Renal insufficiency and anemia are increasingly recognized as predictors of adverse events in heart failure. The impact of blood transfusion on mortality in patients with heart failure has not been previously characterized. We examined temporal changes in admissions and in-hospital mortality using public discharge data from California (2000 to 2006) and then evaluated the impact of renal insufficiency, anemia, and transfusion on in-hospital mortality in univariate and multivariate analyses. In total 596,456 unique patient admissions for heart failure were recorded. Renal insufficiency and anemia were common co-morbidities (27.4% and 27.1%, respectively) and 6.2% of patients received a transfusion of red blood cells. Renal insufficiency and anemia were associated with increased mortality (unadjusted odds ratio [OR] 2.45, 95% confidence interval [CI] 2.39 to 2.52, and 1.27, 95% CI 1.24 to 1.30, respectively). After adjustment, renal insufficiency (OR 2.54, 95% CI 2.46 to 2.62) and anemia (OR 1.12 95% CI 1.07 to 1.17) remained significant; however, transfusion emerged as the strongest single predictor (OR 3.81, 95% CI 3.51 to 4.13) of mortality. In conclusion, these data suggest that anemia and renal insufficiency are independently associated with mortality in an unselected heart failure population. This is the first study to demonstrate that transfusion magnifies this effect and is associated with a particularly poor prognosis.
Heart failure is the leading cause of hospitalization and rehospitalization in elderly patients in the United States. Elderly patients with heart failure frequently have additional co-morbid conditions that complicate their inpatient care and worsen overall prognosis. Specifically, anemia and chronic renal insufficiency are common co-morbidities in the aging population and are associated with increased mortality in the setting of heart failure. The simultaneous presence of anemia and renal insufficiency in patients with heart failure is often referred to as the cardiorenal–anemia syndrome and has been shown to magnify long-term morbidity and mortality irrespective of patient age. The impact of red blood cell transfusion in patients with acute decompensated heart failure, however, has not been previously described, yet may be an important mediator of adverse events. The prognostic importance of these cofactors varies depending on the size of the study population and data source used. Because current heart failure population studies are derived from voluntary quality improvement initiatives, industry-funded registries, or demographically limited cohorts such as Medicare, the generalizability of findings to the diversity of patients with heart failure in the United States is uncertain. The present study, therefore, evaluated discharge data from a large, unselected database in California. We sought to quantify the effects of renal insufficiency, anemia, and the receipt of blood transfusion on in-hospital outcomes.
Methods
The California Office of Statewide Health Planning and Development collect data on all hospitalizations in the state of California as mandated by state law. We selected this state because it is currently the largest single United States population base with standardized, deidentified, and publicly available patient discharge data (PDD). Diagnoses and procedure codes for all admissions are classified using the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM). After obtaining an exemption from Colorado Multiple Institutional Review Board, all PDD from California from January 1, 2000 to December 31, 2006 were obtained and admissions with the principal diagnosis of heart failure were extracted for analysis. Admissions where heart failure was not listed as the principal diagnosis were excluded as were hospitalizations where age was <18 years. These data were linked with census data from California to calculate population-adjusted hospitalization and mortality rates.
De-identified PDD were imported into a MySQL server (MySQL, Inc., Sun Microsystems, Cupertino, California), which was used for data collation. Patient age, gender, ethnicity, payer status, admission type, length of stay, and in-hospital mortality were quantified directly from the database. Presence of co-morbid conditions for each admission was determined using the ICD-9-CM codes in secondary diagnosis fields. Patients who underwent hemodialysis or received transfusions of packed red blood cells were identified by the presence of corresponding ICD-9-CM procedure codes in any of the procedure fields associated with each hospitalization. California population estimates from 2000 to 2006 were acquired from the United States Census Bureau and population-adjusted admission and mortality rates were calculated for each year and summarized across years by calculating an annual percent change (APC). The APC and 95% confidence intervals (CIs) were determined from the slope and standard error estimates from the regression line calculated on the log scale. Baseline clinical and demographic data were summarized using the number and percent per group. Overall mortality rates were presented for various clinical co-morbidities in addition to unadjusted odds ratios (ORs) and 95% CIs.
