6 Contrast Media
Current water-soluble contrast media have as a common structural feature a symmetrically substituted tri-iodinated benzene ring with iodine providing the radiographic contrast. Both ionic and nonionic contrast media are available for coronary angiography.
Ionic contrast media are only sufficiently water soluble as salts. They dissociate in aqueous solutions into an iodine-containing acid (anion) and a contrast-free base (cation). They have high osmolality (Fig. 6.1b). An exception is the low-osmolality ionic contrast medium ioxaglate, which consists of two tri-iodinated benzene rings (a dimer) that are connected via a chain (Fig. 6.1c).
Nonionic contrast media do not carry an electrical charge, are more hydrophilic than ionic contrast media, and possess a significantly lower osmolality (Fig. 6.1a, d). Most nonionic contrast media used in cardiology are nevertheless hypertonic compared with blood (plasma osmolality 290 mosm/kg water) but, due to the physicochemical properties of the nonionic contrast media, they are tolerated substantially better with a relatively low incidence of severe adverse reactions. Hence, nonionic contrast media are now almost exclusively used for coronary angiography.
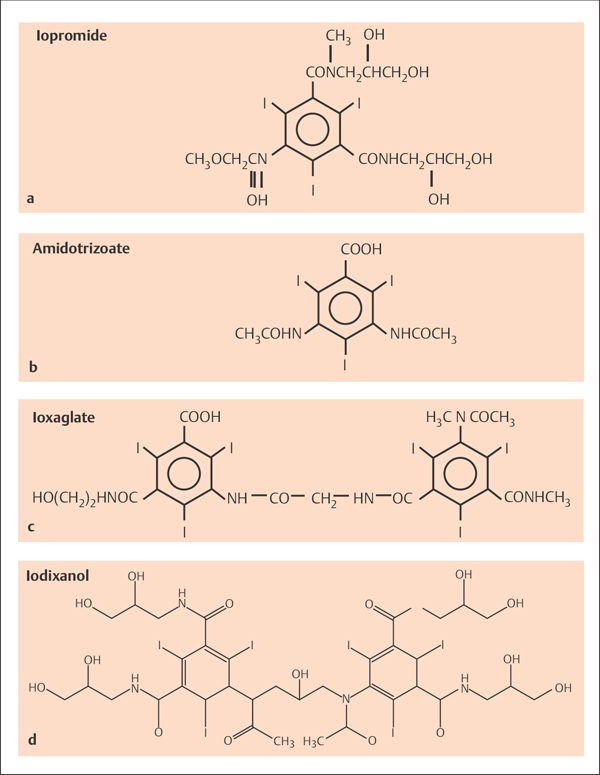
Fig. 6.1 a–d Ionic and nonionic contrast media.
a Iopromide (nonionic).
b Amidotrizoate (ionic).
c Ioxaglate (low osmolality, ionic).
d Iodixanol (nonionic).
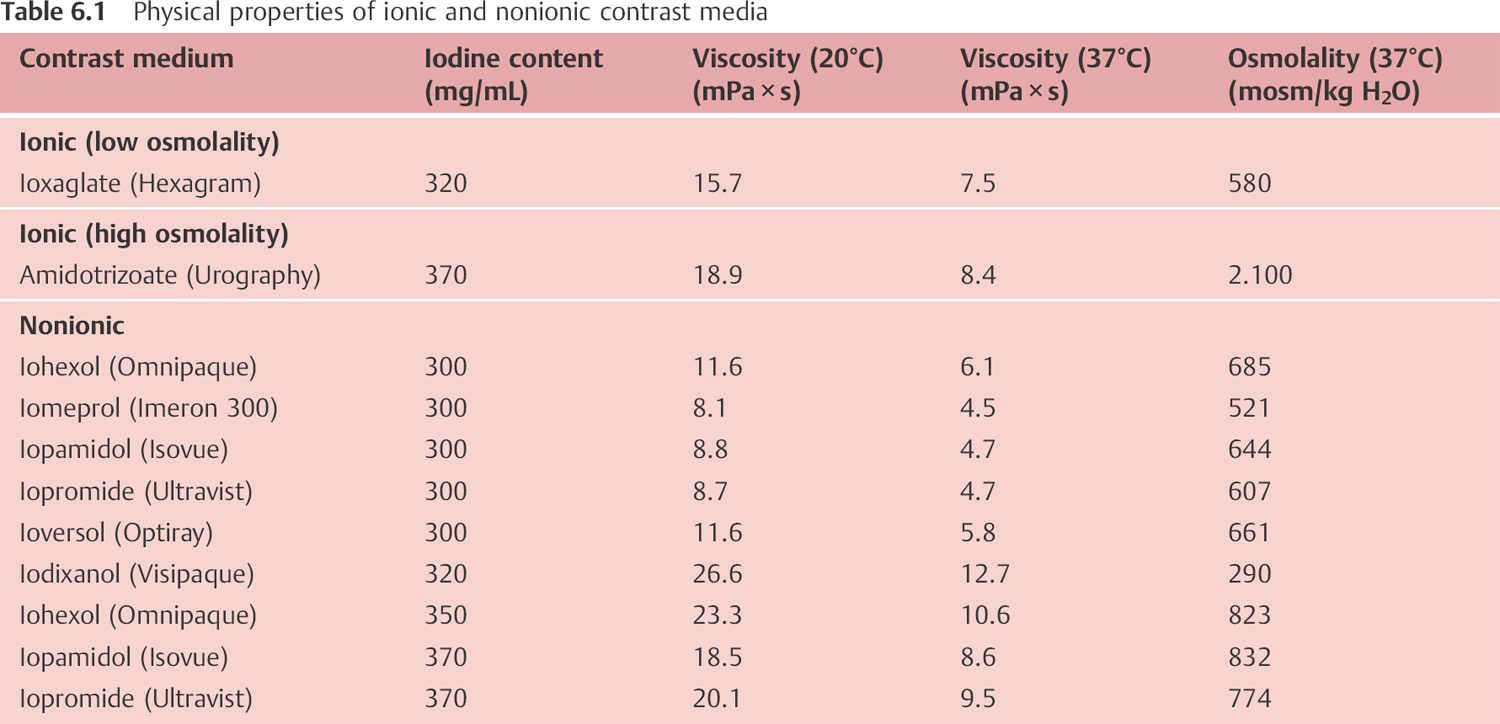
Physical properties of some ionic and nonionic contrast media are listed in Table 6.1.
