Intermediate coronary artery stenosis (≥50% and <90%) on coronary computed tomography angiography (CTA) is usually considered as a significant lesion. However, anatomical diagnosis is not well correlated with the functional significance of myocardial ischemia. We investigated whether functional testing in addition to coronary CTA improves outcomes of patients with intermediate stenosis, compared with the 1-step CTA-alone–based strategy. From 2006 to 2011, we consecutively enrolled 335 patients with chest pain with intermediate stenosis detected by an initially performed coronary CTA. Of these, 159 patients followed the 1-step strategy, whereas 176 followed the 2-step strategy with confirmatory functional tests. One-year follow-up data were obtained for all patients. The primary end point was a composite of cardiovascular death, nonfatal myocardial infarction, and repeated or delayed revascularization (major adverse cardiac event) within a year. Baseline clinical parameters were comparable between patients of the 2 different strategies. The rate of invasive catheterization or percutaneous intervention was 75.5% in the 1-step group and 35.2% in the 2-step group (p <0.001). Consequently, more patients in the 2-step group were medically treated without unnecessary revascularization compared with patients in the 1-step group (71.0% vs 40.9%, p <0.001). Only 2.5% of the patients who received medical treatment in the 2-step group finally received delayed revascularization, whereas 14% in the 1-step group did. Overall, the primary end point occurred in 11.3% in the 1-step group and 4.0% in the 2-step group (p = 0.011). In conclusion, confirmatory functional testing reduces invasive catheterization and coronary intervention and improves clinical outcomes in patients with intermediate stenosis on coronary CTA.
Highlights
- •
We compare 2 strategies for intermediate stenosis detected on coronary CTA.
- •
CTA-alone–based 1-step strategy causes invasive catheterization and intervention.
- •
Functional testing in addition to coronary CTA stops unnecessary revascularization.
- •
Functional testing in addition to coronary CTA improves clinical outcomes.
- •
Two-Step strategy with functional testing might be more proper management strategy.
For patients with an intermediate coronary artery stenosis (i.e., severity ≥50% and <90%) detected by coronary computed tomography angiography (CTA), proper management strategies are needed to identify the patients prone to myocardial ischemia and to treat them appropriately without unnecessary invasive procedures. Without an established strategy, some patients are treated medically and some undergo invasive angiography or revascularization directly, whereas others have further confirmatory stress tests including treadmill or fractional flow reserve (FFR). Functional approach such as FFR-guided intervention seemed to result in better outcomes in patients with multivessel coronary artery disease. However, for intermediate coronary lesions on CTA, it is still unclear whether routine confirmatory functional tests have a beneficial role in guiding the treatment strategy. Therefore, we investigate whether functional diagnosis which followed coronary CTA (2 step strategy) improves clinical outcomes compared with coronary CTA-alone–based (1 step) strategy for patients with intermediate coronary artery stenosis.
Methods
From January 2006 to December 2011, we recruited all the patients who had chest pain and underwent coronary CTA as an initial assessment into the coronary CTA registry of the Seoul National University Hospital. In most cases of the registry, coronary CTA was performed, in whom the cause of chest pain is truly uncertain or the probability of coronary artery disease was low to intermediate (i.e., 20% to 70%). In a total of 1,855 patients in the registry, 545 patients were found to have had an intermediate (50% to 89%) coronary artery stenosis and they were included in this study ( Figure 1 ). Then, we excluded those patients who had (1) significant electrocardiographic (ECG) changes and positive cardiac markers, (2) a history of revascularization or myocardial infarction (MI), (3) severe co-morbidities, such as cancer, (4) serum creatinine ≥2.0 mg/dl or diabetes with serum creatinine ≥1.5 mg/dl, and (5) who were lost to follow-up within 1 year. Significant ECG changes were defined as an ST-segment elevation or observable reversible ST-segment depression ≥0.5 mm in at least 2 contiguous leads or evolution of changes in T-wave polarity of an ischemic nature. Finally, we studied a total of 335 patients with lesions with intermediate stenosis who initially underwent coronary CTA ( Figure 1 ). This study was approved by the Institutional Review Board of the Seoul National University Hospital and conducted in accordance with the principles of the 1996 Declaration of Helsinki of the World Medical Association. Written informed consent for data collection and analysis was obtained from all patients.

The coronary CTA was performed for all patients using a 64-detector row CT scanner (Brilliance 64; Philips Medical Systems, Best, The Netherlands). All subjects whose prescanning heart rate ≥65 beats/min were given 100 mg of oral metoprolol (Betaloc; AstraZeneca, Sodertalje, Sweden) 45 to 60 minutes before the CT examination, unless a subject had a contraindication for taking ß blocker. We administered 0.2 mg of sublingual nitroglycerin (Nitroquick; Ethex, St. Louis, MO) to all the subjects immediately before image acquisition for coronary vasodilation. During acquisition, 90 ml of a non-iodine contrast medium (Ultravist 370; Schering, Berlin, Germany) was injected into an antecubital vein followed by a saline flush, both at a flow rate of 4 ml/s. Details of CT scan protocol have been described in the previous studies.
