Early and accurate triage of patients with possible ischemic chest pain remains challenging in the emergency department because current risk stratification techniques have significant cost and limited availability. The aim of this study was to determine the diagnostic value of the coronary artery calcium score (CACS) for the detection of obstructive coronary artery disease (CAD) in low- to intermediate-risk patients evaluated in the emergency department for suspected acute coronary syndromes. A total of 225 patients presenting to the emergency department with acute chest pain and Thrombolysis In Myocardial Infarction (TIMI) scores <4 who underwent non-contrast- and contrast-enhanced coronary computed tomographic angiography were included. CACS was calculated from the noncontrast scan using the Agatston method. The prevalence of obstructive CAD (defined from the contrast scan as ≥50% maximal reduction in luminal diameter in any segment) was 9% and increased significantly with higher scores (p <0.01 for trend). CACS of 0 were observed in 133 patients (59%), of whom only 2 (1.5%) had obstructive CAD. The diagnostic accuracy of CACS to detect obstructive CAD was good, with an area under the receiver-operating characteristic curve of 0.88 and a negative predictive value of 99% for a CACS of 0. In a multivariate model, CACS was independently associated with obstructive CAD (odds ratio 7.01, p = 0.02) and provided additional diagnostic value over traditional CAD risk factors. In conclusion, CACS appears to be an effective initial tool for risk stratification of low- to intermediate-risk patients with possible acute coronary syndromes, on the basis of its high negative predictive value and additive diagnostic value.
The coronary artery calcium score (CACS) has been proposed as an alternative approach for stratifying cardiovascular risk. In contrast to contrast-enhanced coronary computed tomographic angiography (CCTA), coronary artery calcium scoring has low radiation exposure, produces highly reproducible results, and requires no medication or contrast use and minimal patient cooperation. It has been shown that the presence of calcium is a quantifiable marker of atherosclerotic disease, with good correlations with histologic, intracoronary ultrasound, and angiographic measures of plaque burden. Moreover, CACS is an established predictor of cardiovascular events. However, the role of CACS as part of the initial diagnostic evaluation of patients with suspected acute coronary syndromes (ACS) remains controversial. The primary goal of this study was to determine the diagnostic utility of CACS in low- to intermediate-risk patients presenting to the emergency department (ED) with chest pain or angina-like symptoms, nondiagnostic electrocardiographic findings, and negative cardiac biomarkers.
Methods
From March 2007 to January 2009, all consecutive patients who were evaluated in the ED for suspected ACS with nondiagnostic electrocardiographic findings and negative initial cardiac troponin and subsequently underwent CCTA and coronary artery calcium scoring were retrospectively studied. Exclusion criteria included known significant coronary artery disease (CAD), defined as coronary artery stenosis ≥50% and/or previous coronary revascularization. Troponin I was considered negative when <0.5 ng/dl (the upper limit of normal at our institution), and electrocardiographic findings were considered nondiagnostic in the absence of ST-segment elevation or depression ≥1 mm or T wave >4 mm in ≥2 contiguous leads. For the purpose of analysis, a modified Thrombolysis In Myocardial Infarction (TIMI) risk score was retrospectively calculated. Because patients with positive troponin, diagnostic electrocardiographic findings for ischemia, and/or known significant CAD were excluded from the analysis, and the number of angina episodes was not consistently reported, a maximum score of 3 was possible on this modified scale. Pretest probability of CAD on the basis of American College of Cardiology and American Heart Association guidelines was also retrospectively calculated for further analysis. The CAD risk factors were defined as follows: (1) diabetes mellitus as a history of ≥2 determinations of fasting blood glucose ≥126 mg/dl or taking insulin or oral antidiabetic drugs; (2) hypertension as a history of ≥2 determinations of systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg or taking antihypertensive drugs; (3) smoking history, defined as current or previous tobacco use of 5 pack-years; (4) hypercholesterolemia as a history of total cholesterol ≥200 mg/dl and/or low-density lipoprotein ≥130 mg/dl or taking statins; and (5) positive family history when first-degree relatives had myocardial infarctions, coronary revascularization, or sudden death before the age of 55 years (men) and 65 years (women). The study was approved by the institutional review board of the Mount Sinai School of Medicine.
CCTA was performed using a 64-slice scanner (LightSpeed VCT, XT; GE Healthcare, Milwaukee, Wisconsin) with either retrospective or prospective electrocardiographic gating. All patients received sublingual nitroglycerin (0.4 mg) and β blockers (intravenous metoprolol 5 to 30 mg) if their heart rates were >60 beats/min, unless contraindications were present. After standard scouts in the supine position, a noncontrast scan was performed to assess coronary artery calcification. This consisted of a single inspiratory breath-hold craniocaudal acquisition covering from the carina to the inferior heart border. Prospectively triggered imaging was used, with a tube voltage and an effective current of 120 kVp and 200 mA, respectively. Subsequently, contrast-enhanced angiography was performed in which the contrast circulation time was determined with a timed bolus of 20 ml of contrast agent (Isovue 370; Schering AG, Berlin, Germany) or with the bolus-tracking technique with a threshold of 100 Hounsfield units in a region of interest in the ascending aorta. A 70- to 100-ml contrast bolus followed by 50 ml of saline was injected through a peripheral vein at 4 to 5 ml/s. For scanning, a detector collimation of 64 × 0.625 mm was used, with a gantry rotation of 330 ms, pitch of 0.16 to 0.25, tube voltage of 120 kVp, and tube current of 400 to 700 mA. Tube current modulation was used if applicable in the retrospective protocols.
