The prognostic relevance of direct contrast toxicity in patients treated with primary percutaneous coronary intervention remains unclear, owing to the confounding hemodynamic effect of acute left ventricular ejection fraction (LVEF) impairment on kidney function estimation. In the present study, 644 consecutive patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention were prospectively enrolled. Contrast-induced nephropathy (CIN) was defined as an increase in serum creatinine >25% or a decrease in the estimated glomerular filtration rate (eGFR) <25% from baseline in the first 72 hours. The primary end point of the study was major adverse cardiovascular events at 1 year (composite of death, myocardial infarction, target lesion revascularization, and bleeding). Among the global population, the interaction between the LVEF and eGFR at admission to define CIN was statistically significant (p <0.001). When only the 385 patients without acute LVEF impairment (i.e., those with LVEF ≥40%) were considered, 27 (7%) developed postprocedural CIN that was associated with increased major adverse cardiovascular events rate at 1 year of clinical follow-up (38% vs 9%; p <0.001). On adjusted Cox multivariate analysis, CIN was an independent predictor of worse outcomes, both when defined according to creatinine (hazard ratio 3.81, 95% confidence interval 1.71 to 8.48, p = 0.001) or eGFR (hazard ratio 3.77, 95% confidence interval 1.53 to 9.28, p = 0.004) variations. In conclusion, in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention, LVEF has a significant interaction with eGFR. When only patients without acute LVEF impairment were considered, CIN confirmed its negative prognostic effect on the 1-year clinical outcomes.
Contrast-induced nephropathy (CIN), a complication of primary percutaneous intervention in patients with ST-elevation myocardial infarction (STEMI), is a well-established independent predictor of increased in-hospital morbidity and mortality. However, recent data have suggested that an increase in creatinine could be the result of hemodynamic compromise due to an acute impairment of cardiac pump function after extended myocardial infarction, rather than the direct effect of contrast-induced kidney injury. The purpose of the present study was to examine whether in patients with STEMI without an acute systolic function decrease, CIN would maintain its negative prognostic stratification potential.
Methods
From January 2006 to December 2008, 644 consecutive patients with STEMI who were undergoing primary percutaneous coronary intervention (PCI) were consecutively enrolled at the Cardiovascular Center Aalst Onze-Lieve-Vrouwziekenhuis Hospital (Aalst, Belgium) and at the Cardiovascular Department of the University Hospital of Trieste (Trieste, Italy). Patients receiving fibrinolytic treatment were excluded. STEMI was diagnosed in the presence of chest pain suggestive of myocardial ischemia for ≥30 minutes and electrocardiographic changes with new ST-segment elevation in ≥2 contiguous leads of ≥0.2 mV in leads V 2 to V 3 and/or ≥0.1 mV in other leads or new-onset left bundle branch block. Patients receiving chronic peritoneal or hemodialysis treatment were excluded. Because of the institutional policy on the management of STEMI at both centers, a quantitative left ventricular ejection fraction (LVEF) assessment was performed either angiographically during the procedure or echocardio-graphically within 12 hours after the procedure in the coronary care unit.
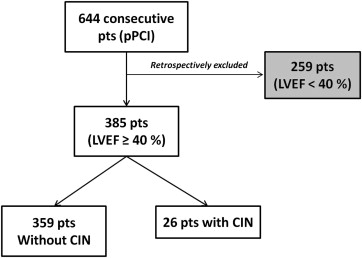
Overall, the patients’ data were analyzed for a potential interaction between the LVEF and renal function. Thereafter, we specifically focused our outcome analysis on patients without acute left ventricular failure (i.e., LVEF ≥40%; Figure 1 ). The local ethics committees approved the study, and all patients provided written informed consent.
