Calcified coronary arteries are associated with the development of cardiovascular disease and stroke. It is currently unknown whether coronary artery calcium (CAC) is associated with an increased risk for atrial fibrillation (AF). The aim of this study was to address this question in 6,641 participants (mean age 62 ± 10 years, 53% women, 62% nonwhites) from the Multi-Ethnic Study of Atherosclerosis (MESA) who were free of baseline clinical cardiovascular disease and AF. CAC measurements were assessed by cardiac computed tomography at study baseline. AF was ascertained by review of hospital discharge records and from Medicare claims data until December 31, 2010. Cox regression was used to compute hazard ratios (HRs) and 95% confidence intervals (95% CIs) for the association between CAC and AF. During a median follow-up period of 8.5 years, 308 participants (4.6%) developed AF. In a model adjusted for sociodemographics, cardiovascular risk factors, and potential confounders, higher CAC scores were associated with increased risk for AF (CAC = 0: HR 1.0, referent; CAC = 1 to 100: HR 1.4, 95% CI 1.01 to 2.0; CAC = 101 to 300: HR 1.6, 95% CI 1.1 to 2.4; CAC >300: HR 2.1, 95% CI 1.4 to 2.9). The addition of CAC to the Framingham Heart Study and Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) AF risk scores yielded integrated discrimination improvement of 0.0033 (95% CI 0.0015 to 0.0066) and 0.0028 (95% CI 0.0012 to 0.0057), with relative integrated discrimination improvement of 0.10 (95% CI 0.061 to 0.15) and 0.077 (95% CI 0.040 to 0.11), respectively. In conclusion, CAC is independently associated with increased risk for AF.
Coronary artery calcium (CAC) measured by cardiac computed tomography (CT) provides an estimate of total coronary plaque burden. This technique has been studied largely to identify patients at risk for obstructive coronary artery disease and has been shown to predict future coronary heart disease events. The application of CAC to predict conditions that are not limited to the coronary arteries has recently been explored. In a large population-based cohort study, CAC independently predicted stroke events. Additionally, highly calcified coronary arteries are associated with larger pulmonary veins and left atria, suggesting an association between CAC and atrial fibrillation (AF). However, no studies have examined this potential association. The purpose of this study was to examine the association of CAC with incident AF using data from the Multi-Ethnic Study of Atherosclerosis (MESA).
Methods
Details of MESA have been reported previously. Briefly, from July 2000 to September 2002, a total of 6,814 subjects were recruited at 6 field centers (Baltimore, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles, California; New York, New York; and St. Paul, Minnesota). Participants were required to be 45 to 84 years of age and to have no clinical cardiovascular disease. All participants provided informed consent, and the study protocol was approved by the institutional review board at each participating institution. Our analysis examined the relation between baseline CAC measurements and incident AF. Participants were excluded if they did not undergo baseline measurement of CAC, a baseline diagnosis of AF was present, baseline characteristics were missing, or follow-up data regarding AF follow-up were missing.
Participant characteristics were collected during the initial MESA visit. Age, gender, race and ethnicity, income, and education were self-reported. Annual income was categorized as <$20,000, $20,000 to $49,999, and ≥$50,000, and education was categorized as “high school or less,” “some college,” and “college or more.” Smoking was defined as current or ever smoker. Blood samples were obtained after a 12-hour fast, and measurements of total cholesterol, high-density lipoprotein cholesterol, plasma glucose, and high-sensitivity C-reactive protein were used. Diabetes was defined as a fasting glucose level ≥126 mg/dl or a history of diabetes medication use. Blood pressure was measured for each participant after 5 minutes in the seated position; systolic measurements were recorded 3 separate times, and the mean of the last 2 values was used. Aspirin, statin, antihypertensive, and lipid-lowering medication use were self-reported. Body mass index was computed as the weight in kilograms divided by the square of the height in meters. Left ventricular hypertrophy was defined by the Cornell criteria (R-wave amplitude in lead AV L plus S-wave amplitude in lead V 3 ≥2,800 mm in men and ≥2,000 mm in women) using baseline electrocardiographic data. In a subgroup of MESA participants who had cardiac magnetic resonance imaging data (n = 4,896), left ventricular end-diastolic mass and the left ventricular ejection fraction were recorded. Myocardial horizontal and vertical tagging were performed on 3 left ventricular short-axis slices (base, mid, and apex) by nonselective radiofrequency pulses separated by a spatial modulation of magnetization-encoding gradients. Imaging and analytical methods for this technique have been previously described.
CAC measurements were assessed by cardiac CT using either cardiac-gated electron-beam computed tomographic or multidetector computed tomographic systems, depending on the study site. The CAC score was computed using the phantom-adjusted Agatston score for 2 consecutive scans for each participant, and the mean value was used. During the computed tomographic examinations, the 2 scans were independently analyzed for CAC by 2 analysts. Interobserver agreement between different computed tomographic image analysts who measured CAC on the same cardiac computed tomographic image was excellent (κ = 0.90). Similarly, intraobserver agreement was excellent when the same analyst measured CAC at separate time periods (κ = 0.93).