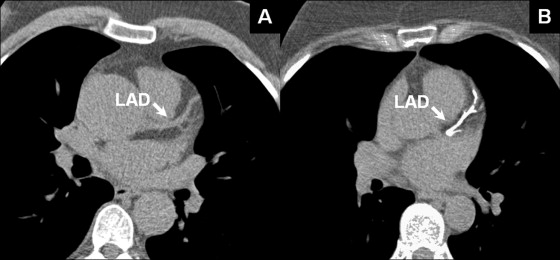
Axial images were reconstructed with an image matrix of 512 × 512 pixels and slice thickness of 0.625 mm. A half-scan algorithm with a temporal resolution of approximately 165 ms was performed for retrospectively gated acquisitions, whereas a multisegment algorithm was used for heart rates >70 beats/min. Images were preferentially reconstructed in the mid-diastolic phase (65% to 85% of the cardiac cycle) for motion-free images of the coronary arteries. The CACS was calculated using the Agatston method, which is determined by calcified area and calcium score density. Semiautomatic software (TeraRecon, San Mateo, California) displayed colored spots for calcium, defined as hyperattenuating lesions with ≥130 Hounsfield units with an area ≥1.0 mm 2 , which were manually identified by the operator and automatically summed to obtain total calcium score ( Figure 1 ). Patients were stratified according to CACS into 3 groups: normal (CACS = 0), low (CACS = 1 to 100), and high (CACS >100). The results of CCTA were interpreted on a dedicated workstation (Aquarius; TeraRecon) by 2 experienced readers. Coronary assessment was performed on original axial sources images, thin-slice maximum-intensity projections, or multiplanar reformatted reconstructions. Significant or obstructive CAD was defined as ≥50% luminal diameter narrowing and considered moderate or severe when causing 50% to 70% or >70% stenosis, respectively. Plaques causing <50% stenosis were considered nonsignificant disease. The presence of calcification per artery was also evaluated, as well as the composition of coronary plaques responsible for significant stenosis. Briefly, calcified plaque was defined as any lesion with attenuation >130 Hounsfield units and noncalcified plaque with attenuation below the contrast-enhanced coronary lumen and Hounsfield units >0. Nondiagnostic results of CCTA were considered when any proximal or mid coronary segment was not evaluable because of motion artifacts, calcification, or low contrast-to-noise ratio.
Statistical analysis was performed with SPSS version 15.0 (SPSS, Inc., Chicago, Illinois). Continuous variables are expressed as mean ± SD or as median (range) depending on their distribution. Categorical variables are expressed as total number (percentage). The accuracy of CACS to detect significant CAD was assessed by the area under the receiver-operating characteristic curve. Sensitivity, specificity, and predictive values were calculated for a CACS of 0. Analysis of variance for trend and the Mantel-Haenszel test were performed to evaluate differential distribution of age, CAD risk factors, and significant CAD according to CACS severity. Multivariate analysis was used to identify independent predictors of significant CAD. Two logistic regression models were constructed; the first included age, gender, CAD risk factors, and chest pain characteristics, and the second model additionally included CACS. To evaluate the goodness of fit of the logistic regression models, the coefficient of determination (Nagelkerke’s R 2 ) was calculated. A p value <0.05 was considered statistically significant.
Results
From March 2007 to January 2009, 247 consecutive patients presenting to the ED with suspected ACS underwent CCTA. Of them, 22 patients did not have calcium score scans performed, because of histories of coronary revascularization or young age (<30 years). Therefore, the final cohort consisted of 225 patients. Study population characteristics are listed in Table 1 . The prevalence of significant CAD was 9% and increased along with higher pretest probability and higher TIMI risk score ( Figure 2 ). All patients with severe coronary stenosis on CCTA (n = 7) were referred for invasive coronary angiography and subsequent coronary revascularization. Patients with moderate stenosis were referred for invasive coronary angiography (n = 6), stress testing (n = 2), or clinical follow-up (n = 5), as determined by the attending physician in the ED in conjunction with the consulting cardiologist. Of a total of 13 patients referred for invasive coronary angiography, 2 had <50% coronary stenosis, and 11 had ≥1-vessel disease with >50% coronary stenosis. In 6 patients (3%), CCTA was considered a nondiagnostic test, and patients underwent nuclear stress testing or coronary angiography on the basis of the recommendation of the cardiology consult service. In these patients, the presence of significance was established on the basis of the subsequent test results. Mean radiation exposure for CACS scans was 0.8 ± 0.3 mSv and for CCTA was 8.5 ± 3.2 mSv.
