The present report compared the incidence of 1-year clinical events in patients with bifurcation lesions that had been treated with a simple approach who were randomized to either a simultaneous final kissing balloon (KB) or an isolated side-branch (SB) balloon post-dilation. From February 2007 to December 2008, 293 patients with all types of Medina bifurcation lesions were enrolled in a prospective study. All patients underwent implantation of a sirolimus- or everolimus-eluting stent across the bifurcation and provisional SB stenting. Patients with no SB ostial compromise or those needing a second stent were excluded from the present study (n = 49). The eligible patients were randomly assigned to treatment with final KB inflation (n = 124, KB group) or isolated balloon after dilation (n = 120, non-KB group). No significant differences were found between the patients from the KB and non-KB groups in terms of age, risk factors, clinical status, or location of the bifurcation lesions. The angiographic data and immediate results were also similar in both groups. Four patients experienced a non–Q-wave acute myocardial infarction in the hospital: three (2%) from the KB group and one (1%) from the non-KB group. Two in-hospital deaths occurred in the non-KB group. Target lesion revascularization was required in 7 patients (3%): 5 from the KB group and 2 from the non-KB group. Late mortality occurred in 3 patients from the KB group and 2 patients from the non-KB group. The incidence of major events at 1 year (death, target lesion revascularization, or acute myocardial infarction) was similar in both groups: 11 (9%) from the KB group and 7 (6%) from the non-KB group (p = NS). In conclusion, no differences in the clinical outcome at 1 year of follow-up were observed between the patients with bifurcation lesions treated with a simple approach and either a simultaneous final KB or an isolated SB balloon post-dilation.
In vitro studies have demonstrated stent deformation when struts have been opened to dilate a side-branch (SB). On the basis of these studies, final kissing inflation has been proposed to correct these deformations and restore the original geometry of the stent in patients with bifurcation lesions that had been treated with a simple approach. However, new bench studies and optimal coherence tomography clinical studies in drug-eluting stents have suggested that kissing balloon (KB) inflation can cause proximal segment elliptical deformation and damage to the polymer coating, increasing the possibility of restenosis and thrombus formation. Furthermore, in patients who had been treated with a simple approach, no in vivo studies have yet demonstrated the usefulness of this maneuver. The purpose of the present report was to compare the incidence of 1-year clinical events in patients with bifurcation lesions that had been treated with a simple approach who were randomized to either a simultaneous final KB or an isolated SB balloon post-dilation.
Methods
From February 2007 to December 2008, 293 patients with all types of Medina bifurcation lesions were enrolled in a prospective study. The patients underwent implantation of a sirolimus- or everolimus-eluting stent across the bifurcation and provisional SB stenting. All patients fulfilled the following inclusion criteria: (1) lesion located in a major bifurcation point, regardless of morphology and angulation; (2) main vessel ≥2.5 mm in diameter; (3) SB ≥2.25 mm in diameter; and (4) SB stenosis length of <10 mm. The exclusion criteria were contraindications to 1-year antiplatelet therapy and cardiogenic shock. The patients who had no SB ostial compromise after main vessel (MV) stent implantation, those needing a second stent at the SB, and those in whom it was impossible to rewire the SB after the MV stent were not considered for the present study (n = 49). The eligible patients (n = 244) were randomly assigned to treatment with either a final KB inflation (n = 124; KB group) or an isolated balloon post-dilation (n = 120; non-KB group). All patients provided written informed consent.