Invasive coronary angiography (CAG) and percutaneous interventions (PCIs) were performed using conventional techniques. In the case of PCIs, some patients underwent stenting directly with angiographic guidance alone, so-called “angiographic PCI.” Others received functional assessment and underwent stenting only if their results were positive, so-called “functional PCI.” The choice of procedure (stent, predilation, post-stent adjunctive balloon inflation, and use of glycoprotein IIb/IIIa inhibitor) was left to the operators’ discretion. All patients who underwent PCI were pretreated with aspirin and clopidogrel. Aspirin was maintained indefinitely and clopidogrel for at least 12 months.
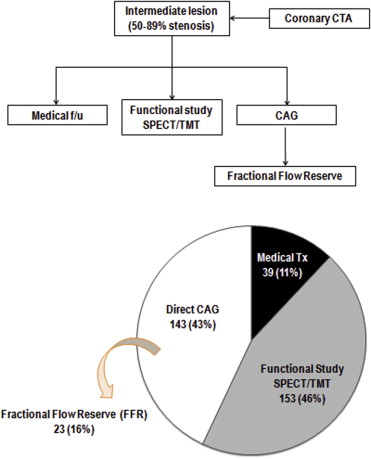
In the “2-step strategy” group, 3 types of functional studies were performed to evaluate the functional significance of anatomical stenosis: treadmill test (TMT), single-photon emission computed tomography (SPECT), and FFR. TMTs were conducted in 83 patients and SPECT in 85 patients. Among these, 15 patients were evaluated by both TMT and SPECT. FFR was measured in 23 patients without preceding noninvasive functional tests ( Figure 2 ). In this group, patients were considered for stenting of indicated lesions only if the results of noninvasive stress tests were positive or the FFR <0.80. Patients who underwent >2 functional tests were considered as positive if the results were positive in at least 1 test.
Gamma cameras equipped with high-resolution, parallel hole collimators (Prism 3000, Picker or Vertex; ADAC, Houston, Texas) were used for the SPECT studies. The consumption of caffeine-rich food and the intake of nitrates or calcium-channel blockers was forbidden for at least 24 hours before the study and the patients came in a fasted state to the Department of Nuclear Medicine. SPECT in rest was first obtained for 10 minutes after the injection of thallium-201. The dose of thallium-201 was adjusted according to the body weight, that is, 74 MBq for <40 kg, 111 MBq for 40 to 70 kg, and 129.5 MBq for >70 kg. After the rest image acquisition, adenosine 0.14 mg/kg/min was infused over 6 minutes and technetium-99m (Tc-99m)-sestamibi (925 MBq) was injected at 3 minutes after the adensosine infusion started. Thirty minutes later, a fatty meal (1 whole egg and 180 ml of milk) was ingested to eliminate the gall bladder activity of Tc-99m-sestamibi. The gated stress SPECT was performed 1 hour after Tc-99m-sestamibi injection. ECG gating was performed using frame-mode (8 frames per cardiac cycle) acquisition.
Two nuclear medicine physicians with expertise in nuclear cardiology interpreted in consensus the regional myocardial perfusion and wall motion. A standard 17-myocardial segment model was used in the study. Perfusion status was graded semiquantitatively using a 4-point system (normal = 0, mild decrease = 1, moderate decrease = 2, and severe defect = 3). Wall motion was also graded using a 4-point system (normal = 0, hypokinesia = 1, akinesia = 2, and dyskinesia = 3). The presence of stress/rest reversibility was defined as at least 1 grade improvement of rest perfusion compared with the stress perfusion decrease or defect.
The coronary CTA registry included demographic, clinical, and laboratory data and prescription records of medications in all patients. We examined the nature of chest pain and clinical risk factors including gender, age, diabetes, hypertension, dyslipidemia, smoking, and family history of early coronary disease. In addition, we analyzed the laboratory risk factors: total cholesterol, low-density lipoprotein, high-density lipoprotein, triglycerides, fasting blood sugar, hemoglobin, blood urea nitrogen, and creatinine. We also reviewed the prescription records of medical treatments with agents such as beta-blockers, calcium channel blockers, inhibitors of angiotensin-converting enzyme, angiotensin II receptor blockers, nitrates, and statins.