| Variable | Value |
|---|---|
| Age (years) | 53 (32–89) |
| Men | 102 (45%) |
| Race | |
| Hispanic | 96 (43%) |
| African American | 64 (28%) |
| Caucasian | 49 (21%) |
| Asian American | 16 (7%) |
| Cardiac risk factors ⁎ | |
| Hypertension | 104 (46%) |
| Hypercholesterolemia | 72 (32%) |
| Current or former smoker | 69 (30%) |
| Diabetes mellitus | 44 (20%) |
| Medical treatment | |
| Aspirin | 41 (18%) |
| Statins | 34 (15%) |
| Angiotensin-converting enzyme inhibitors | 23 (10%) |
| Calcium channel antagonists | 18 (8%) |
| Diuretics | 14 (6%) |
| β blockers | 10 (4%) |
| Symptoms | |
| Atypical chest pain | 190 (84%) |
| Typical chest pain | 35 (16%) |
| Acute dyspnea | 39 (17%) |
| Chest discomfort and palpitations | 10 (4%) |
| TIMI risk score | |
| 0 | 134 (60%) |
| 1 | 69 (31%) |
| 2 | 18 (8%) |
| 3 | 4 (2%) |
| Pretest probability of CAD | |
| Low | 33 (15%) |
| Intermediate | 172 (76%) |
| High | 20 (9%) |
| Creatinine (mg/dl) | 0.93 ± 0.21 |
| CACS | 0 (0–3,454) |
| Multidetector computed tomography | |
| Heart rate (beats/min) | 67.2 ± 12.1 |
| Systolic blood pressure (mm Hg) | 135.1 ± 17.5 |
| Diastolic blood pressure (mm Hg) | 77.1 ± 13.2 |
| Contrast agent (ml) | 92.6 ± 23.8 |
| Retrospective | 197 (88%) |
| Metoprolol use | 179 (79%) |
| Nitroglycerin use | 213 (95%) |
⁎ Cardiac risk factors are defined in the “Methods” section.
The percentage of patients with CACS >0 was significantly higher in the presence of intermediate or high pretest probability compared to low pretest probability and gradually augmented with the modified TIMI risk score ( Figure 3 ). Coronary artery calcification was found in the left anterior descending coronary artery in 85 patients (34%), the right coronary artery in 38 (17%), the left circumflex coronary artery in 36 (16%), and the left main coronary artery in 16 (7%). In the 133 patients (59%) with CACS of 0, 2 (1.5%) had significant CAD, 7 (5%) had nonsignificant CAD, and 124 (93%) had no evidence of CAD. One of the 2 patients with CACS of 0 and significant CAD had intermediate pretest probability and a TIMI score of 1 (a 48-year-old Hispanic man with multiple cardiac risk factors and atypical chest pain), and the other patient had high pretest probability and a TIMI score of 2 (a 75-year-old black woman without cardiac risk factors and typical chest pain). In these cases, the stenosis was graded as moderate in severity, and subsequently, the patients underwent stress testing, which did not demonstrate inducible ischemia. Furthermore, no cardiovascular events were registered within 12 months after discharge.
The distribution of baseline characteristics, cardiac risk factors, and results of CCTA according to the severity of CACS is listed in Table 2 . Age, male gender, hypercholesterolemia, diabetes, and previous aspirin use as well as the severity of CAD increased gradually among groups. Coronary plaques responsible for significant stenosis were predominately totally or partially calcified in composition. Of 34 significant stenoses found in our study population, 27 (80%) contained calcium, whereas 7 (20%) lesions were caused by noncalcified plaques. Noncalcified plaques causing significant stenosis occurred in patients with coronary calcification in other segments, and therefore, CACS was positive, except in 2 cases. This finding suggests that is very rare to find obstructive noncalcified plaques in the setting of a CACS of 0.
| CACS | ||||
|---|---|---|---|---|
| Variable | 0 (n = 133) | 1–100 (n = 61) | >100 (n = 31) | p Value for Trend |
| Age (years) | 51 ± 9 | 54 ± 9 | 66 ± 10 | <0.01 |
| Men | 49 (37%) | 35 (57%) | 18 (58%) | 0.01 |
| Hypertension | 57 (43%) | 29 (48%) | 18 (58%) | 0.13 |
| Hypercholesterolemia | 24 (18%) | 25 (41%) | 23 (74%) | <0.01 |
| Smokers | 42 (32%) | 17 (28%) | 9 (29%) | 0.66 |
| Diabetes mellitus | 13 (10%) | 21 (34%) | 10 (32%) | <0.01 |
| Previous use of aspirin | 14 (11%) | 17 (28%) | 10 (32%) | <0.01 |
| Typical angina pectoris | 22 (17%) | 10 (17%) | 3 (12%) | 0.43 |
| Significant CAD by CCTA | 2 (1.5%) | 6 (10%) | 12 (39%) | <0.01 |
| Moderate | 2 (100%) | 5 (83%) | 6 (46%) | <0.01 |
| Severe | 0 (0%) | 1 (17%) | 6 (54%) | <0.01 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