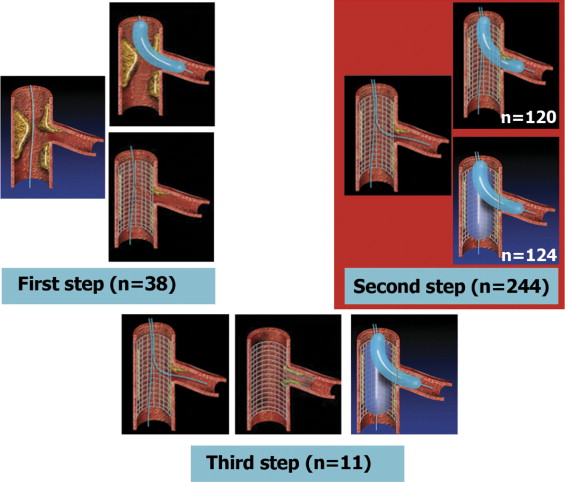
The technique for stent implantation has been previously described, as a stepwise strategy ( Figure 1 ). The MV stent was implanted first. The SB was then rewired, and balloon dilation of the ostium was performed across the metal structure of the stent. The final KB or isolated balloon post-dilation was performed according to the randomization process. Stenting of the SB origin was considered in the presence of residual stenosis >50% or coronary Thrombolysis In Myocardial Infarction flow <3. In the hemodynamic laboratory, patients received a bolus of 100 IU/kg of intravenous unfractionated heparin and continued with low-molecular-weight heparin for the first month. Thienopyridines were maintained for ≥1 year, and aspirin was maintained indefinitely. The baseline bifurcation anatomy was assessed according to the Medina classification. We used the CAAS II, version 4.1.1 (Pie Medical Imaging, Maastricht, The Netherlands) for quantitative coronary angiography, with the dye-filled catheter as a reference. An intravascular ultrasound study (IVUS) was performed at the discretion of the operator. Intrastent ultrasound measurements were obtained in the MV at the edges, at the distal stent segment, immediately under the SB origin, and at the proximal maximal stent diameter. The proximal and distal references were examined at 1 cm from the stent borders. The external elastic lamina area and stent area were obtained at each site. Serial determinations of the troponin I and creatine kinase levels were performed every 6 hours during the first 24 hours after the procedure. Non–Q-wave myocardial infarction was defined as an increase in the creatine kinase level to 3 times the upper limit of the normal range.
The patients were monitored closely by telephone, and additional cardiac catheterization was recommended in the presence of symptoms. Restenosis was defined as ≥50% stenosis during follow-up.
The end point of the study was to assess the incidence of major cardiac events (target lesion revascularization, non–Q-wave acute myocardial infarction, or death) at 1 year of follow-up in each group of patients. In patients with ultrasound results available, a comparison between the IVUS parameters was also performed.
The data are expressed as the mean ± SD. A Student-Fisher pair or unpaired t test was used to compare the mean values from the same patient or from different groups of patients. Differences between the proportions were studied using the chi-square or Fisher exact test, as appropriate. A value of p <0.05 was considered statistically significant.
Results
The baseline clinical and angiographic data are listed in Table 1 . Most of the patients were admitted to the hospital in an unstable clinical condition. No significant differences were found between the groups in terms of age, gender, risk factors, or clinical condition. The 2 groups did not differ significantly with respect to the bifurcation location, vessel size, stenosis severity, or type of bifurcation lesions ( Tables 1 and 2 ). The procedural characteristics are summarized in Table 3 . The lesions in the 2 groups were treated similarly. No significant differences were seen between the groups with regard to technical aspects or the use of platelet glycoprotein IIb/IIIa inhibitors.
| Variable | Group Kissing Balloon (KB) (n=124) | Group Non-KB (n=120) |
|---|---|---|
| Clinical | ||
| Age (years) | 63 ± 10 | 63 ± 12 |
| Men | 94 (76%) | 103 (86%) |
| Smoker | 28 (23%) | 27 (23%) |
| Hypercholesterolemia | 68 (55%) | 58 (48%) |
| Hypertension | 88 (71%) | 76 (63%) |
| Diabetes mellitus | 39 (31%) | 36 (30%) |
| Unstable condition | 110 (89%) | 112 (93%) |
| Previous myocardial infarction | 21 (17%) | 21 (18%) |
| Angiographic | ||
| Ejection fraction (%) | 59 ± 11 | 59 ± 13 |
| Treated bifurcation | ||
| Left anterior descending artery | 70 (56%) | 68 (57%) |
