Pathologic features that characterize hypertrophic cardiomyopathy (HC) in exertional versus nonexertional sudden deaths have not been extensively studied. We performed gross measurements and histologic analysis on 103 autopsy cases of HC and correlated these with clinical findings. Pathologic features of the 71 sudden deaths were compared between exertional and nonexertional deaths. Age at death was significantly younger in exertional (27 ± 13 years) versus nonexertional sudden deaths (40 ± 16 years, p = 0.0003). Exertional deaths were more likely in women (35 of 37) versus sudden deaths at rest (21 of 34, p = 0.0002). There was no significant difference in the incidence of syncope in the exertional sudden deaths (14%) compared to the nonexertional sudden deaths (9%, p = 0.5) or in the rate of a previous diagnosis of HC (21% vs 21%, respectively). Mean heart weight was significantly decreased in exertional sudden deaths versus nonexertional sudden deaths. There was no difference in the frequency of left ventricular outflow tract plaque (54% exertional vs 46% nonexertional, p = 0.06). By multivariate analysis, including all categories of HC, only decreased heart weight (p = 0.02) and male gender (p = 0.002) were significantly associated with exertional sudden death. In conclusion, there are no pathologic features that would identify patients with HC at risk for exertional death. Because relatively decreased heart weight is strongly associated with exertional death, and because a large proportion of exertional deaths with HC are not associated with significant asymmetry, cardiologists should be careful in excluding the diagnosis of HC in athletes with even mild degrees of cardiomegaly, especially young men.
Autopsy studies have demonstrated that there are no reliable morphologic criteria that are associated with sudden death in patients with hypertrophic cardiomyopathy (HC). Although a large proportion of patients with sudden death had markedly thickened ventricular septa (>20 mm), survivors of cardiac arrest had similar septal dimensions, and hemodynamic parameters including outflow tract obstruction did not identify patients with HC who died suddenly. The present series was undertaken to determine if certain clinicopathologic parameters are increased in exertional deaths compared to deaths at rest and those due to heart failure or other causes.
Methods
A retrospective review of 103 cases of HC was undertaken from a series referred to the same consultants who reviewed each case in a standardized manner. Clinical information was acquired from the medical examiner or hospital pathologist. Family history and circumstances of death were obtained by review of investigators’ records or hospital charts. Institutional review board approval was granted for the study.
Criteria for inclusion into study were that the heart specimen was reviewed per gross heart protocol, with uniform sections taken in each case. Diagnostic criteria for HC were (1) the presence of pathologic myofiber disarray and (2) the lack of other conditions, such as amyloid or Fabry disease, which may cause cardiac hypertrophy and asymmetry. Myofiber disarray was defined as marked (≥4 times) increase in myocyte size diameter and myocyte nuclear size compared to reference myocytes and presence of branched or bifurcating myocytes or presence of haphazardly arranged groups or bundles of myocytes. Reference myocytes indicates those subendocardial areas remote from the midseptal or midventricular area of hypertrophy.
Gross evaluation included weighing the heart after removal of arch vessels, cavitary blood, and pericardium; routine measurements of the ventricular septum and left ventricular free wall thicknesses at the level of the papillary muscles; description of outflow tract; description of coronary arteries including tunneling; and description of gross ventricular fibrosis with gross photography. Histologic sections were taken in a standardized way and included the anterior, lateral, and posterior left ventricle; the anterior and posterior ventricular septum near the base; and the posterior right ventricle. In cases of suspected apical disease or if there were other gross findings, additional sections were taken. For purposes of the present study, histologic sections were re-reviewed to characterize myofiber disarray, histologic fibrosis, and intramural coronary artery dysplasia.
Myofiber disarray was characterized as whorled or cartwheel pattern, linear pattern, bundled pattern, or mixed pattern, similar to a previous description. The extent in each section was semiquantitated as 0 to 4+ with 0 indicating absent; 1+ focal; 2+ <1/3 of section area; 3+ 1/3 to 2/3 of section area; and 4+ >2/3 of section area. When necessary, morphometric area measurements were made using a SPOT Insight Digital camera (Sterling Heights, Michigan) mounted on an Olympus BX41 (Olympus America Inc., Center Valley, Pennsylvania) microscope. A score was recorded for each section and a sum of 6 sections (anterior, posterior, and lateral left ventricle, anterior and posterior septum, and posterior right ventricle).
