Complication
Operative
Nonoperative
Overall rate (%)
Range (%)
Overall rate (%)
Range (%)
Wound complications
3.10
(0–20)
N/A
N/A
Empyema
0.12
(0–5)
0.45
(0–20)
Pleural effusion
0.12
(0–2)
0
(0)
Nonunion
0.84
(0–15)
0.22
(0–4.5)
Chest wall numbness
0.6
(0–16)
0
(0)
Hardware pain
1.91
(0–33)
N/A
N/A
Hardware removal
1.91
(0–33)
N/A
N/A
Loose hardware
0.95
(0–20)
N/A
N/A
Chest wall rigidity
2.39
(0–60)
3.58
(0–84)
Tracheostomy
5.37
(0–20)
10.51
(0–79)
Sepsis
0.48
(0–4)
4.47
(0–50)
Death
7.16
(0–23)
20.58
(0–46)
Pneumonia
8.00
(0–42)
28.86
(0–90)
Chest wall deformity
0.84
(0–12)
8.50
(0–64)
Atelectasis
1.91
(0–21)
0.22
(0–3)
Chest wall pain
2.98
(0–39)
3.80
(0–89)
Retained hemothorax
0.12
(0–0.5)
0
(0)
Cumulative complication rate
38.8
80.52
While recognizing these limitations, several important observations can be made. First, consistent with previous systematic reviews, we found that the surgical stabilization of flail chest injuries led to significantly reduced rates of general complications including pneumonia (8.0 % operative vs. 28.86 % nonoperative), sepsis (0.48 % operative vs. 4.47 % nonoperative), tracheostomy (5.37 % operative vs. 10.51 % nonoperative), and death (7.16 % operative vs. 20.58 % nonoperative). Second, the rates of local complications such as empyema (0.12 % operative vs. 0.45 % nonoperative), retained hemothorax (0.12 % operative vs. 0 % nonoperative), and recurrent pneumothorax (none reported) are relatively low and generally compare favorably to the rates seen with nonoperative management. Finally, the rates of surgery-specific complications such as surgical wound infections (3.10 %), hardware failur e (0.95 %), and symptomatic hardware requiring removal (1.91 %) appear to be relatively low. In addition, the cumulative complication rate was 38.78 % in the surgical group vs. 81.21 % in the nonoperative group. Once again, it is important to view these rates in the context of what has likely been a substantial underreporting of surgical complications in the previous literature.
Specific Surgical Complications and Their Treatment
Infection
Infection can occur in the lung parenchyma (pneumonia), in the pleural space (empyema), superficially in the surgical wound, or systemically (sepsis). In the setting of operative intervention, any infection of the surgical site or pleural space is complicated by the presence of surgical implants, which are typically metallic and prone to biofilm formation. Rates of pneumonia following surgical stabilization of flail chest injuries range from 0 to 42 % with an average rate of 8.0 %. While this may appear to be an elevated rate, it must be remembered that this is a high-risk patient group: these rates are significantly lower than the rates observed in patients with similar injuries treated nonsurgically, which may be due to decreased time spent on mechanical ventilation in the surgical group. Pneumonia in the setting of surgical stabilization is reliably treated with targeted antibiotic therapy and appropriate pulmonary toilet practices. There have been no reports in the literature of the need for secondary surgery in the setting of pneumonia following surgical stabilization of flail chest injuries.
Rates of pleural empyema in the literature have varied widely, with rates 0–20 % reported. The overall rate in our systematic review was 0.12 % with surgical management versus 0.45 % with nonoperative management. These rates seem low, given the fact that previous literature had documented an empyema rate of 3 % among all patients with blunt chest trauma [7]. Diagnosis is generally based on physical exam findings, culture of chest tube drainage, routine blood work (white blood cell count, c-reactive protein, and erythrocyte sedimentation rate), and radiographic imaging including a chest radiograph and contrast computed tomography (CT) of the chest to assess for pleural collections. Given the presence of hardware (typically plates and screws) traversing both the deep wound and the pleural space, distinguishing between a deep wound infection and empyema can often be difficult. Rates of wound infection following surgical stabilization of flail chest injuries range from 0 to 20 %. Mayberry et al. reported two deep infections in their cohort of 46 patients (4.3 %) treated with a combination of implants for rib fracture fixation [8]. Both cases of infection required secondary surgery for drainage of infection.