Adverse Reactions to Contrast Media
Factors that affect the tolerability of a contrast medium include viscosity, osmolality, and iodine content. Important adverse reactions include
 Allergic reactions (flushing, urticaria, bronchospasm, anaphylaxis)
Allergic reactions (flushing, urticaria, bronchospasm, anaphylaxis)
 Electrophysiological effects (ST changes, sinus bradycardia, AV conduction disorders, extrasystoles, and ventricular tachyarrhythmias)
Electrophysiological effects (ST changes, sinus bradycardia, AV conduction disorders, extrasystoles, and ventricular tachyarrhythmias)
 Hemodynamic effects (increase in LVEDP, cardiac depression, peripheral vasodilatation, hypotension)
Hemodynamic effects (increase in LVEDP, cardiac depression, peripheral vasodilatation, hypotension)
 Rheological alterations and thrombotic complications
Rheological alterations and thrombotic complications
 Contrast media–induced acute kidney injury
Contrast media–induced acute kidney injury
With the exception of thrombotic complications, the incidence of adverse reactions is substantially lower with administration of nonionic media than with ionic contrast media. Most adverse reactions are a consequence of the high osmolality of ionic contrast media. Thrombotic complications of the nonionic contrast media are due to their lesser anticoagulatory properties. Experimental studies have shown that contrast media inhibit platelet aggregation in response to thrombin, ADP and epinephrine. These anticoagulatory and platelet-inhibiting properties of contrast media are particularly potent with ionic contrast media, but markedly less so with nonionic contrast media. This requires administration of heparin when nonionic contrast media are given, which in turn essentially cancels any clinical impact of the difference in anticoagulatory properties of the various contrast media.
 Allergic Reactions
Allergic Reactions
Although the use of nonionic contrast media has markedly reduced the incidence of contrast-associated adverse reactions, severe adverse reactions with fatal outcomes after contrast administration can still occur (risk of death with ionic contrast media 1:75,000; with nonionic contrast media 1:500,000). Potential causes of adverse reaction include
 Release of vasoactive mediators (especially histamine)
Release of vasoactive mediators (especially histamine)
 Complement activation
Complement activation
 Alterations in histamine–kallikrein metabolism
Alterations in histamine–kallikrein metabolism
 Direct effects on the central nervous system
Direct effects on the central nervous system
The allergic reaction associated with contrast is frequently designated as an anaphylactoid reaction. It is therefore differentiated from the classic IgE-mediated anaphylaxis, but prophylaxis and therapy of both manifestations are similar.
Symptoms
Symptoms of contrast-related adverse reactions include
 Skin:
Skin:
– Itchiness on hands, feet, and ears
– Urticaria, angioedema
– Flushing
 Respiratory tract:
Respiratory tract:
– Rhinorrhea, sneezing attacks
– Hoarseness, glottis edema
– Bronchospasm
– Apnea
 Gastrointestinal tract:
Gastrointestinal tract:
– Nausea, vomiting
– Cramps
– Fecal incontinence
 Circulatory system:
Circulatory system:
– Tachycardia
– Hypotension/hypertension
– Rhythm disorders
– Shock
– Cardiac arrest
Prophylaxis
Given the very low incidence of adverse reactions with nonionic contrast media, it is not recommended to provide prophylaxis routinely to all patients. This applies also because, compared with intravenous administration, contrast medium–specific adverse reactions after arterial administration are observed relatively rarely and are usually milder.
The need for prophylactic premedication is undisputed in patients with the following risk factors:
 Allergic diathesis (hay fever, drug allergy)
Allergic diathesis (hay fever, drug allergy)
 Prior adverse reaction to contrast
Prior adverse reaction to contrast
 Diseases that are associated with increased histamine levels (lung diseases, food allergy, etc.)
Diseases that are associated with increased histamine levels (lung diseases, food allergy, etc.)
 Age (> 70 years; children)
Age (> 70 years; children)
 Cardiac, respiratory, or hepatic insufficiency
Cardiac, respiratory, or hepatic insufficiency
For these patients premedication is indicated with H1– and H2-receptor antagonists 5 to 10 minutes before contrast medium administration. Recommended dosages are shown in Table 6.2.
For patients with prior severe contrast-related reactions, additional premedication with corticosteroids is recommended.
Prophylaxis is most effective when there is repeated corticosteroid administration 24, 12, and 2 hours before the start of the study (40 mg methylprednisolone orally each time). Bolus administration of corticosteroids (100– 250 mg methylprednisolone) up to 2 hours before the start of the study probably has the same efficacy.
Body weight (kg) | Dimetindene maleate | Cimetidine |
< 60 | 4 mg | 200 mg IV |
60–100 | 8 mg | 400 mg IV |
> 100 | 12 mg |