this theme that can be used by the creative surgeon. For example, the basilic vein in the forearm, which runs too dorsally for use in dialysis, may be transposed and connected to the radial artery, or the median antebrachial vein may be connected in a side-to-side fashion in the upper forearm to the radial artery with lysis of vein valves allowing reverse flow through this vein into the forearm venous system.7 These unusual procedures can produce complicated anatomy, which should be diagramed by the surgeon to allow the dialysis technicians and sonographers to understand the anatomy when placing the patient on dialysis or studying the fistula for possible abnormalities (Fig. 33.2).

FIGURE 33.2 A proximal radial artery arteriovenous fistula with skin markings to indicate the path of flow, which is bidirectional in this case. Such diagrams are useful for both the dialysis technicians who access the fistula and the sonographers who scan them.
(Courtesy of William C. Jennings, M.D.)
The main purpose of preoperative duplex scanning is to confirm the patency and determine the size of the cephalic and basilic veins in the upper extremity. Many studies have shown that the main predictor of success for a new access is the size of the outflow vein. Most authors state that a minimum diameter of 2.5 mm is required for a reasonable chance of successful maturation for a native arteriovenous fistula, although some now suggest that the failure rate is unacceptable for veins below 3 mm. A vein diameter of at least 3 mm, and preferably 4 mm or greater, is required for a prosthetic graft. In addition to having an adequate caliber, veins must be superficial enough for ease of puncture. Veins deeper than 6 mm from the skin surface are difficult to access unless they are exceptionally large. Thus, depth is an important consideration. Excessive depth does not preclude use of the vein but often requires the surgeon to “superficialize” it—surgically transposing it to a more superficial location. Patency of the central veins should also be assessed, especially in patients who have had prior access through central venous catheters.
A complete evaluation must include the arterial supply to the extremity. Renal failure patients are particularly prone to develop calcification of their arteries due to secondary hyperparathyroidism and an imbalance of calcium and phosphate. Heavily calcified arteries may not be suitable for access use owing to the difficulty in suturing these vessels. These patients develop occlusive disease in arteries from the aortic branches all the way to the digital vessels, which can result in inadequate flow for successful dialysis. Arterial occlusive disease also places patients at increased risk for clinically significant steal that can cause irreversible pain, loss of sensation, and weakness in the hand, as discussed later in this chapter. A preoperative digit-brachial pressure index of less than 0.6 should raise concern for the risk of steal. Some examiners check the response to hyperemia created by simple fist clenching. There should be an increase in diastolic flow with release of the clenched fist. Absence of this response suggests lack of reserve and increased risk for steal.
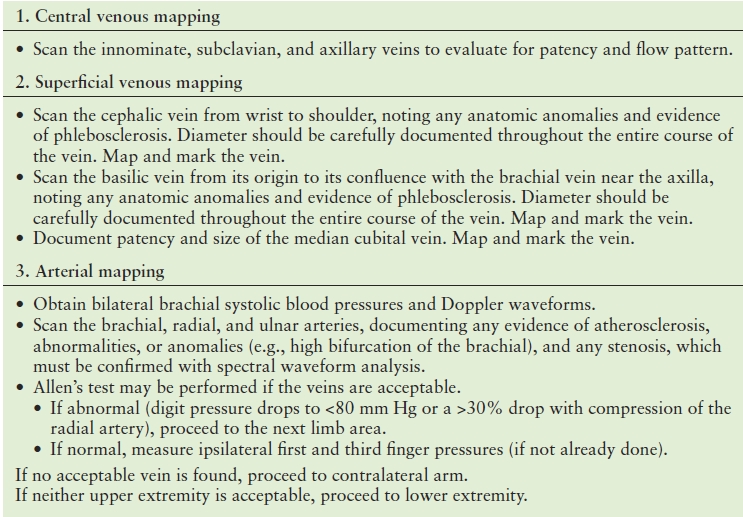
As described in Table 33.3, a predialysis access duplex mapping examination consists of three main components: (1) central venous mapping, (2) superficial venous mapping, and (3) arterial mapping. Specific mapping protocols should be developed at each facility by the local vascular technologists and access surgeons. Some consider an examination complete if the duplex of the nondominant arm is “normal.” Most often, the nondominant arm is used first; however, the referring physician or surgeon may want to use the patient’s dominant arm in unusual circumstances such as stroke affecting the dominant side. In general, if “right only” or “left only” is not specified, the vessels are evaluated bilaterally (this applies to the upper or lower extremities) to ensure that all possible critical information is obtained. Adequate communication with the referring physician is particularly important prior to revision of an existing dialysis access fistula or graft to make sure that questions about anatomy, outflow veins, potential substitute veins, or arterial inflow are answered.
