Despite its proven efficacy, low cost, and wide availability, aspirin remains underused. We examined current aspirin use and determined factors that influence its use among outpatients in the United States (US). The REduction of Atherothrombosis for Continued Health (REACH) Registry is an international, prospective, longitudinal study of >68,000 outpatients with established atherothrombosis or ≥3 atherothrombotic risk factors. The rates of aspirin use were compared in various patient subgroups. Multivariate logistic regression models were constructed to determine the factors influencing the baseline use of aspirin and other antithrombotic agents in the US population. Approximately 70% of 25,686 US outpatients were treated with aspirin, with greater use in the Midwest and among men, whites, and those aged <65 years. Among aspirin users, 18% took other antiplatelet agents and 6% took oral anticoagulants. Low-dose aspirin (≤100 mg/day) was used in approximately 2/3 of aspirin users. Of patients not taking aspirin, 1/2 were receiving oral anticoagulants or other antiplatelet agents. However, 15% of patients used no antithrombotic agent at all. Female gender, current smoking, or having diabetes mellitus were predictors of a lack of antithrombotic use; white race, atrial fibrillation or vascular disease, the use of other risk-reducing medications, or treatment by a cardiologist were associated with a greater likelihood of receiving antithrombotic therapy. In conclusion, approximately 1/4 of US patients with vascular disease are not treated with aspirin for secondary prevention, and 15% are not treated with any antithrombotic agent.
Aspirin irreversibly inhibits the synthesis of thromboxane A 2 , a potent vasoconstrictor and platelet pro-aggregant. Several trials have shown that aspirin doses of 75 to 150 mg will yield a reduction in cardiovascular events similar to that realized with higher doses of 150 to 325 mg/day. In addition, the risk of major bleeding appears to be lower with lower aspirin doses. Current guidelines recommend 75 to 162 mg/day for secondary prevention of atherosclerotic vascular disease. No prospective registry data are available describing aspirin use among outpatients with, or at risk of, clinically manifest atherothrombotic disease in a “real-world” setting. The REduction of Atherothrombosis for Continued Health (REACH) Registry, an international, prospective, observational study, was designed to collect data on an ethnically and geographically diverse population across 44 countries in an outpatient setting. The baseline characteristics and 1-year outcomes of the global REACH Registry population have been published previously. The primary objectives of the present analysis were to (1) describe the use of aspirin, including the rates of use and dosage, among patients enrolled in the United States (US) and (2) identify the independent predictors of aspirin use or nonuse in the US.
Methods
The REACH Registry is an international, prospective, longitudinal study of >68,000 patients across 6 continents recruited from December 2003 to June 2004. The present report was based on a database lock of July 2006. The methods have been described previously. In brief, the patients were eligible for enrollment if they were aged ≥45 years and had ≥1 of the following: (1) ≥3 atherothrombotic risk factors; (2) documented coronary artery disease (CAD); (3) documented cerebrovascular disease; or (4) documented peripheral artery disease (PAD). The exclusion criteria included patients who were already participating in other clinical trials, currently hospitalized patients, and those expected to have difficulty returning for follow-up visits. This protocol was submitted to the institutional review board in each country according to the local requirements, and all patients provided signed informed consent. All data were collected locally using a standard subject data form and forwarded to a central site. The data control audits were performed throughout the data collection period by way of site visits conducted at 10% of all sites that enrolled ≥1 patient (6% selected randomly, 4% selected according to performance level). All case report forms at the audited sites were monitored for documentation and accuracy.
The aspirin dosage at baseline was evaluated overall and in patients grouped by age, gender, race, US Census Region, patient type (asymptomatic with risk factors, CAD at baseline, cerebrovascular disease at baseline, PAD at baseline), previous revascularization, previous coronary angioplasty/stenting, and previous coronary artery bypass grafting without previous revascularization. We also evaluated the different combinations of antiplatelet therapy (eg, clopidogrel, ticlopidine) or oral anticoagulant agents used. Data for aspirin users were represented with and without the missing data points for the dosages used. The present report was prepared in compliance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist.
