Fractional flow reserve (FFR) is widely used for the assessment of myocardial ischemia. However, it has the disadvantage of cost and invasive complication risks. We investigated the usefulness of quantitative coronary angiography–derived translesional pressure (QCA-TP) for predicting functional myocardial ischemia, using FFR as the gold standard. We retrospectively analyzed 152 coronary narrowings (98 left anterior descending arteries, 28 left circumflex arteries, and 26 right) in 132 patients with mild-severe coronary stenosis who underwent coronary angiography and FFR measurements simultaneously. QCA-TP was calculated using software implemented in the QCA software. Coronary morphology was calculated using both densitometry and lumen edges. Functional myocardial ischemia was defined as an FFR of 0.8 or less. The mean values of diameter stenosis by QCA and FFR were 48.9% ± 14.9 and 0.76 ± 0.14, respectively. QCA-TP was significantly correlated with FFR ( r = 0.76, p <0.01). The cut-off values of QCA-TP for predicting functional myocardial ischemia based on FFR were 72.8 mm Hg for the left anterior descending arteries (accuracy, 86.7%; area under the curve [AUC], 0.93), 60.5 mm Hg for the left circumflex arteries (accuracy, 89.3%; AUC, 0.88), and 64.4 mm Hg for the right (accuracy, 88.5%; AUC, 0.94). Therefore, our data suggest that QCA-TP can predict myocardial ischemia with high diagnostic accuracy.
Fractional flow reserve (FFR)–guided percutaneous coronary intervention reduces major adverse cardiac events. FFR evaluation is invasive and expensive in cost. Quantitative coronary angiography (QCA) allows reproducible stenosis evaluation in comparison with visual assessment. Morphologic details assessed by conventional QCA do not completely reflect the entire physiological impact. By current QCA software (CAAS II; Pie Medical Imaging BV, Maastricht, the Netherlands), the coronary lumen area can be calculated using densitometry, resulting in a more precise stenosis evaluation. A close relation was found between QCA-derived translesional pressure (QCA-TP) and coronary flow reserve. However, the validity of the FFR and the QCA-TP in clinical settings has not yet been fully established. The purpose of this study was to investigate the usefulness of QCA-TP for predicting functional myocardial ischemia.
Methods
We retrospectively analyzed 152 lesions in 132 patients with stable angina pectoris who underwent both coronary angiography and FFR for the assessment of myocardial ischemia from January 2011 to March 2016 at Ehime University Graduate School of Medicine. Patients who had angiographically diffuse coronary artery stenosis, significant left main coronary artery disease, in-stent restenosis disease, graft disease, severe systolic dysfunction (left ventricular ejection fraction, ≤40%), or an infarct-related artery were excluded from the present study. The institutional review boards of our hospital approved the retrospective use of patient data.
Diagnostic coronary angiography was performed using 4Fr to 6Fr coronary catheters. Intracoronary isosorbide dinitrate (1.25 mg) was administered before the angiogram and a pressure-monitoring guidewire (Verrata or Prime Wire Prestige PLUS or Prime Wire; Volcano, San Diego, California) was advanced into the distal coronary vessel past and through the lesion. Hyperemia was induced by intravenous administration of adenosine triphosphate (0.16 mg/kg/min), as previously reported. Functional myocardial ischemia was determined as an FFR 0.8 or less, according to previous reports.
QCA analysis was performed by an experienced QCA analyst who was blinded to the FFR results. QCA was performed offline using automated software (CAAS II; Pie Medical Imaging BV). Angiographic views with the least foreshortening and yielding the best depiction of the stenoses were used. Measurements were performed on image sequences adequately filled with contrast and on the lesion of interest. Proximal and distal reference locations were determined manually to cover the entire lesion and to measure the diameter of the normal segment of the vessel ( Figure 1 ). When there were tandem lesions, both lesions were covered manually. The absolute reference diameter, minimum lumen diameter, diameter stenosis, and lesion length were calculated using the contrast-filled angiographic catheter as a scaling device ( Figure 1 ).
