, James L. JanuzziJr.2 and James L. JanuzziJr.3
(1)
Harvard Medical School Advanced Heart Failure and Cardiac Transplantation, Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
(2)
Harvard Medical School, Boston, USA
(3)
Cardiac Intensive Care Unit, Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
Abstract
Heart failure (HF) is a complex disorder that consists of a clinical syndrome with symptoms associated with pulmonary or systemic congestion with or without poor cardiac output. Acute heart failure is defined as acute onset of signs and symptoms of HF requiring urgent or emergent intervention. Symptoms may be of new onset or recurrent. Acute HF can be associated with reduced LV systolic dysfunction (HFrEF or Systolic HF) or can occur in patients with preserved LV ejection fraction (LVEF) (HFpEF or diastolic HF); up to 50 % of patients hospitalized with acute HF have preserved LV systolic function. It is important to recognize that acute HF can present without signs and symptoms of congestion and patients may only have manifestations of low cardiac output and cardiogenic shock.
Abbreviations
ACC
American college of cardiology
ACE
Angiotensin converting enzyme
ACS
Acute coronary syndromes
ADHF
Acute decompensated heart failure
AHA
American heart association
AR
Aortic regurgitation
ARB
Angiotensin II receptor blocker
BNP
B-type natriuretic peptides
BUN
Blood urea nitrogen
Ca
Calcium
cAMP
Cyclic adenosine monophosphate
CBC
Complete blood count
Cr
Creatinine
CRT
Cardiac resynchronization therapy
CVA
Cerebrovascular accident
CXR
Chest X-ray
HF
Heart failure
HFpEF
Heart failure with preserved ejection fraction
HFrEF
Heart failure with reduced ejection fraction
HFSA
Heart Failure Society of America
ICD
Implantable cardioverter defibrillator
JVP
Jugular venous pressure
K
Potassium
LFT
Liver function tests
LV
Left ventricle
LVEF
Left ventricle ejection fraction
MCS
Mechanical circulatory support
Mg
Magnesium
Na
Sodium
NSAIDS
Nonsteroidal anti-inflammatory drugs
NT-proBNP
N-terminal proBNP
NYHA
New York Heart Association
PAD
Peripheral arterial disease
PCWP
Pulmonary capillary wedge pressure
PVC
Premature ventricular contractions
PVR
Pulmonary vascular resistance
RV
Right ventricular
SVR
Systemic vascular resistance
TIA
Transient ischemic attack
VAD
Ventricular Assist Devices
VT
Ventricular tachycardia
Introduction
Heart failure (HF) is a complex disorder that consists of a clinical syndrome with symptoms associated with pulmonary or systemic congestion with or without poor cardiac output. Acute heart failure is defined as acute onset of signs and symptoms of HF requiring urgent or emergent intervention. Symptoms may be of new onset or recurrent. Acute HF can be associated with reduced LV systolic dysfunction (HFrEF or Systolic HF) or can occur in patients with preserved LV ejection fraction (LVEF) (HFpEF or diastolic HF); up to 50 % of patients hospitalized with acute HF have preserved LV systolic function [1, 2]. It is important to recognize that acute HF can present without signs and symptoms of congestion and patients may only have manifestations of low cardiac output and cardiogenic shock.
Epidemiology [3]
670,000 people are diagnosed with HF annually in the US; more than 290,000 deaths are associated with HF.
HF is the most common reason for hospitalization in people over age 65.
Over one million hospitalizations occur annually due to acute HF
Pathophysiology
Variety of mechanisms, consisting of an underlying substrate, triggering mechanism and perpetuating factors [8]
A.
Substrate: myocardial structure and function
Normal myocardial substrate that has suffered an acute injury
Ischemia/infarction
Inflammation (myocarditis, autoimmune)
Could be completely reversible, partially reversible or irreversible
Abnormal underlying substrate
American College of Cardiology (ACC)/American Heart Association (AHA) Stage B with first symptomatic event
Those with chronic compensated HF who present with an acute decompensation
Most common presentation
B.
Triggering mechanisms
Acute coronary syndromes (ACS) /ischemia
Medication non-compliance, iatrogenic changes in medications, drug interactions.