Descriptive values were calculated using the mean, standard deviation (SD), and range for continuous data and counts and/or percentages for categorical data. Bivariate values were also reported as counts and percentages. Multivariate models of the baseline study end points were constructed using the available baseline variables, consisting of patient level data (medical history, risk factors, sociodemographics, and geographic location) and physician data (specialty, years in practice, and geographic location). Contingency tables, simple Poisson and logistic regression models, and graphics were used to assess the magnitude, direction, and functional form of the bivariate relationships between the baseline factors and the study end points of interest. The method of generalized estimating equations was then used to construct multivariate hierarchical Poisson or logistic regression models, as appropriate, given the event proportions and evidence-supporting, technique-specific assumptions. The US Census Region in which the patient resided was used as a nested level in the hierarchical models, and several correlation structures were tested to identify the best fit. The log-likelihood measure, Akaike Information Criterion, Bayesian information criterion, and Hosmer and Lemeshow’s statistic were used to assess the various dimensions of model fit. Variance inflation factors, tolerance measures, contingency tables, and graphic methods were used to assess the degree of collinearity and multicollinearity during the model-building process and to facilitate model specification. Only subject data with complete information on model variables were included in the final models. Fisher’s exact test was used to compare the categorical variables. No measures were taken to address the potential nonresponse effects of item-level missing data. All statistical hypotheses were tested at α = 0.05. No adjustments were made for multiple comparisons. Odds ratios (ORs) were calculated with their 95% confidence intervals. All statistical calculations were performed using SAS, version 8.2 (SAS Institute, Cary, North Carolina).
Results
A total of 25,686 patients were registered in the REACH database from 1,599 practices in the US. At baseline, 15,360 (59.8%) had CAD, 5,478 (21.3%) had cerebrovascular disease, 2,382 (9.3%) had PAD, and 6,617 (25.8%) were asymptomatic with risk factors only. Of those with CAD, 11,677 had undergone previous angioplasty/stenting or coronary artery bypass surgery. Of those with cerebrovascular disease, 792 had previously undergone carotid angioplasty/stenting or carotid surgery. Of the patients with PAD, 1,558 had a history of lower limb angioplasty/stenting/bypass or amputation.
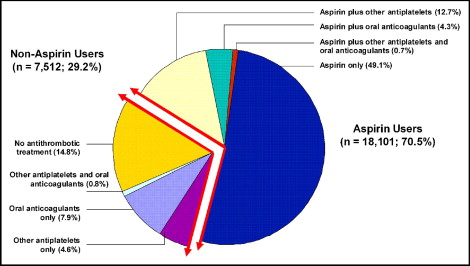
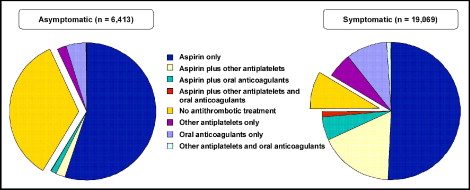
At baseline, 71% of patients reported taking aspirin ( Figure 1 ). Of these patients, 70% used aspirin alone, 18% used aspirin plus other antiplatelet agents, 6% were taking aspirin and an oral anticoagulant, and 1% were taking all 3 antithrombotic classes. Among patients not receiving aspirin, 1/2 used no antithrombotic agent, 27% took oral anticoagulants, 16% used other antiplatelet agents, and 3% were taking both another antiplatelet agent and an oral anticoagulant. Predictably, aspirin use was significantly greater among symptomatic patients than among those with risk factors only (75% vs 59%; p <0.001; Figure 2 ). Approximately 15% of patients used no antithrombotic agent at all ( Figure 1 ). In patients with known disease, 25% were not taking aspirin, among whom 9.1% were not taking any antithrombotic. In the asymptomatic group, 34.5% were not taking antithrombotic medication ( Figure 2 ).
The baseline characteristics of the patients, stratified by antithrombotic use, are listed in Table 1 . Aspirin use was significantly greater among patients aged <65 years than those aged ≥65 years (73.2% vs 69.5%; p <0.001) and among men versus women (74.4% vs 65.7%; p <0.001). Whites had the greatest use of aspirin (71.6%), followed by Hispanics (68.6%), Asians (68.1%), and African-Americans (65.5%; p = 0.017, p = 0.036, p <0.001, respectively, compared to whites). The use of aspirin among the US Census Regions was significantly greater in the Midwest (72.7%) than in the Northeast (70.9%; p = 0.039), South (70.1%; p <0.001), or West (69.3%; p <0.001).