TABLE 33.3 Predialysis Access Mapping
A standard duplex ultrasound system is required for this examination with high-resolution B-mode imaging, color Doppler, and spectral waveform analysis. A selection of transducers with a choice of operating frequencies and “footprints” is necessary for scanning of the central and peripheral extremity vessels. These include a midrange-frequency linear array transducer (e.g., L7-4) for general applications and a high-frequency transducer (e.g., L12-5, L10-5 intraoperative, L15-7 intraoperative) for assessing the superficial veins. A small curved array transducer (e.g., C8-5), such as one designed for scanning neonatal heads, is excellent when scanning around the clavicle.
The examination begins with the patient in the supine position for bilateral brachial artery pressures and with the head slightly turned away from the limb being examined for evaluation of the subclavian and axillary veins. For evaluation of the arm veins, the head of the bed may be elevated 45 degrees with the arm dependent. Warming and a tourniquet, as described later in this chapter, may promote distention of the superficial veins. Several examiner positions can be utilized to scan the arms. Whenever possible, the examiner is positioned closest to the limb being evaluated (e.g., scan the right arm from the patient’s right side). Reaching across the patient’s body with one arm and operating the controls on the ultrasound system with the other arm causes muscle strain for the sonographer and can lead to musculoskeletal injuries. Thus, for a bilateral examination, after scanning the first arm, the machine may be moved to the contralateral side. Alternatively, if the examiner prefers to scan with one hand but still avoid reaching across to the contralateral side, the patient may be turned 180 degrees.
Central Venous Mapping
The normal anatomy of the upper extremity central veins is illustrated in Figure 33.3. Patency of the central veins should be ensured as far as possible, particularly in patients who have had prior venous access through puncture of these veins. Patency is compromised in about 20% of patients who have had indwelling central catheters for dialysis or other purposes. For these reasons, the central veins should be scanned first when performing a predialysis access mapping examination. The two main forms of central venous obstruction are stenosis and thrombosis. Stenosis in the innominate or subclavian vein is particularly common in patients with prior central venous catheters for short-term dialysis. Doppler