A multiple logistic regression model was fit to estimate the odds for predictors of mortality. Predictors for length of stay (LOS) were estimated using a Cox proportional hazards model censoring for deaths before discharge. Covariates used in the 2 models included demographics (age, gender, and ethnicity), admission type, the most common co-morbidities (hypertension, ischemic heart disease, diabetes, atrial fibrillation, renal insufficiency, anemia, chronic obstructive pulmonary disease, and dyslipidemia), and 2 prespecified procedures (transfusion and hemodialysis). All covariates remained in the model to assess their strength of association with the outcome in the presence of other factors. Interactions of anemia with transfusion, anemia with renal insufficiency, hemodialysis with renal insufficiency, and transfusion with renal insufficiency were included in the models and removed if their maximum likelihood estimate was not significant at the 0.05 alpha level. Because of the large number of observations in this study, overpowering resulted in most covariates showing statistical significance in the models. Therefore, to identify covariates that had a consistent reportable relation with the outcome, the models were run on smaller random samples of the data. Statistical analysis was performed using SAS 9.2 (SAS Institute, Cary, North Carolina).
Results
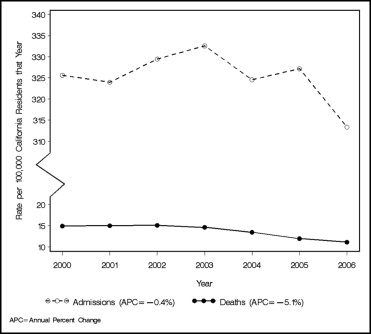
In total 596,456 of 27,522,042 (2.2%) hospital admissions in California met criteria for inclusion in the analysis from 2000 to 2006. Population-adjusted rates of hospitalization and in-hospital mortality are presented in Figure 1 . Over the study period population-adjusted rate of heart failure admissions varied from 332 to 313 per 100,000 but did not exhibit a significant increase or decrease over the study period (APC −0.4%, 95% CI −1.07 to 0.28). However, population-adjusted mortality rates decreased moderately from 15 to 11 per 100,000, resulting in an APC equal to −5.1% (95% CI −3.02 to −7.04).
Baseline demographics and clinical characteristics are listed in Table 1 . A majority (72.6%) of the population was >65 years old and correspondingly nearly 70% of the population was a recipient of Medicare. Hypertension and coronary heart disease were the 2 most common co-morbidities. In total 27.4% of patients had renal insufficiency and 27.1% had anemia. Overall, 6.2% of the population received a blood transfusion.
| Category | |
|---|---|
| Age (years) | |
| 18–34 | 8,640 (1.5%) |
| 35–64 | 155,066 (26.0%) |
| ≥65 | 432,750 (72.6%) |
| Men | 261,019 (43.8%) |
| Women | 280,664 (47.1%) |
| Unknown/masked/missing | 54,773 (9.2%) |
| Ethnicity/race | |
| White | 334,625 (56.1%) |
| Hispanic | 73,556 (12.3%) |
| Black | 58,027 (9.7%) |
| Asian/Pacific islander | 25,424 (4.3%) |
| Native American/Eskimo/Aleut | 486 (0.1%) |
| Other | 7,039 (1.2%) |
| Unknown | 97,299 (16.3%) |
| Insurance | |
| Medicare | 416,373 (69.8%) |
| Medicaid | 76,333 (12.8%) |
| Private coverage | 75,249 (12.6%) |
| Self-pay | 12,513 (2.1%) |
| Other | |
| Admission | |
| Scheduled | 41,426 (7.0%) |
| Unscheduled | 554,265 (92.9%) |
| Other | 765 (0.1%) |
| Co-morbidity | |
| Hypertension | 362,919 (60.9%) |
| Coronary heart disease | 296,177 (49.7%) |
| Diabetes mellitus | 242,956 (40.7%) |
| Atrial fibrillation | 182,361 (30.6%) |
| Renal insufficiency | 163,402 (27.4%) |
| Anemia | 161,468 (27.1%) |
| Chronic obstructive pulmonary disease | 152,340 (25.5%) |
| Dyslipidemia | 129,867 (21.8%) |
| Underwent hemodialysis | 40,098 (6.7%) |
| Received transfusion | 36,749 (6.2%) |
Effects of demographics and clinical characteristics on in-hospital mortality and LOS are presented in Table 2 . Overall, 4.23% of the population died, and median LOS was 4 days. Absolute mortality rates were higher than the overall population in subjects with renal insufficiency or who underwent hemodialysis or transfusion during their hospitalization. Median LOS was increased in subjects with renal insufficiency (5 days), anemia (5 days), and for those who received a transfusion (6 days). Patients who received a blood transfusion without concurrent anemia had the highest absolute mortality rate (17.46%) and longest median LOS (10 days).