After the diagnostic coronary angiogram, a 6F sheath was introduced into the femoral artery, and a 6F guiding catheter was engaged into the coronary ostium. A high-quality angiogram was obtained after intracoronary nitrates to assess the vessel dimensions and flow during the procedure, as previously described. All patients were treated with aspirin (500 mg) and clopidogrel (300 or 600 mg) before the procedure. During PCI, additional weight-adjusted unfractionated heparin was administrated (100 U/kg or 50 U/kg in the case of glycoprotein inhibitor administration). The use of glycoprotein IIb/IIIa receptor inhibitors was left to the discretion of the interventional cardiologist. Mechanical thrombus aspiration was performed, as previously described. Standard therapy after PCI included aspirin, clopidogrel, β blockers, lipid-lowering agents, and angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers. In patients with multivessel disease, only the infarct-related artery was revascularized at enrollment.
Baseline clinical features and laboratory data were collected from the patient database of the participating institutions. CIN was defined as an increase in creatinine >25% from the baseline value or a decrease in the estimated glomerular filtration rate (eGFR) <25% within 72 hours after primary PCI (calculated using the Cockcroft-Gault formula). The serum creatinine concentration was measured at admission (just before primary PCI), each day for the next 3 days, and at hospital discharge. Chronic kidney disease was defined as a baseline serum creatinine of >1.5 mg/dl or an eGFR of 60 ml/min/1.73 m 2 (Levey modified Modification of Diet in Renal Disease formula). Patients with chronic kidney disease were not excluded from the present study, regardless of the degree of chronic kidney disease. Hypertension was defined as previously described. The Thrombolysis in Myocardial Infarction flow grade was evaluated at the beginning (before wiring the lesion) and at the end of the procedure. Post-PCI no-reflow was defined as a Thrombolysis in Myocardial Infarction flow grade <2 not attributable to dissection, occlusive thrombosis, or epicardial spasm. Two independent expert interventional cardiologists, unaware of the treatment strategies adopted during primary PCI (i.e., administration of glycoprotein IIb/IIIa inhibitors and performance of thrombus aspiration) and outcome, reviewed all coronary angiograms to assess the baseline and final Thrombolysis in Myocardial Infarction flow grade. In the case of disagreement, a third operator was involved to reach a consensus. The interobserver coefficient of variation assessed was 7% for the Thrombolysis in Myocardial Infarction flow grade.
Clinical follow-up data were gathered from the hospital records and using telephone interviews. All events were classified and adjudicated by a physician not involved in the follow-up process. The primary end point of our study was major adverse cardiovascular events, defined as the composite of overall death, reinfarction, target vessel revascularization, and major bleeding. Reinfarction was defined as recurrent symptoms with new ST-segment elevation and an increase of cardiac markers to ≥2 times the upper limit of normal. Target vessel revascularization was defined as any clinically driven percutaneous revascularization involving the target lesion or any segment of the epicardial coronary artery containing the target lesion. Major bleeding was defined according to the Thrombolysis In Myocardial Infarction bleeding classification as intracranial bleeding or a 5-g/dl decrease in the hemoglobin concentration or a 15% absolute decrease in the hematocrit. An echocardiographic evaluation was performed in all patients within 12 hours after hospital admission.
Continuous variables are expressed as the mean ± SD or median and interquartile range. Categorical variables are reported as frequencies and percentages. Variables with a normal distribution were assessed using the Kolmogorov-Smirnov test. Student’s t test or the Mann-Whitney U test was used to compare continuous variables, as appropriate. Comparisons between categorical variables were evaluated using 2-tailed Fisher’s exact test or Pearson’s chi-square test, as appropriate. In the global population of 644 patients, binary logistic regression analysis was performed with respect to the end point CIN. An interaction term was constructed, using the centered values of 2 continuous variables, LVEF and eGFR, and adjusted linear regression analysis was performed to assess statistical significance.
Considering the 385 patients without LVEF impairment, the survival curve was constructed using the Kaplan-Meier method. Cox analysis was performed twice, in a stepwise manner, and using a different definition of CIN (i.e., creatinine or eGFR postprocedural modification), adjusted for all variables listed in Tables 1 and 2 with p <0.05 on univariate analysis. The results are expressed as hazard ratios (HRs) and 95% confidence intervals (CIs). All p values were 2-tailed. Analyses were done with SPSS software, version 17.0 (SPSS, Chicago, Illinois).