| Right coronary artery | 16 (13%) | 14 (12%) |
| Circumflex | 26 (21%) | 30 (25%) |
| Left main | 12 (7%) | 8 (7%) |
| Main vessel | ||
| Vessel diameter (mm) | 3.1 ± 0.4 | 3.0 ± 0.4 |
| Lesion length | 17 ± 7 | 17 ± 8 |
| Minimal lumen diameter (Pre) | 0.94 ± 0.38 | 0.98 ± 0.38 |
| % Stenosis (Pre) | 70 ± 12 | 68 ± 12 |
| Minimal lumen diameter (Post) | 2.90 ± 0.43 | 2.85 ± 0.39 |
| % Stenosis (Post) | 7 ± 4 | 7 ± 5 |
| Side branch | ||
| Vessel diameter (mm) | 2.44 ± 0.3 | 2.44 ± 0.3 |
| Lesion length | 5.3 ± 2.2 | 5.5 ± 2.5 |
| Minimal lumen diameter (Pre) | 1.3 ± 0.67 | 1.3 ± 0.60 |
| % Stenosis (Pre) | 44 ± 24 | 47 ± 23 |
| Minimal lumen diameter (Post) | 2.13 ± 0.36 | 2.14 ± 0.38 |
| % Stenosis (Post) | 13 ± 8 | 13 ± 10 |
| KB Group (n = 124) | Non-KB Group (n = 120) | |
|---|---|---|
| True bifurcations | 73 (59%) | 71 (59%) |
| 1, 1, 1 | 57 (46%) | 59 (49%) |
| 1, 0, 1 | 2 (2%) | 4 (3%) |
| 0, 1, 1 | 12 (10%) | 6 (5%) |
| 0, 0, 1 | 2 (2%) | 2 (2%) |
| Medina side branch 0 | 51 (41%) | 49 (41%) |
| 1, 1, 0 | 34 (27%) | 29 (24%) |
| 1, 0, 0 | 9 (7%) | 9 (8%) |
| 0, 1, 0 | 8 (6%) | 11 (9%) |
| Variable | KB Group (n = 124) | Non-KB Group (n = 120) |
|---|---|---|
| Main vessel stent diameter (mm) | 3.0 ± 0.5 | 3.0 ± 0.5 |
| Main vessel stent length (mm) | 23 ± 9.3 | 22 ± 8.7 |
| Main vessel stent inflation pressure (atm) | 16 ± 1.4 | 15 ± 1.8 |
| Main vessel stent type | ||
| Sirolimus | 66 (53%) | 57 (48%) |
| Everolimus | 58 (47%) | 63 (52%) |
| Main vessel predilation | 53 (43%) | 49 (41%) |
| Main vessel proximal stent postdilation | — | 37 (31%) |
| Main vessel distal geographic miss | 2 (2%) | 8 (7%) |
| Main vessel intravascular ultrasound study | 53 (43%) | 49 (41%) |
| Side-branch balloon diameter | 2.5 ± 0.3 | 2.5 ± 0.3 |
| Remote site intervention | 73 (59%) | 79 (66%) |
| Incomplete revascularization | 11 (9%) | 11 (9%) |
| Glycoprotein IIb/IIIa inhibitors | 13 (10%) | 13 (11%) |
| Femoral Angio-Seal | 123 (99%) | 119 (99%) |
The in-hospital and 1-month outcomes were as follows. Angiographic success (residual stenosis <30%) was obtained in all the parent vessels. Eleven patients (five from the KB group and six from the non-KB group) had a suboptimal immediate result at the SB and received a second stent at this vessel ( Figure 1 ). These patients were excluded from the present analysis. The mean minimal luminal diameter of the treated segments and the reduction in stenosis immediately after the procedure was similar in the MV and SB in both groups ( Table 1 ). The major cardiac events are listed in Table 4 . Two in-hospital deaths occurred in the non-KB group: 1 patient with multivessel disease and poor left ventricular function died from pulmonary edema, and 1 patient died from sepsis and a cerebrovascular accident. No differences were seen in the markers of myocardial damage after the procedure between the 2 groups ( Table 4 ). With respect to the MV stent type, no differences were present between the sirolimus stent- and everolimus stent-treated patients (1 in-hospital death and 2 non–Q-wave acute myocardial infarction in each group).
| Variable | KB Group (n = 124) | Non-KB Group (n = 120) |
|---|---|---|
| In-hospital and 1-month outcomes | ||
| Non–Q-wave myocardial infarction | 3 (2%) | 1 (1%) |
| Death | 0 | 2 (1.7%) |
| Creatine kinase after procedure (IU/L) | 141 ± 175 | 143 ± 126 |
| Troponin I after procedure (IU/L) | 1.2 ± 2.7 | 1.8 ± 5.1 |
| 12-Month follow-up | ||
| Recurrent infarction | 1 (1%) | 1 (1%) |
| Death (all causes) | 3 (2%) | 2 (2%) |
| Need for target lesion revascularization | 5 (4%) | 2 (2%) |
| Stent thrombosis | 1 (1%) ⁎ | 2 (2%) † |
| Remote site revascularization | 1 (1%) | 4 (3%) |
| Total major events ‡ | 11 (9%) | 7 (6%) |
† One probable and 1 possible stent thrombosis.
‡ Major events included death, acute myocardial infarction, or target lesion revascularization per patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