findings with subclavian vein stenosis include a focal increase in Doppler flow velocity with poststenotic turbulence centrally and a continuous flow pattern peripherally. The duplex evaluation for upper extremity deep vein thrombosis is discussed in Chapter 20. Doppler waveforms from the innominate (brachiocephalic), subclavian, and axillary veins are all assessed for patency, normal flow pattern, and symmetry with the contralateral side.
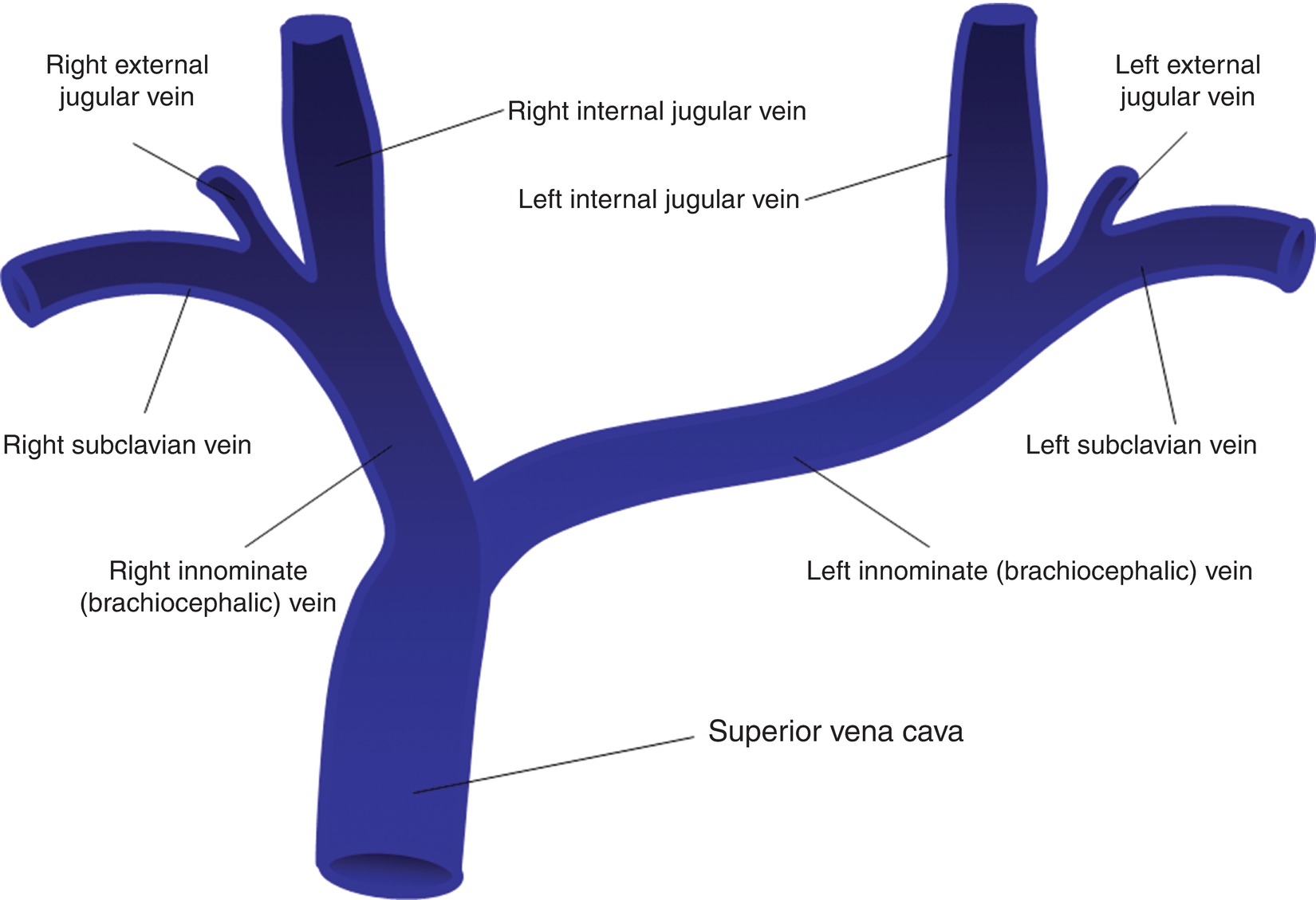
FIGURE 33.3 Anatomy of the upper extremity central veins.
The supraclavicular subclavian vein is a common location for venous stenosis where the subclavian vein curves to join the internal jugular vein. This segment often contains a valve that can become stenotic due to fibrosis of the leaflets. The infraclavicular subclavian vein is more easily imaged but is less likely to be stenotic. Doppler waveform analysis of flow in the infraclavicular subclavian vein can provide clues to the presence of a more proximal obstruction.
The axillary vein is a less common location for obstruction but may be a site of numerous collateral flow channels when a more central stenosis or occlusion exists. Subclavian vein obstruction may cause reversed flow in the axillary vein, which drains into chest wall collaterals. These prominent subcutaneous chest wall veins may be visible.
Superficial Venous Mapping
The entire cephalic vein (from the wrist to its confluence with the subclavian vein) should be scanned noting any branching, wall thickening, or thrombosis (Fig. 33.4). The diameter of the cephalic vein is measured along its entire course. A tourniquet can also be useful. Some examiners advocate use of two tourniquets, one above the elbow to occlude the deep veins and one below to occlude more superficial veins. The examination may begin without the use of a tourniquet. A diameter of 3 mm or greater is generally adequate. A tourniquet should be used if vein diameter is less than 3 mm. Diameter should be recorded with a note regarding use or nonuse of a tourniquet. Vein measurements can be obtained using either a long-axis or a transverse image, with minimal pressure on the skin to avoid compressing the vein. The long-axis view has been recommended to avoid inadvertent use of an oblique transverse image, which can cause overestimation of the diameter. If the cephalic vein is inadequate, a survey should be done for other veins in the distal half of the forearm. If other forearm veins are 3 mm or larger, they should be mapped and marked from the wrist to the antecubital fossa.