| Feature (ICD-9-CM code) | Mortality (%) | Unadjusted OR (95% CI) | LOS (Days), Median (Q1–Q3) |
|---|---|---|---|
| All | 4.23% | — | 4 (2–6) |
| Men | 4.24% | — | 4 (2–6) |
| Women | 4.10% | 0.96 (0.94–0.99) | 4 (2–6) |
| White | 4.86% | — | 4 (2–6) |
| Hispanic | 3.07% | 0.62 (0.59–0.65) | 4 (2–6) |
| Black | 2.08% | 0.42 (0.39–0.44) | 3 (2–6) |
| Asian | 3.76% | 0.76 (0.0.72-0.82) | 4 (2–7) |
| Native-American | 1.85% | 0.37 (0.19–0.72) | 4 (2–6) |
| Other race | 3.58% | 0.73 (0.64–0.83) | 4 (2–6) |
| Scheduled admission | 5.60% | — | 4 (2–8) |
| Unscheduled admission | 4.12% | 0.73 (0.69–0.76) | 4 (2–6) |
| Hypertension | 3.41% | 0.61 (0.59–0.62) | 4 (2–6) |
| Coronary heart disease | 4.57% | 1.18 (1.15–1.21) | 4 (2–6) |
| Diabetes mellitus | 3.75% | 0.82 (0.80–0.84) | 4 (2–6) |
| Atrial fibrillation | 5.64% | 1.60 (1.56–1.64) | 4 (2–7) |
| Renal insufficiency | 7.25% | 2.45 (2.39–2.52) | 5 (3–8) |
| Anemia | 4.96% | 1.27 (1.24–1.30) | 5 (3–8) |
| Dyslipidemia | 2.67% | 0.56 (0.54–0.58) | 3 (2–6) |
| Hemodialysis | 7.43% | 1.93 (1.85–2.01) | 4 (2–8) |
| Transfusion | 8.37% | 2.22 (2.13–3.21) | 6 (4–11) |
| Chronic obstructive pulmonary disease | 5.35% | 1.36 (1.31–1.40) | 4 (2–7) |
| Neither anemia nor renal insufficiency | 2.95% | — | 3 (2–5) |
| Anemia and renal insufficiency | 6.82% | 2.40 (2.32–2.49) | 5 (3–9) |
| Renal insufficiency, no anemia | 7.56% | 2.69 (2.61–2.78) | 4 (2–7) |
| Anemia, no renal insufficiency | 3.58% | 1.22 (1.17–1.27) | 4 (3–7) |
| Neither anemia nor transfusion | 3.81% | — | 3 (2–6) |
| Anemia and transfusion | 7.09% | 1.93 (1.84–2.02) | 6 (4–10) |
| Transfusion, no anemia | 17.46% | 5.34 (4.94–5.78) | 10 (6–17.5) |
| Anemia, no transfusion | 4.43% | 1.17 (1.14–1.21) | 4 (3–7) |
Univariate predictors of in-hospital mortality and hospital LOS are listed in Table 2 . Renal insufficiency was the strongest univariate predictor of mortality followed by receipt of transfusion. Presence of anemia was a modest predictor of in-hospital mortality. Additional co-morbidities such as chronic obstructive pulmonary disease and atrial fibrillation were significantly associated with adverse outcomes, whereas dyslipidemia and hypertension were associated with lower mortality rates in the univariate model. Notably, receipt of transfusion without a documented anemia diagnosis was strongly associated with mortality (OR 5.34, 95% CI 4.94 to 5.78) and hospital LOS (10 days, 6 to 17.5).
ORs and 95% CIs from a multiple logistic regression mortality model are presented in Figure 2 . Advanced age (≥65 years) was a significant predictor of mortality, whereas dyslipidemia and hypertension were associated with lower odds of mortality as observed in the univariate model. However, atrial fibrillation and renal insufficiency persisted as adverse prognostic factors. Undergoing hemodialysis (OR 2.2, 95% CI 2.1 to 2.3) and transfusion (OR 3.8, 95% CI 3.5 to 4.1) were also associated with an increased in-hospital mortality rate. Anemia alone, however, was associated with only a small increased risk for in-hospital mortality (OR 1.1, 95% CI 1.1 to 1.2), although interactions of anemia with transfusion (OR 1.7, 95% CI 1.6 to 1.8) and with renal insufficiency (OR 2.2, 95% CI 2.1 to 2.3) magnified the odds in the 2 cases. Receipt of a blood transfusion during the index hospitalization remained the strongest single predictor (OR 3.81, 95% CI 3.51 to 4.13) of mortality.