Histologic fibrosis was estimated on a 0 to 4+ scale using a Masson trichrome stain; 1+ indicated focal replacement fibrosis, 2+ replacement fibrosis 25% of the section area; 3+ replacement fibrosis 26% to 50% of the section area, and 4+ >50% of the section area. When necessary, morphometric area measurements were made using a SPOT Insight Digital camera mounted on an Olympus BX41 microscope. A score was recorded for each section and a sum of 6 sections (anterior, posterior and lateral left ventricle, anterior and posterior septum, and posterior right ventricle).
Intramural coronary thickening score was graded as 0 to 4+; 1+ indicated 1 thickened artery per section, 2+ 2 to 3 thickened arteries per section, 3+ 4 to 5 thickened arteries per section or any intramural artery >0.5 mm in diameter, and 4+ >5 thickened arteries per section or ≥2 thickened areas >0.5 mm in diameter.
Areas of subepicardial scarring with or without fatty replacement were recorded as were lymphoid infiltrates in any section.
Clinical and pathologic parameters were compared using Student’s t tests for parametric data and Mann-Whitney unpaired t tests for nonparametric data. Differences across multiple groups were studied by analysis of variance with Fisher’s post hoc test. Association between continuous parameters was studied using simple regression. Statistical analysis was performed using JMP software (SAS Institute, Cary, North Carolina).
Results
Of the 103 deaths, patients with nonsudden deaths (32) were significantly older and more likely to have a history of HC ( Table 1 ). Sudden death cases had significantly decreased heart weight and higher intramural coronary artery thickening score ( Table 2 ) compared to nonsudden deaths.
| Variable | Age at Death (years), Mean ± SD | Men:Women | White:Black:Other | History of HC | Family History | History of Unexplained Syncope |
|---|---|---|---|---|---|---|
| Nonsudden (n = 32) | 52 ± 15 | 24:7 | 14:16:1 | 14 | 1 | 1 |
| Incidental finding (n = 20) | 49 ± 13 | 18:2 | 6:13:1 | 3 | 0 | 0 |
| Heart failure (n = 11) | 54 ± 18 | 6:5 | 8:3:0 | 11 | 1 | 1 |
| Sudden (n = 71) | 33 ± 16 | 57:15 | 40:32:0 | 15 | 9 | 8 |
| Sudden unexpected death at rest (n = 34) | 40 ± 16 | 21:13 | 16:18:0 | 7 | 3 | 3 |
| Sudden unexpected death during exertion (n = 37) | 27 ± 13 | 36:2 | 24:14:0 | 8 | 6 | 5 |
| Total (n = 103) | 39 ± 18 | 81:22 | 54:48:1 | 25 | 10 | 9 |
| p value, sudden vs nonsudden | 0.0001 | 0.9 | 0.2 | 0.01 | 0.1 | 0.1 |
| p value, exertional vs nonexertional sudden deaths | 0.0003 | 0.0002 | 0.2 | 0.5 | 0.3 | 0.3 |
| Variable | Non-SCD | Incidental | Heart Failure | SCD | SCD at Rest | Exertional Sudden Death |
|---|---|---|---|---|---|---|
| (n = 32) | (n = 20) | (n = 11) | (n = 71) | (n = 34) | (n = 38) | |
| Heart weight (g), mean ± SD | 685 ± 143 | 719 ± 135 | 618 ± 145 | 600 ± 178 | 659 ± 193 | 547 ± 148 |
| Maximal ventricular septum thickness (mm), mean ± SD | 24.0 ± 5.3 | 23 ± 3 | 27 ± 6 | 22.8 ± 7.0 | 23 ± 8 | 21 ± 6 |