| Variable | Aspirin Users (n = 18,101) | Aspirin Nonusers (n = 7,512) | ||||||
|---|---|---|---|---|---|---|---|---|
| Concomitant Antithrombotic Medication | None (n = 12,612) | Other Antiplatelet Agents Only (n = 3,265) | Oral Anticoagulants Only (n = 1,103) | Both Agents (n = 189) | None (n = 3,795) | Other Antiplatelet Agents Only (n = 11,70) | Oral Anticoagulants Only (n = 2,026) | Both Agents (n = 204) |
| Age (years) | 69.8 ± 10.2 | 68.8 ± 10.6 | 70.8 ± 9.9 | 70.1 ± 10.5 | 69.4 ± 10.7 | 71.1 ± 10.3 | 73.3 ± 9.6 | 70.5 ± 10.5 |
| Age group | ||||||||
| <65 years | 3,913 (31.2%) | 1,179 (36.3%) | 298 (27.2%) | 56 (29.9%) | 1,239 (32.8%) | 325 (27.9%) | 383 (18.9%) | 61 (30.0%) |
| ≥65 years | 8,629 (68.8%) | 2,069 (63.7%) | 799 (72.8%) | 131 (70.1%) | 2,542 (67.2%) | 838 (72.1%) | 1,640 (81.1%) | 142 (70.0%) |
| Gender | ||||||||
| Male | 7,494 (59.5%) | 1,940 (59.5%) | 749 (68.0%) | 118 (62.4%) | 1,743 (45.9%) | 588 (50.3%) | 1,155 (57.0%) | 110 (53.9%) |
| Female | 5,105 (40.5%) | 1,321 (40.5%) | 353 (32.0%) | 71 (37.6%) | 2,051 (54.1%) | 581 (49.7%) | 871 (43.0%) | 94 (46.1%) |
| Race | ||||||||
| White | 10,201 (81.7%) | 2,580 (80.0%) | 942 (86.2%) | 160 (84.7%) | 2,771 (73.7%) | 857 (74.1%) | 1,743 (87.0%) | 171 (84.2%) |
| African-American | 1,215 (9.7%) | 343 (10.6%) | 93 (8.5%) | 14 (7.4%) | 534 (14.2%) | 179 (15.5%) | 157 (7.8%) | 18 (8.9%) |
| Hispanic | 660 (5.3%) | 190 (5.9%) | 37 (3.4%) | 10 (5.3%) | 277 (7.4%) | 68 (5.9%) | 60 (3.0%) | 10 (4.9%) |
| Asian | 339 (2.7%) | 101 (3.1%) | 16 (1.5%) | 3 (1.6%) | 145 (3.9%) | 46 (4.0%) | 28 (1.4%) | 3 (1.5%) |
| Atrial fibrillation | 710 (5.7%) | 240 (7.5%) | 480 (44.4%) | 69 (38.1%) | 181 (4.9%) | 66 (5.8%) | 1,061 (53.1%) | 93 (46.3%) |
| Diabetes | 6,344 (50.6%) | 1,456 (44.8%) | 521 (47.5%) | 92 (48.9%) | 2,377 (63.0%) | 580 (49.8%) | 936 (46.6%) | 97 (47.8%) |
| Current smoking | 1,760 (14.3%) | 457 (14.4%) | 97 (8.9%) | 21 (11.4%) | 666 (18.1%) | 167 (14.8%) | 213 (10.9%) | 25 (12.4%) |
| ≥1 Antihypertensive agent | 11,818 (93.8%) | 3,093 (94.8%) | 1,062 (96.4%) | 182 (96.3%) | 3,490 (92.2%) | 1,090 (93.2%) | 1,926 (95.1%) | 191 (93.6%) |
| ≥1 Lipid-lowering agent | 10,823 (86.0%) | 2,876 (88.4%) | 916 (83.9%) | 172 (91.5%) | 2,961 (78.3%) | 929 (79.6%) | 1,506 (74.5%) | 173 (85.6%) |
| ≥1 Antidiabetic agent | 5,852 (46.5%) | 1,328 (40.8%) | 483 (43.9%) | 83 (44.4%) | 2,217 (58.7%) | 524 (44.9%) | 825 (40.8%) | 90 (44.1%) |
| Risk factors only | 3,346 (26.7%) | 139 (4.3%) | 78 (7.1%) | 7 (3.7%) | 2,098 (56.1%) | 120 (10.4%) | 279 (13.9%) | 16 (7.9%) |
| Symptomatic | 9,178 (73.3%) | 3,123 (95.7%) | 1,019 (92.9%) | 182 (96.3%) | 1,641 (43.9%) | 1,038 (89.6%) | 1,729 (86.1%) | 187 (92.1%) |
| CVD | 1,890 (15.2%) | 1,097 (34.3%) | 346 (32.2%) | 61 (32.6%) | 439 (11.8%) | 499 (43.5%) | 758 (37.9%) | 92 (45.8%) |