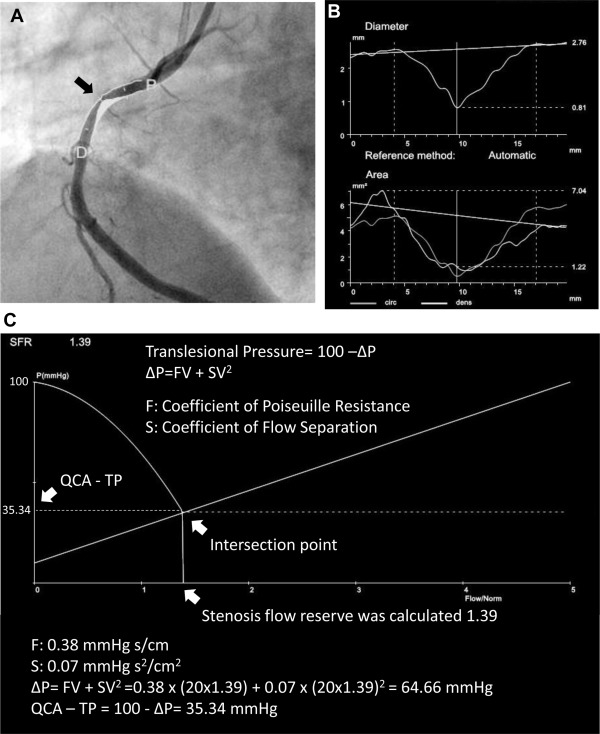
TPs were determined by software integrated in the CAAS II ( Figure 1 ). Gould et al have shown that the calculated pressure gradient (ΔP) across a stenosis can be described by the following simplified equation: ΔP = FV + SV 2 . The coefficients F and S are determined by the morphology of the coronary stenosis. F is the coefficient of pressure loss due to viscous friction (Poiseuille resistance), and S is the coefficient of pressure loss due to exit separation (flow separation). Assuming that the normal coronary flow is defined as 20 cm/s, QCA-TP was defined as the following equation: QCA − TP = 100 − ΔP. Assuming that a patient has a mean arterial pressure of 100 mm Hg and a coronary flow that can increase to 5 times its value at rest without stenosis, one can then graphically determine the stenosis flow reserve (SFR) by plotting coronary pressure (distal to the stenosis) against relative coronary flow. Distal coronary pressure decreases nonlinearly as relative coronary flow increases until hyperemia. The intersection of the curve (100 − ΔP), with the line representing coronary perfusion pressure under hyperemia is the SFR of that region for the flow in the distal coronary vascular bed under conditions of hyperemia. QCA-TP was shown at the point (pressure) of SFR, which is the intersection point between the 2 lines ( Figure 1 ). A representative case is shown in Figure 1 . The time necessary to measure QCA-TP was only several seconds in addition to the QCA analysis.
Statistical analysis was performed using IBM SPSS Statistics, version 18.0 (IBM, Armonk, New York). Categorical variables were summarized using counts and percentages. Continuous variables were presented as mean ± SD. Receiver-operating characteristics curve analysis was used to identify the cut-off value predictive of functional myocardial ischemia. Difference between the 2 groups with and without FFR ≤0.8 was assessed with the chi-square test for categorical variables and with unpaired Student t -test for continuous variables. Multiple regression analysis was performed to identify the independent predictors of FFR. A value of p <0.05 was considered significance.
Results
QCA and FFR assessments included 98 left anterior descending arteries (LADs), 28 left circumflex arteries (LCs), and 26 right from 132 patients with stable angina pectoris. Baseline clinical characteristics are presented in Table 1 . The mean patient age was 70.0 ± 10.2 years and male gender was 70%. Lesion characteristics are presented in Table 2 . The mean values of percent diameter stenosis, FFR, and QCA-TP were 48.9% ± 14.9, 0.76 ± 0.14, and 65.3 ± 20.1 mm Hg, respectively. Intraobserver and interobserver error was −0.5 ± 8.6 mm Hg ( r = 0.96) and −4.5 ± 9.9 mm Hg ( r = 0.91), respectively.
| Age (years) | 70.0 ± 10.2 |
| Men | 92 (70%) |
| Height (cm) | 160.9 ± 8.0 |
| Body weight (kg) | 62.1 ± 11.7 |
| Body mass index (kg/m 2 ) | 23.9 ± 3.5 |
| Hypertension | 87 (66%) |
| Dyslipidemia | 84 (64%) |
| Current smoker | 27 (20%) |
| Diabetes mellitus | 54 (41%) |
| Previous myocardial infarction | 6 (5%) |
| Previous percutaneous coronary intervention | 41 (31%) |
| Previous coronary artery bypass graft | 1 (1%) |
| Index coronary artery | |
| Left anterior descending | 98 (64%) |
| Left circumflex | 28 (18%) |
| Right | 26 (17%) |
| Lesion morphology | |
| Regular | 119 (78%) |
| Irregular | 33 (22%) |
| Concentric plaque | 110 (72%) |
| Eccentric plaque | 42 (28%) |
| Tandem lesion | 29 (19%) |
| Quantitative coronary angiography analysis | |
| Percent diameter stenosis (%) | 48.9 ± 14.9 |
| Minimum lumen diameter (mm) | 1.33 ± 0.48 |
| Reference vessel diameter (mm) | 2.62 ± 0.56 |
| Lesion length (mm) | 17.5 ± 12.4 |
| Quantitative angiography derived translesional pressure (mm Hg) | 65.3 ± 20.1 |
| Fractional flow reserve measurement | |
| Fractional flow reserve | 0.76 ± 0.14 |
| Fractional flow reserve ≤ 0.8 | 83 (54%) |
| Lesion with diameter stenosis > 50% and fractional flow reserve > 0.8 | 11 (7%) |
| Lesion with diameter stenosis ≤ 50% and fractional flow reserve ≤ 0.8 | 21 (14%) |
Correlations between FFR and QCA-TP are shown in Figure 2 . FFR and QCA-TP had a significant positive correlation with coronary arteries overall ( r = 0.76, p <0.001, Figure 2 ). Even in each coronary artery, a good correlation was observed between FFR and QCA-TP ( Figure 3 ). Receiver-operating characteristics analysis showed each QCA-TP cut-off value that predicted functional myocardial ischemia (FFR ≤0.8): 72.8 mm Hg for the LADs (area under the curve [AUC] = 0.93), 60.5 mm Hg for the LCs (AUC = 0.88), and 64.4 mm Hg for the right (AUC = 0.94; Figure 4 ). These QCA-TP cut-off values predicted FFR-based myocardial ischemia with a high diagnostic accuracy ( Table 3 ).