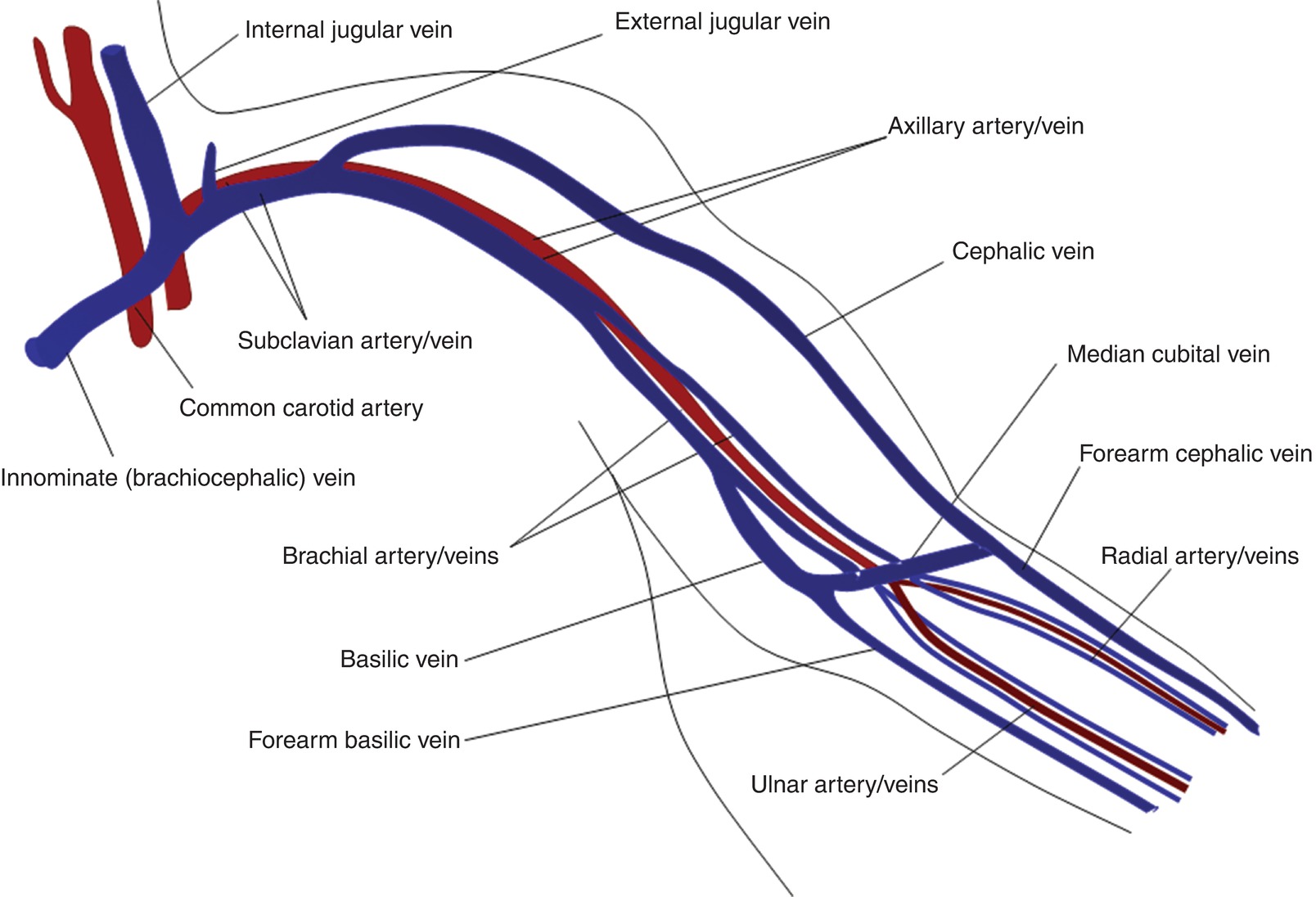
FIGURE 33.4 Anatomy of the upper extremity arteries and veins.
The basilic vein is examined from the wrist to the confluence with the brachial vein, noting the confluence location, branching, wall thickening or thrombosis, and vein diameter. Because the brachial vein is sometimes used for a transposition fistula, the diameter of this vessel should also be obtained. The anatomy of the basilic vein is quite variable; it may confluence with the brachial vein at the proximal or mid upper arm or with the axillary vein more centrally.
The median cubital is a short superficial vein that passes across the anterior aspect of the elbow between the cephalic and the basilic veins. The anatomy of the median cubital vein is extremely variable. Whenever it is associated with a patent basilic or cephalic vein, the diameter and patency of the median cubital vein should be documented.