Follow-up phone calls to study participants every 9 to 12 months were used to identify AF events. Medical records, including discharge diagnoses, were obtained for each hospitalization. Additionally, for participants ≥65 years of age enrolled in fee-for-service Medicare, Medicare claims data were used to identify AF diagnoses in the inpatient setting. Incident AF was defined by International Classification of Diseases, Ninth Revision, codes 427.31 and 427.32.
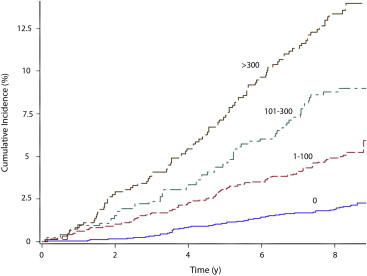
Categorical variables are reported as frequencies and percentages, while continuous variables are reported as mean ± SD. Statistical significance for categorical variables was tested using the chi-square method and Wilcoxon’s rank-sum procedure for continuous variables. Kaplan-Meier estimates were used to compute cumulative incidence of AF by CAC score, and the differences in incidence estimates were compared using the log-rank procedure. Follow-up time was defined as the time between initial visit until the diagnosis of AF or until death, loss to follow-up, or end of follow-up (December 31, 2010). Cox proportional-hazards regression was used to compute hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between CAC scores and AF. CAC was examined using predefined categories (0, 1 to 100, 101 to 300, and >300). Additionally, CAC score was analyzed as a continuous variable using the base-2 logarithm of the CAC score plus 1 (log 2 [CAC + 1]) to examine the risk for AF when the CAC score doubled. Multivariate models were constructed with incremental adjustments as follows: model 1 adjusted for age, gender, race and ethnicity, income, and education; Model 2 adjusted for Model 1 covariates plus smoking status, systolic blood pressure, diabetes, body mass index, total cholesterol, high-density lipoprotein cholesterol, aspirin, antihypertensive and lipid-lowering medications, high-sensitivity C-reactive protein, and left ventricular hypertrophy. The proportional-hazards assumption was not violated in our analysis. We tested for interactions between our main effect variable and age, gender, and race and ethnicity. Additionally, we further adjusted for coronary heart disease events as a time-dependent variable to examine whether incident coronary heart disease events mediated the association between CAC and AF. In participants with cardiac magnetic resonance imaging data, we further adjusted for left ventricular end-diastolic mass and the left ventricular ejection fraction.
We assessed the ability of CAC to predict AF by computing the C-statistic using covariates from the Framingham Heart Study and Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) AF consortium risk models for AF. The added predictive ability of CAC was compared by the difference in C-statistics of the models before and after CAC inclusion. We also investigated the integrated discrimination improvement (IDI) and relative IDI. The IDI quantifies the increase in the difference between mean predicted risks for participants who do and do not develop AF after adding CAC to the model, and this measure also was computed. Additionally, net reclassification improvement, which quantifies any desirable change in predicted risk, was computed for the following risk categories: <2.5%, 2.5% to 5%, and >5%. Statistical significance was defined as p <0.05. SAS version 9.3 (SAS Institute Inc., Cary, North Carolina) was used for all analyses.
Results
Of the 6,814 participants from the original MESA cohort, 58 participants had diagnoses of AF before enrollment in MESA. These patients, detected by Centers for Medicare and Medicaid Services linkage, were excluded, although they did not have AF on baseline electrocardiography. Of those who remained, 6 participants with missing follow-up data and 109 participants missing either baseline characteristics or medication data also were excluded. A total of 6,641 study participants (mean age 62 ± 10; 53% women, 38% whites, 27% blacks, 22% Hispanics, and 12% Chinese-Americans) were included in the final analysis.
Over a median follow-up period of 8.5 years, 308 participants (4.6%) developed AF. Baseline characteristics for study participants stratified by AF are listed in Table 1 . The incidence rate of AF increased with increasing CAC score ( Table 2 ). Unadjusted cumulative incidence curves for AF by CAC score are shown in Figure 1 (log-rank p <0.0001). In an unadjusted Cox regression model, higher CAC scores were associated with an increased risk for AF (CAC = 0: HR 1.0; CAC = 1 to 100: HR 2.5, 95% CI 1.8 to 3.4; CAC = 101 to 300: HR 4.3, 95% CI 3.1 to 6.1; CAC >300: HR 6.9, 95% CI to 5.0 to 9.4). Similarly, doubling of the CAC score was associated with a 23% increased risk for AF (p <0.0001). This pattern of increasing risk for AF associated with increasing CAC scores persisted after adjustment for sociodemographics, cardiovascular risk factors, and potential confounders ( Table 2 ). These results were consistent in subgroup analyses by gender and race and ethnicity ( Table 3 ). A significant interaction was observed for age, with the association being slightly stronger for participants <62 years of age ( Table 3 ). The association between CAC and AF remained significant after further adjustment for coronary heart disease events as a time-dependent variable (log 2 [CAC + 1]; HR 1.1, 95% CI 1.05 to 1.12), left ventricular end-diastolic mass (log 2 [CAC + 1]; HR 1.1, 95% CI 1.05 to 1.14), and the left ventricular ejection fraction (log 2 [CAC + 1]; HR 1.1, 95% CI 1.06 to 1.15).