| CAD | 7,798 (62.3%) | 2,463 (75.9%) | 845 (77.3%) | 157 (83.5%) | 1,253 (33.6%) | 665 (57.5%) | 1,244 (62.2%) | 140 (69.3%) |
| PAD | 975 (7.7%) | 466 (14.3%) | 133 (12.1%) | 31 (16.4%) | 236 (6.2%) | 177 (15.1%) | 203 (10.0%) | 42 (20.6%) |
| Previous revascularization | ||||||||
| Angio/stent only | 2,307 (18.5%) | 1,099 (34.2%) | 226 (20.9%) | 61 (33.3%) | 287 (7.7%) | 232 (20.1%) | 245 (12.3%) | 45 (22.2%) |
| CABG only | 2,555 (20.5%) | 467 (14.5%) | 259 (23.9%) | 24 (13.1%) | 302 (8.1%) | 149 (12.9%) | 433 (21.7%) | 32 (15.8%) |
| Both | 1,035 (8.3%) | 503 (15.7%) | 183 (16.9%) | 53 (29.0%) | 120 (3.2%) | 107 (9.2%) | 162 (8.1%) | 32 (15.8%) |
| None | 6,576 (52.4%) | 1,144 (35.3%) | 415 (37.9%) | 45 (24.3%) | 3,038 (80.7%) | 669 (57.5%) | 1,151 (57.4%) | 94 (46.1%) |
| Region | ||||||||
| Northeast ⁎ | 2,418 (19.2%) | 528 (16.2%) | 201 (18.2%) | 26 (13.8%) | 660 (17.4%) | 224 (19.1%) | 416 (20.5%) | 39 (19.1%) |
| Midwest † | 3,043 (24.1%) | 940 (28.8%) | 296 (26.8%) | 49 (25.9%) | 860 (22.7%) | 266 (22.7%) | 485 (23.9%) | 42 (20.6%) |
| South ‡ | 4,791 (38.0%) | 1,245 (38.1%) | 411 (37.3%) | 86 (45.5%) | 1,510 (39.8%) | 469 (40.1%) | 744 (36.7%) | 80 (39.2%) |
| West § | 2,231 (17.7%) | 529 (16.2%) | 182 (16.5%) | 27 (14.3%) | 721 (19.0%) | 196 (16.8%) | 359 (17.7%) | 41 (20.1%) |
⁎ Maine, New Hampshire, Vermont, Massachusetts, Rhode Island, Connecticut, New York, New Jersey, Pennsylvania.
† Ohio, Indiana, Illinois, Michigan, Wisconsin, Minnesota, Iowa, Missouri, North Dakota, South Dakota, Nebraska, Kansas.
‡ Delaware, Maryland, District of Columbia, Virginia, West Virginia, North Carolina, South Carolina, Georgia, Florida, Kentucky, Tennessee, Alabama, Mississippi, Arkansas, Louisiana, Oklahoma, Texas.
§ Montana, Idaho, Wyoming, Colorado, New Mexico, Arizona, Utah, Nevada, Washington, Oregon, California, Alaska, Hawaii.
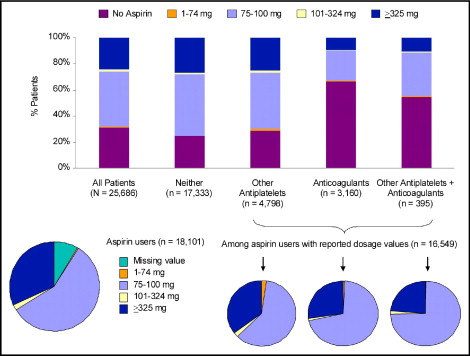
Most patients who reported aspirin use at baseline were taking a low dose (75 to 100 mg) instead of a higher dose (≥325 mg). Although the total number of those who reported taking aspirin was 18,101, dosage information was available for only 16,549 patients, among whom nearly 2/3 used aspirin 75 to 100 mg/day ( Figure 3 and Table 2 ). Only 2% of patients took a “medium” dose (101 to 324 mg). Patients given the higher dose of aspirin were more often younger, male, and white ( Table 2 ). More patients with CAD took high-dose aspirin compared with those with cerebrovascular disease or PAD ( Table 2 ). Similar to the overall population of aspirin users, patients taking aspirin only (without other antithrombotic agents) primarily used low-dose aspirin ( Figure 3 ). Patients taking aspirin and an oral anticoagulant, with or without other antiplatelet agents, more often used low-dose versus high-dose, aspirin ( Figure 3 ).