| Variable | Global Population (n = 644) | Patients With LVEF ≥40% (n = 385) | p Value † | ||
|---|---|---|---|---|---|
| No CIN (n = 358) | CIN (n = 27) | p Value ∗ | |||
| Age (yrs) | 65 ± 12 | 64 ± 12 | 69 ± 14 | 0.055 | 0.644 |
| Men | 483 (75%) | 272 (76%) | 21 (78%) | 0.801 | 0.923 |
| Hypertension | 373 (58%) | 215 (60%) | 17 (62%) | 0.851 | 0.247 |
| Diabetes mellitus | 135 (21%) | 64 (18%) | 6 (23%) | 0.516 | 0.982 |
| Hypercholesterolemia ‡ | 412 (64%) | 226 (63%) | 18 (65%) | 0.817 | 0.899 |
| Active smoker | 264 (41%) | 147 (41%) | 7 (27%) | 0.209 | 0.153 |
| Chronic kidney disease | 142 (22%) | 68 (19%) | 12 (44%) | 0.005 | 0.222 |
| Contrast (ml) | 227 ± 80 | 223 ± 79 | 242 ± 81 | 0.308 | 0.776 |
| Previous myocardial infarction | 90 (14%) | 47 (13%) | 5 (19%) | 0.388 | 0.323 |
| Previous percutaneous coronary intervention | 77 (12%) | 43 (12%) | 5 (19%) | 0.355 | 0.456 |
| Previous coronary artery bypass grafting | 19 (3%) | 14 (4%) | 0 (0%) | 0.351 | 0.397 |
∗ Comparison between no-CIN and CIN groups without acute LVEF impairment.
† Comparison between patients without acute LVEF impairment and global patient population.
| Variable | Global Population (n = 644) | Patients With LVEF >40% (n = 385) | p Value † | ||
|---|---|---|---|---|---|
| No CIN (n = 358) | CIN (n = 27) | p Value ∗ | |||
| Stenotic coronary arteries | 1.7 ± 0.8 | 1.7 ± 0.9 | 1.9 ± 0.9 | 0.322 | 0.655 |
| Culprit coronary vessel | |||||
| Left anterior descending artery | 335 (52%) | 179 (50%) | 17 (63%) | 0.332 | 0.738 |
| Left coronary artery | 193 (30%) | 111 (31%) | 7 (26%) | 0.866 | 0.553 |
| Right | 109 (17%) | 64 (18%) | 2 (7%) | 0.874 | 0.938 |
| Saphenous vein graft | 7 (1%) | 4 (1%) | 1 (4%) | 0.984 | 0.383 |
| Left ventricular ejection fraction (%) | 52 ± 14 | 56 ± 10 | 52 ± 10 | 0.496 | 0.394 |
| Systolic blood pressure (mm Hg) | 129 ± 26 | 132 ± 25 | 128 ± 29 | 0.320 | 0.499 |
| Diastolic blood pressure (mm Hg) | 75 ± 15 | 76 ± 15 | 75 ± 19 | 0.184 | 0.364 |
| Stent implantation | 593 (92%) | 329 (92%) | 22 (82%) | 0.065 | 0.476 |
| Direct stenting | 271 (42%) | 168 (47%) | 14 (52%) | 0.820 | 0.378 |
| Drug-eluting stents | 116 (18%) | 72 (20%) | 4 (15%) | 0.863 | 0.239 |
| Intra-aortic balloon pump | 58 (9%) | 32 (9%) | 3 (11%) | 0.655 | 0.949 |
| Thrombolysis In Myocardial Infarction flow grade | |||||
| 0-1 at baseline | 553 (86%) | 301 (84%) | 24 (87%) | 0.877 | 0.493 |
| 3 at end of procedure | 528 (82%) | 297 (83%) | 20 (74%) | 0.252 | 0.349 |
| No reflow | 39 (6%) | 18 (5%) | 3 (11%) | 0.166 | 0.985 |
| Thrombus aspiration | 386 (60%) | 226 (63%) | 15 (56%) | 0.534 | 0.479 |
| Glycoprotein IIb/IIIa inhibitors | 374 (58%) | 211 (59%) | 14 (52%) | 0.464 | 0.343 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