We analyzed the rate of invasive catheterization or PCI in each group, and 1-year follow-up data were obtained for all patients. The primary end point was a composite of cardiovascular death, nonfatal MI, and repeat or delayed revascularization (major adverse cardiac event [MACE]) at 1 year. MI was defined as an elevation of the creatine kinase MB fraction by a factor of 3 or more or new Q waves in 2 or more contiguous leads of the electrocardiogram. Delayed revascularization was defined as clinically driven interventional or surgical treatment of an index vessel with intermediate stenosis on coronary CTA after adequate medical treatment for at least 3 months. The secondary end point was a composite of heart failure, nonfatal stroke, and MACE at 1 year.
Continuous variables are expressed as means ± SD, whereas categorical variables, including the end points and their components, are presented as absolute values and proportions. Differences between continuous variables were analyzed by the unpaired Student t test and those between categorical variables by the chi-square test or Fisher’s exact test, as appropriate. A p value <0.05 was considered to be statistically significant. Kaplan-Meier curves are shown for the time-to-event distributions of the primary and secondary end points. All statistical analyses were performed using SPSS, version 18.0 (SPSS Inc., Chicago, Illinois).
Results
For all patients, physicians’ choices after a diagnosis of intermediate stenosis as revealed by coronary CTA were observed. As a result, Figure 2 shows several real-world strategies for managing the patients with intermediate stenosis. Of all patients, 11% (n = 39) were treated medically without any functional tests or diagnostic CAG. About a half of the rest (46%, n = 153) had noninvasive functional assessments through SPECT or TMT, whereas the other half (43%, n = 143) were referred to undergo CAG directly without a confirmatory functional test. In this case, during angiography, FFR was measured in 23 patients (16% of the patients with direct CAG) to evaluate a functional significance ( Figure 2 ). One-third (33%) of the patients who underwent functional tests showed positive results, whereas 58% showed negative results. The rest of the patients (9%) had indeterminate test results.
Clinical characteristics of the study population are listed in Table 1 . To determine whether the different management strategies after coronary CTA affected clinical outcomes of the patients who had intermediate stenosis, we divided study patients into 2 groups by the presence or absence of additional functional tests ( Figure 3 ). In the so-called 1-step strategy group (n = 159), patients received either medical treatment or anatomical PCI based on the anatomical diagnosis only. In the 2-step strategy group (n = 176), patients had a confirmatory functional test (TMT/SPECT/FFR) with further treatment (i.e., medical treatment or functional PCI), which was planned according to their results. There were no significant differences between those groups both in clinical and laboratory characteristics ( Table 1 ).
| Variable | One-step strategy (n=159) | Two-step strategy (n=176) | Total (n=335) | p value |
|---|---|---|---|---|
| Male | 101 (63.5%) | 116 (65.9%) | 217 (64.8%) | 0.648 |
| Age (years) | 64.4 ± 9.2 | 62.9 ± 9.6 | 63.5 ± 9.4 | 0.136 |
| Diabetes mellitus | 32 (20.1%) | 32 (18.2%) | 64 (19.1%) | 0.873 |
| Hypertension | 103 (64.8%) | 102 (58.0%) | 205 (61.2%) | 0.201 |
| Dyslipidemia | 49 (30.8%) | 50 (28.4%) | 99 (29.6%) | 0.512 |
| Smoker, current | 26 (16.4%) | 30 (17.0%) | 56 (16.7%) | 0.473 |
| Atypical chest pain | 93 (58.5%) | 116 (65.9%) | 209 (62.4%) | 0.154 |
| Body mass index (kg/m 2 ) | 24.9 ± 2.9 | 25.7 ± 2.6 | 25.1 ± 2.8 | 0.108 |
| Hemoglobin (g/dL) | 13.1 ± 1.9 | 12.9 ± 2.0 | 13.0 ± 2.0 | 0.346 |
| Cholesterol (mg/dL) | 171 ± 46 | 168 ± 39 | 170 ± 43 | 0.526 |
| LDL cholesterol (mg/dL) | 98 ± 25 | 93 ± 31 | 95 ± 30 | 0.199 |
| HDL cholesterol (mg/dL) | 41 ± 14 | 43 ± 13 | 42 ± 14 | 0.201 |
| Triglycerides (mg/dL) | 140 ± 72 | 135 ± 80 | 137 ± 77 | 0.564 |
| Fasting blood sugar (mg/dL) | 98 ± 20 | 111 ± 17 | 105 ± 18 | 0.612 |
| Blood urea nitrogen (mg/dL) | 15.2 ± 5.3 | 14.3 ± 3.7 | 14.9 ± 4.2 | 0.123 |
| Creatinine (mg/dL) | 0.99 ± 0.19 | 0.94 ± 0.19 | 0.96 ± 0.20 | 0.116 |
| 10 year risk of CVD (%) | 7.3 ± 1.2 | 6.9 ± 1.1 | 7.1 ± 1.2 | 0.529 |