| Variable | Missing or 0 mg ⁎ (n = 1,552) | 1–74 mg (n = 123) | 75–100 mg (n = 10,310) | 101–324 mg (n = 347) | ≥325 mg (n = 5,769) |
|---|---|---|---|---|---|
| Age (years) | 70.3 ± 10.5 | 70.0 ± 10.2 | 70.2 ± 10.3 | 70.3 ± 9.8 | 68.6 ± 10.2 |
| Age group | |||||
| <65 years | 445 (29.1%) | 35 (28.9%) | 3,068 (29.9%) | 111 (32.1%) | 2,117 (36.9%) |
| ≥65 years | 1,086 (70.9%) | 86 (71.1%) | 7,187 (70.1%) | 235 (67.9%) | 3,618 (63.1%) |
| Gender | |||||
| Male | 905 (58.5%) | 67 (54.9%) | 5,877 (57.1%) | 239 (68.9%) | 3,760 (65.2%) |
| Female | 642 (41.5%) | 55 (45.1%) | 4,419 (42.9%) | 108 (31.1%) | 2,004 (34.8%) |
| Race | |||||
| White | 1,137 (74.5%) | 93 (76.9%) | 8,214 (80.5%) | 311 (90.4%) | 4,816 (84.2%) |
| African-American | 214 (14.0%) | 16 (13.2%) | 1,019 (10.0%) | 20 (5.8%) | 523 (9.1%) |
| Hispanic | 103 (6.7%) | 8 (6.6%) | 589 (5.8%) | 3 (0.9%) | 256 (4.5%) |
| Asian | 57 (3.7%) | 4 (3.3%) | 322 (3.2%) | 7 (2.0%) | 100 (1.7%) |
| Atrial fibrillation | 143 (9.4%) | 11 (9.2%) | 955 (9.5%) | 34 (10.1%) | 425 (7.5%) |
| Diabetes | 784 (51.1%) | 46 (37.7%) | 5,236 (51.1%) | 152 (44.7%) | 2,668 (46.4%) |
| Current smoking | 203 (13.6%) | 22 (18.0%) | 1,348 (13.4%) | 46 (13.5%) | 850 (15.0%) |
| ≥1 Antihypertensive agent | 1,471 (95.1%) | 114 (92.7%) | 9,697 (94.2%) | 321 (92.5%) | 5,435 (94.2%) |
| ≥1 Lipid-lowering agent | 1,326 (86.4%) | 101 (82.1%) | 8,805 (85.8%) | 301 (86.7%) | 5,040 (87.6%) |
| ≥1 Antidiabetic agent | 734 (47.7%) | 44 (35.8%) | 4,842 (47.1%) | 140 (40.3%) | 2,428 (42.2%) |
| Risk factors only | 338 (22.0%) | 16 (13.0%) | 2,608 (25.5%) | 52 (15.2%) | 763 (13.3%) |
| Symptomatic | 1,197 (78.0%) | 107 (87.0%) | 7,632 (74.5%) | 291 (84.8%) | 4,988 (86.7%) |
| Cerebrovascular disease | 380 (25.0%) | 67 (55.4%) | 1,947 (19.2%) | 68 (20.0%) | 1,127 (19.9%) |
| Coronary artery disease | 969 (63.3%) | 53 (43.1%) | 6,316 (61.8%) | 246 (71.9%) | 4,289 (74.7%) |
| Peripheral artery disease | 166 (10.7%) | 12 (9.8%) | 941 (9.1%) | 35 (10.1%) | 536 (9.3%) |
| Previous revascularization | |||||
| Angiography/stent only | 270 (17.9%) | 13 (10.8%) | 1,971 (19.4%) | 78 (22.7%) | 1,555 (27.3%) |
| Coronary artery bypass grafting only | 256 (16.9%) | 16 (13.3%) | 1,856 (18.2%) | 83 (24.1%) | 1,268 (22.3%) |
| Both | 164 (10.9%) | 13 (10.8%) | 929 (9.1%) | 43 (12.5%) | 716 (12.6%) |
| None | 821 (53.7%) | 78 (63.9%) | 5,423 (52.9%) | 140 (40.6%) | 2,148 (37.5%) |
| Region | |||||
| Northeast † | 328 (21.1%) | 21 (17.1%) | 1,849 (17.9%) | 66 (19.0%) | 1,112 (19.3%) |
| Midwest ‡ | 378 (24.4%) | 42 (34.1%) | 2,500 (24.2%) | 88 (25.4%) | 1,537 (26.6%) |
| South § | 579 (37.3%) | 40 (32.5%) | 3,926 (38.1%) | 118 (34.0%) | 2,224 (38.6%) |
| West ¶ | 244 (15.7%) | 19 (15.4%) | 1,931 (18.7%) | 71 (20.5%) | 847 (14.7%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