| Ventricular septum: left ventricular free wall ratio, mean ± SD | 1.3 ± 0.2 | 1.3 ± 0.2 | 1.4 ± 0.3 | 1.3 ± 0.4 | 1.3 ± 0.5 | 1.3 ± 0.3 |
| %Ventricular septum: left ventricular free wall <1.1 | 87 | 86 | 91 | 77 | 79 | 75 |
| %Ventricular septum: left ventricular free wall <1.3 | 45 | 43 | 55 | 49 | 48 | 47 |
| Left ventricular outflow tract plaque | 39% | 35% | 45% | 51% | 46% | 54% |
| Gross fibrosis, septum | 43% | 42% | 45% | 47% | 52% | 43% |
| Left anterior descending coronary artery tunnel | 7% | 5% | 9% | 13% | 9% | 17% |
| Histologic disarray score | 4.8 ± 2.6 | 5.1 ± 2.9 | 4.0 ± 0.8 | 6.4 ± 2.9 | 5.6 ± 2.7 | 7.2 ± 2.8 |
| Histologic fibrosis score | 4.3 ± 3.9 | 4.2 ± 3.2 | 4.4 ± 2.3 | 4.8 ± 3.0 | 4.8 ± 2.6 | 4.8 ± 3.5 |
| Any intramural coronary artery thickness | 48% | 55% | 36% | 67% | 62% | 71% |
| Intramural coronary artery thickening score | 1.2 ± 1.7 | 1.1 ± 1.3 | 1.5 ± 2.3 | 2.5 ± 2.6 | 2.8 ± 2.9 | 2.2 ± 2.3 |
| Areas of subepicardial fibrofatty areas, left ventricle | 0 | 0 | 0 | 3/71 | 1/34 | 2/37 |
Of the 71 sudden cardiac deaths (SCDs), 37 occurred during exertion. Exertional deaths included 13 while running or jogging, 11 while playing basketball, 3 during physical labor, 2 during soccer, 2 during gym workouts, 2 during emotional stress (physical assault, spectator at soccer game), and 1 each during boxing, childbirth, swimming, football, and hockey. Of exertional deaths, 8 had previous HC, 1 with an automatic implantable cardioverter–defibrillator, 1 with a pacemaker, and 1 had discontinued β blockers 3 months before death. Of those without a history, 2 had previous syncope, 1 the day before death. Six had a family history of HC, 1 of whom had a negative evaluation including echocardiogram the week before death. Thirty-four sudden deaths occurred during rest: 6 had previous HC, 3 had a history of unexplained syncope, and the remainder had no medical history. There were 20 cases with incidental HC, and deaths were attributed to severe coronary artery disease with thrombosis (n = 5), drug overdose (n = 6), suicide (n = 2), trauma (n = 5), pulmonary embolism (n = 1), and aortic dissection (n = 1). Of these, 3 had previous HC, but none had heart failure. Eleven patients died with end-stage HC and heart failure. Age at death was significantly younger in exertional versus nonexertional deaths (p = 0.0003; Table 1 ), and exertional deaths were primarily in men (p = 0.0002; Table 1 ).
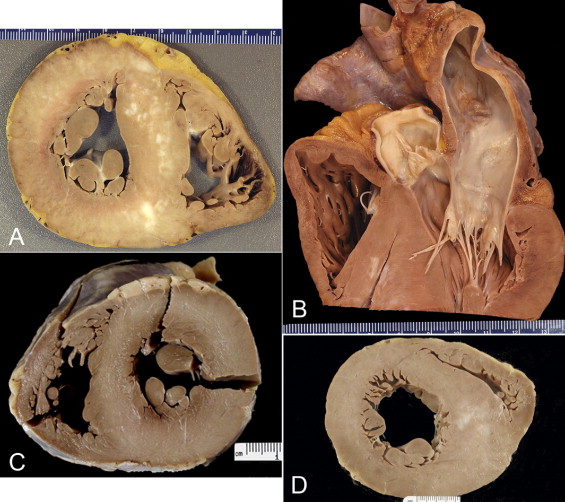
Gross and microscopic findings are presented in Figures 1 and 2 and Table 2 . Mean heart weight was significantly decreased in sudden versus nonsudden deaths (p = 0.02), and the intramural coronary artery thickening score was higher (p = 0.02; Figure 3 ). Between exertional and nonexertional sudden deaths, the myofiber disarray score was higher in exertional deaths (p = 0.01) and heart weight was decreased (p = 0.008). The difference in heart weight was significant only in men (p = 0.006); there were only 2 exertional deaths in women.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


