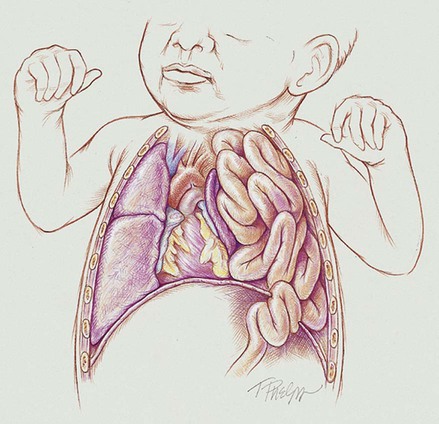
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with congenital diaphragmatic hernia. • Describe the causes of congenital diaphragmatic hernia. • List the cardiopulmonary clinical manifestations associated with congenital diaphragmatic hernia. • Describe the general management of congenital diaphragmatic hernia. • Describe the clinical strategies and rationales of the SOAP presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. During normal fetal development, the diaphragm first appears anteriorly between the heart and liver and then progressively grows posteriorly. Between the eighth and tenth week of gestation, the diaphragm normally completely closes at the left Bochdalek foramen, which is located posteriorly and laterally on the left diaphragm. At about the tenth week of gestation (close to the same time the Bochdalek foramen is closing), the intestines and stomach normally migrate from the yolk sac. If, however, the bowels reach this area before the Bochdalek foramen closes, a hernia results—a congenital diaphragmatic hernia (CDH) (also called a Bochdalek hernia or posterior-lateral diaphragmatic hernia). In other words, a Bochdalek hernia is an abnormal hole in the posterolateral corner of the left diaphragm that allows the intestines—and in some cases the stomach—to move directly into the chest cavity and compress the developing lungs.* As shown in Figure 38-1, the effects of a diaphragmatic hernia are similar to the effects of a pneumothorax or hemothorax—the lungs are compressed. As the condition becomes more severe, atelectasis and complete lung collapse may occur. When this happens, the heart and mediastinum are pushed to the right side of the chest—called dextrocardia. In addition, long-term lung compression in utero causes pulmonary hypoplasia, which is most severe on the affected (ipsilateral) side but also occurs on the unaffected (contralateral) side. Finally, as a consequence of the hypoxemia associated with a diaphragmatic hernia, these babies often develop hypoxia-induced pulmonary arterial vasoconstriction and vasospasm, which produces a state of pulmonary hypertension. As a general rule, however, these babies only have a transient state of pulmonary hypertension until the diaphragmatic hernia is repaired. This is different from persistent pulmonary hypertension of the newborn (PPHN) (see Chapter 31).
Congenital Diaphragmatic Hernia
Anatomic Alterations of the Lungs