Arterial Mapping
Bilateral brachial systolic blood pressures are obtained with the patient supine to assess for occlusive disease in the innominate, subclavian, and axillary arteries. Doppler velocity waveforms are also obtained from the brachial arteries in both arms. However, blood pressures generally should not be taken in arms with a patent fistula or graft, to avoid inadvertent thrombosis of the access. The subclavian and axillary arteries are scanned, with particular attention to these segments if the brachial systolic blood pressures are unequal. Normal velocity waveforms in the upper extremity arteries are triphasic with no significant focal velocity increases. Upper extremity arterial duplex scanning is discussed in Chapter 14. The brachial, radial, and ulnar arteries are scanned throughout their entire course, noting any atherosclerosis, tortuosity, medial calcification, or anatomic variants such as a high bifurcation of the brachial artery into the radial and ulnar branches in the proximal arm.
Palmar Arch (Allen’s Test)
If the forearm arteries and veins appear adequate for creation of a forearm fistula or graft, the palmar arch is evaluated to determine whether the blood supply to the hand is dependent on either the radial or the ulnar artery alone. The ulnar artery is often the dominant of the two forearm arteries and, therefore, is usually preserved for arterial supply to the hand. The radial artery is often nondominant and can be utilized for arterial inflow to the access site with little risk of hand ischemia. Patency of the palmar arch, which connects the radial and ulnar artery circulations, is evaluated with Allen’s test. In the classic, less reliable form, this test uses simple observation of the return of pink color to the palm after clenching the fist with either the radial or the ulnar artery manually compressed. Slow return of color with one or the other artery manually occluded suggests that the hand is reliant on the occluded artery for its primary blood supply. A more quantitative version of Allen’s test can be performed using photoplethysmography (PPG), as outlined in Table 33.4. Duplex scanning of the palmar arch can also be used for a direct evaluation of flow from the radial and ulnar arteries into the palm, using manual occlusion of these arteries at the wrist. These variations of Allen’s test are described in more detail in Chapter 34.
TABLE 33.4 Photoplethysmography Allen’s Test for Completeness of the Palmar Arch
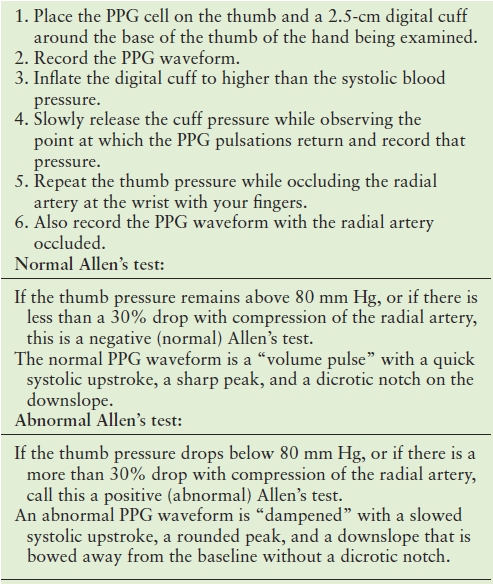
PPG, photoplethysmography.
Lower Extremity Mapping
Lower extremity sites may be considered for dialysis if there is no upper extremity alternative. The first step in the lower extremity evaluation is obtaining the ankle-brachial index bilaterally, being careful to avoid applying pressure cuffs over an existing patent graft or fistula. Generally, a dialysis access graft or fistula should not be placed in an extremity with an abnormally low ankle-brachial index or ankle pressure. The common femoral and proximal superficial femoral arteries in the thigh should be scanned to evaluate for stenosis and extent of calcification. Focal velocity increases of greater than 1.5-fold are suggestive of a significant stenosis. Duplex evaluation of the lower extremity arteries is discussed in Chapter 12. If vein mapping of the lower extremity is requested, the approach is similar to mapping these veins for use in arterial bypass surgery (see Chapter 28). Evaluation of the saphenofemoral junction and great saphenous vein is performed to the level of the knee for thrombosis, wall thickening, chronic webbing, varicosity, branching, and diameter. The common femoral, deep femoral, and femoral veins are evaluated for patency and velocity waveform patterns, as discussed in Chapter 19.
Pitfalls of Predialysis Access Mapping
A cold environment (cold room or cold gel) may cause the superficial veins to vasoconstrict and appear smaller on B-mode image than in their normal state. Furthermore, superficial veins are easily compressed, which makes accurate diameter measurements a delicate procedure. Optimal results are obtained if the patient is in a warm environment for at least 30 minutes prior to scanning. Directly warming the extremity with a heating pad and exercise of the extremity may also be helpful, as is gentle repeated slapping over the vein, as is done prior to phlebotomy. In some cases, it may be necessary to bring the patient back on another day for a repeat examination.