Dietary non-compliance
Worsening renal dysfunction
Renal artery stenosis [9] “Pickering syndrome”
Arrhythmias (Atrial or ventricular)
Pulmonary emboli
Infection
Severe hypertension
Volume administration (e.g. intravenous fluids or blood transfusions)
Cardiotoxic agents
Antineoplastic agents
Anthracyclines
Trastuzumab
Cyclophosphamide
Imatinib
Mitoxantrone
Sunitinib
Cocaine
ETOH
Ephedra
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDS)
Corticosteroids
Negative inotropes (e.g. verapamil/diltiazem)
RV pacing [12]
Hyper/hypothyroidism
Inflammation
Sleep apnea
Classification
Two major classification systems have been described for patients with HF [13]
A.
New York Heart Association (NYHA) Functional Classification of Heart Failure Symptoms (Table 14-1)
Table 14-1
New York Heart Association (NYHA) functional classification of heart failure symptoms
Class I | No symptoms with ordinary activity |
Class II | Slight limitation of physical activity; comfortable at rest, but ordinary physical activity results in fatigue, dyspnea or angina |
Class III | Marked limitation of physical activity; comfortable at rest, but less than ordinary physical activity results in fatigue, dyspnea or angina |
Class IV | Unable to carry out any physical activity without symptoms. Symptoms may be present at rest |
B.
ACC/AHA Staging System for HF (Table 14-2)
Table 14-2
American College of Cardiology/American Heart Association staging system for HF
Stage A | High risk for developing HF | Hypertension |
CAD | ||
Diabetes Mellitus | ||
Family history of cardiomyopathy | ||
Stage B | Asymptomatic HF | Previous MI |
LV Systolic dysfunction | ||
Asymptomatic valvular disease | ||
Stage C | Symptomatic HF | Known structural heart disease |
Shortness of breath and fatigue | ||
Reduced exercise tolerance | ||
Stage D | Refractory end-stage HF | Marked symptoms at rest despite maximal medical therapy |
Initial Assessment
Presentation
Dyspnea on exertion
most sensitive symptom
Paroxysmal nocturnal dyspnea
most specific symptom [14]
Peripheral edema
less common (66 %)
Fatigue
Cough, particularly nocturnal
Chest discomfort
Physical Examination
A rapid initial assessment should be performed to identify (Table 14-3):
Table 14-3
Estimation of hemodynamic profile based on exam findings
Congestion | Low cardiac output |
|---|---|
S3 and/or S4 gallop | Narrow pulse pressure (Usually less than 25) |
Prominent P2 | Cool extremities |
Elevated JVP | Lethargy/ altered mentation |
JVD > 10 cm corresponds to PCWP > 22 mmHg with 80 % accuracy | |
Hepatojugular reflux | Hypotension |
Hepatomegaly | Sinus Tachycardia |
Edema | Pulsus alternans |
Pulsatile liver | |
Ascites | |
Rales or wheezes (cardiac asthma) |
Evidence of congestion
Evidence of low output/ cardiogenic shock
Presence of co-morbidities and precipitating factors
NOTE: Clinical evaluation is often inaccurate
Diagnostic Evaluation (Table 14-4)
Table 14-4
Possible etiologies of AHF
Cardiac causes | Progression of underlying cardiomyopathy |
New onset/acute cardiomyopathy | |
Postpartum | |
Myocarditis | |
Tako-tsubo syndrome | |
Ischemia | |
Arrhythmias | |
Pericardial | |
Constriction | |
Tamponade | |
Valvular dysfunction | |
Stenosis | |
Regurgitation | |
Pressure overload | Severe hypertension |
Volume overload | Renal dysfunction |
Sodium/ volume load | |
Medication non-compliance (diuretics) | |
High output | Thyroid disease |
Shunt | |
Intracardiac | |
Extracardiac (A-V fistula) | |
Anemia | |
Septicemia | |
Miscellaneous causes | Infection |
Pulmonary embolism | |
New medications/substances | |
NSAIDs | |
Corticosteroids | |
Cardiotoxic agents |
1.
Chest X-ray (CXR)
Initial radiographs may not show evidence of pulmonary congestion [15]
>25 % of patients with acute decompensated heart failure (ADHF) present without CXR findings [16]
CXR findings include:
Dilated upper lobe vessels
Interstitial edema
Enlarged pulmonary arteries
Pleural effusion
Alveolar edema
Prominent superior vena cava
Kerley B lines
2.
Electrocardiogram
Assess for
Acute myocardial ischemia/infarction
LV hypertrophy
Arrhythmias
Atrial fibrillation
present in 31 % of patients presenting with acute HF
Heart block
PVC’s
Pacemaker malfunction, particularly in those patients with cardiac resynchronization therapy (CRT) devices; assess for adequate biventricular pacing.