| Characteristic | AF (n=308) | No AF (n=6,333) | P-value ∗ |
|---|---|---|---|
| Age, mean ± SD (years) | 70 ± 8.0 | 62 ± 10 | <0.0001 |
| Male | 189 (61%) | 2,941 (46%) | <0.0001 |
| White | 168 (55%) | 2,381 (38%) | |
| Black | 66 (21%) | 1,757 (28%) | |
| Chinese-American | 21 (6.8%) | 773 (12%) | |
| Hispanic | 53 (17%) | 1,422 (22%) | <0.0001 |
| Education | |||
| At least high school | 118 (38%) | 2,299 (36%) | |
| Some college | 78 (25%) | 1,814 (29%) | |
| College or more | 112 (36%) | 2,220 (35%) | 0.45 |
| Annual income | |||
| <$20,000 | 99 (32%) | 1,680 (27%) | |
| $20,000-$49,999 | 106 (34%) | 2,219 (35%) | |
| ≥$50,000 | 103 (33%) | 2,434 (38%) | 0.067 |
| Body mass index, mean ± SD (kg/m 2 ) | 29 ± 5.6 | 28 ± 5.5 | 0.19 |
| Current or former smoker | 180 (58%) | 3,107 (49%) | 0.0013 |
| Diabetes | 51 (17%) | 878 (14%) | 0.24 |
| Systolic blood pressure, mean ± SD (mm Hg) | 135 ± 22 | 126 ± 21 | <0.0001 |
| Total cholesterol, mean ± SD (mg/dL) | 190 ± 36 | 194 ± 36 | 0.011 |
| HDL-cholesterol, mean ± SD (mg/dL) | 50 ± 15 | 51 ± 15 | 0.034 |
| Antihypertensive medications | 177 (57%) | 2,262 (36%) | <0.0001 |
| Statins | 52 (17%) | 924 (15%) | 0.27 |
| Aspirin | 120 (39%) | 1,452 (23%) | <0.0001 |
| Lipid-lowering medications | 56 (18%) | 1,007 (16%) | 0.29 |
| hs-CRP, mean ± SD (mg/L) | 3.9 ± 6.0 | 3.7 ± 5.9 | 0.31 |
| Left ventricular hypertrophy | 15 (4.9%) | 241 (3.8%) | 0.34 |
| Coronary artery calcium score | |||
| 0 | 67 (22%) | 3,283 (52%) | |
| <100 | 84 (27%) | 1,660 (26%) | |
| 100-300 | 60 (19%) | 674 (11%) | |
| >300 | 97 (31%) | 716 (11%) | <0.0001 |
| Mean ± SD | 444 ± 807 | 128 ± 377 | <0.0001 |
∗ Statistical significance for continuous data was tested using Wilcoxon rank-sum procedure and categorical data was tested using the Chi-square test.
| CAC Score | Events/No. at risk | Incidence Rate per 1000 Person-Years (95%CI) | Model 1 ∗ HR (95%CI) | P-value | Model 2 † HR (95%CI) | P-value |
|---|---|---|---|---|---|---|
| 0 | 67/3,350 | 2.6 (2.0, 3.2) | 1.0 | – | 1.0 | – |
| 1-100 | 84/1,744 | 6.4 (5.1, 7.9) | 1.5 (1.04, 2.0) | 0.027 | 1.4 (1.01, 2.0) | 0.046 |
| 101-300 | 60/734 | 11 (8.5, 14) | 1.8 (1.2, 2.6) | 0.0017 | 1.6 (1.1, 2.4) | 0.010 |
| >300 | 97/813 | 17 (14, 21) | 2.4 (1.7, 3.3) | <0.0001 | 2.1 (1.4, 2.9) | <0.0001 |
| Log 2 (CAC + 1) ‡ | 308/6,641 | 6.1 (5.4, 6.8) | 1.1 (1.07, 1.14) | <0.0001 | 1.1 (1.05, 1.13) | <0.0001 |
∗ Adjusted for age, sex, race/ethnicity, income, and education.
† Adjusted for Model 1 covariates plus smoking status, systolic blood pressure, diabetes, body mass index, total cholesterol, HDL-cholesterol, aspirin, antihypertensive and lipid-lowering medications, hs-CRP, and left ventricular hypertrophy.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