Patients with ESRD commonly present to the vascular laboratory with a history of multiple prior dialysis access procedures and revisions. There may be patent or occluded access sites, which complicate ultrasound evaluation and mapping. In these cases, obtaining as much detailed surgical history as possible is very helpful. Operative notes or diagrams are particularly helpful in this setting.
INTRAOPERATIVE EVALUATION
There are several ways for the surgeon to assess the adequacy of a new access site in the operating room. Simple palpation can often determine whether the access is functioning well. There should be a strong palpable thrill along the course of a fistula and in the draining vein of a graft. Absence of a thrill indicates inadequate flow, often due to impaired arterial inflow. Problems with outflow result in a strong pulse in the fistula or graft due to increased pressure resulting from restricted outflow. A normal access will have an obvious thrill that disappears and is replaced by a strong pulse when the outflow is manually occluded. If a sterile flow meter is available, this can be used to ensure that initial flow through the new fistula is at least 200 mL/min. Sterile continuous-wave Doppler examination should indicate low-resistance flow (high velocities with significant forward flow during diastole) in the fistula and in the artery just proximal to it. The artery distal to the anastomosis may also have this velocity pattern if it carries retrograde flow into the fistula from collateral vessels (such as flow from the ulnar artery through the palmar arch to the radial artery).
The surgeon should make sure that the circulation to the hand is adequate by listening to continuous-wave Doppler arterial signals at the wrist and palm as well as at the base of the fingers. Unfortunately, it is difficult to quantitate this examination to ensure that flow to the hand is sufficient to prevent a clinically significant steal. Even with adequate distal perfusion, it is common for these signals to be slightly diminished by the fistula and augmented when it is occluded. Digit pressures of at least 60 mm Hg are reassuring but are difficult to obtain at the time of surgery. Intraoperative angiography can also be helpful when there is doubt about fistula function. Central vein stenosis or occlusion is best studied with computerized tomography or magnetic resonance angiography.
Duplex scanning also can be a useful tool in the operating room. When a new arteriovenous fistula is created, the vein should have a diameter of at least 2.5 to 3.0 mm and should have flows of 200 mL/min or more. The vein should also be within 6 mm of the skin surface, although the surgeon may choose to superficialize the vein at a separate procedure after it has matured to a larger, thicker, and sometimes slightly elongated vessel that is more easily manipulated. The intraoperative duplex assessment is described in Chapter 30.
ACCESS MATURATION
Adequacy of access for hemodialysis can be judged by the rule of sixes: 6 weeks after placement, there should be a length of at least 6 cm for cannulation, the access should be no more than 6 mm below the skin surface for ease of puncture, and blood flow should be at least 600 mL/min for adequate filtration. These parameters can be assessed with duplex scanning, which can evaluate problems that may be interfering with vein maturation such as the presence of large side branches that divert flow, narrowing of the outflow vein or more central venous outflow obstruction, and stenosis of the arterial anastomosis. It is helpful to scan new fistulas 4 to 6 weeks after surgery to ensure that they are maturing or determine the cause of nonmaturation.8 Aggressive intervention soon after access creation may speed maturation and even salvage some fistulas that may not otherwise have matured. Possible interventions include ligation of venous side branches, repair of venous or arterial stenoses, vein angioplasty (balloon-assisted maturation), and vein superficialization.9
Volume Flow Measurements for Maturation
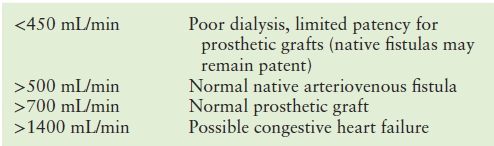
Access monitoring has typically relied on anatomic imaging (i.e., angiography) to evaluate access function and maturity. However, current recommendations support the addition of physiologic testing using Doppler measurements to identify low volume flow, a hemodynamic parameter predictive of impending thrombosis or difficult hemodialysis. Volume flow rates are typically in the range of 800 to 1200 mL/min in functioning fistulas and grafts. Flow rates of less than 500 mL/min are generally considered indicative of possible impending failure. Native vein fistulas tend to require less flow to remain patient than do prosthetic grafts. Table 33.5 lists some threshold volume flow criteria for dialysis access sites. Volume flow is more predictive of access failure than increased velocity, whereas velocity is better for detecting stenosis. Volume flow calculations also can help determine failure to mature (decreased volume flow) or cardiac volume overload (increased volume flow).
TABLE 33.5 Dialysis Access Volume Flow Criteria
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