3.
Laboratory tests
Electrolytes, including sodium (Na), calcium (Ca), potassium (K) and magnesium (Mg)
Renal function (blood urea nitrogen (BUN), Creatinine (Cr)) [17]
Liver function tests (LFT’s)
Thyroid function tests
Natriuretic Peptides
Two forms have been studied:
B-type natriuretic peptides (BNP), N-terminal proBNP (NT-proBNP)
Can be used when the diagnosis of acute HF is uncertain, for prognostication or to guide therapy [18]
Levels may be elevated in states other than acute HF, including chronic, compensated HF, acute myocardial infarction, valvular heart disease, and arrhythmias, while non-cardiac causes may include advancing age and renal failure.
complete blood count (CBC)
4.
Echocardiography
Assess LV and RV Function
1.
Preserved or reduced
2.
Ventricular structure
3.
Size
4.
Wall thickness
Other structural abnormalities
5.
Valvular
6.
Pericardial
7.
Right ventricle
8.
Atrial size
Indications for Hospitalization
A.
Per Heart Failure Society of America (HFSA) guidelines [19], hospitalization is recommended for patients with ADHF who present with the following clinical circumstances:
Hypotension
Worsening renal function
Altered mentation
Rest dyspnea
Tachypnea
Hypoxia
Hemodynamically significant arrhythmias
New onset rapid atrial fibrillation
ACS
B.
Consideration of hospitalization should be made if:
Evidence of worsening pulmonary or systemic congestion (even in the absence of dyspnea or weight gain)
Marked electrolyte disturbances
Multiple implantable cardioverter defibrillator (ICD) firings
Co-morbid conditions
Pneumonia
Diabetic ketoacidosis
Pulmonary embolus
Transient ischemic attack (TIA)/cerebrovascular accident (CVA)
Initial Management of Acute HF Syndromes
Goals
Rapidly relieve symptoms of congestion
Identify reversible causes, particularly ischemia
Restore hemodynamics
Ensure adequate oxygenation
Prevent end organ damage
Identify patients with low output states
Management should be based on hemodynamic profile
Rapid assessment and initiation of therapy can be made using the following 2 × 2 diagram demonstrating the various hemodynamic profiles of patients presenting with acute HF (Fig. 14-1) [20]
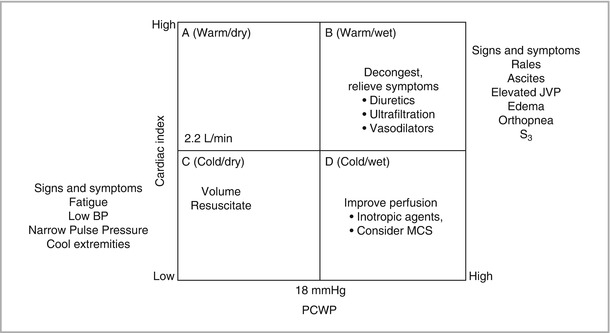
Figure 14-1
2 × 2 HF hemodynamic profiles. The above diagram demonstrates the hemodynamic profiles, signs and symptoms and treatment approach of patient’s presenting with heart failure. Quadrant A represents the patient who is not congested and has adequate perfusion. Quadrant B represents the patient who is congested but has adequate perfusion. Quadrant C represents the patient who is congested and has poor perfusion. Quadrant D represents the patient who has a normal to low volume status and poor perfusion. Treatment approaches overlap in the low output profiles, as those patients who are congested and also poorly perfused may need a separate treatment approaches to both conditions
After Admission
Practice guidelines recommend that the following parameters be monitored in patients hospitalized for acute HF [19]:
Get Clinical Tree app for offline access
Daily weight
Daily measurement of fluid intake and output
Vital signs (more than once daily, as indicated)
Physical exams signs (at least daily)
Increased jugular venous pressure (JVP)
Hepatojugular reflux
Rales
Edema
Hepatomegaly
Liver tenderness
Labs (at least daily)
Electrolytes
Renal function
Symptoms (at least daily)
Fatigue
Dyspnea
Orthopnea
Paroxysmal nocturnal dyspnea or cough
Hemodynamic monitoring
Studies, such as the ESCAPE study, assessing the use of routine invasive monitoring such as pulmonary artery catheter have been essentially neutral [21]
The routine use of invasive hemodynamic monitoring is not recommended, but should be considered under the following circumstances:
In those patients refractory to initial therapy< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