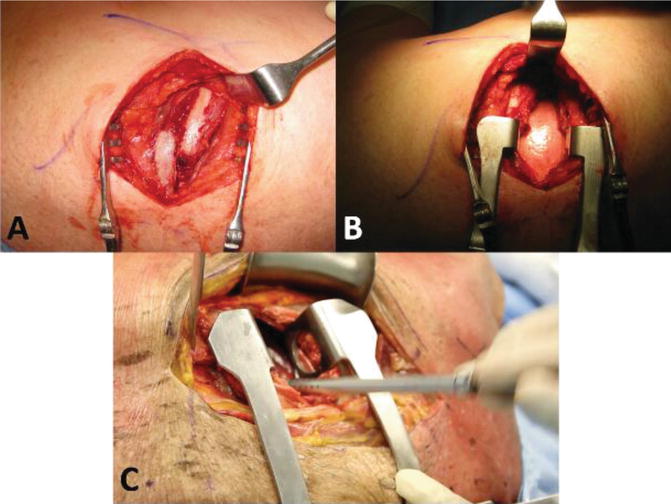
Superficial wound infections can generally be treated with antibiotics alone and close surveillance. However, the treatment of both deep wound infections and pleural empyemas requires surgical intervention given the presence of hardware. There are no published guidelines on the management of empyema or deep wound infections in the setting of rib fixation. However, treatment recommendations can be extrapolated from the existing orthopedic literature on implant-related infections [9]. Acute infections (less than 6 weeks post-rib fixation) can be managed with irrigation and debridement, retention of stable hardware, and culture-specific intravenous antibiotics. Chronic infections (greater than 6 weeks post-rib fixation) require a similar approach as outlined above plus removal of hardware and necrotic/infected bone. In both the acute and chronic setting, any suggestion of infection of the pleural space requires additional irrigation and debridement of the pleural space +/− decortication, by either a formal thoracotomy or video-assisted thoracoscopic surgery (VATS) (see Fig. 12.1) [7].
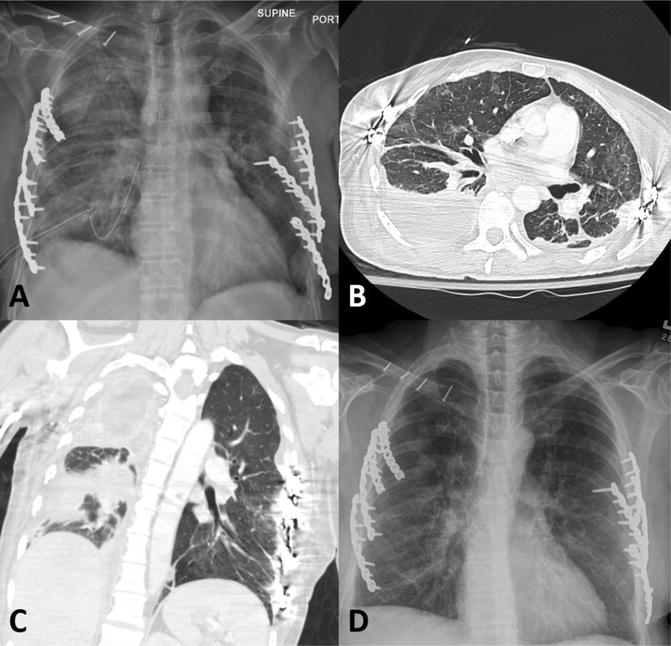
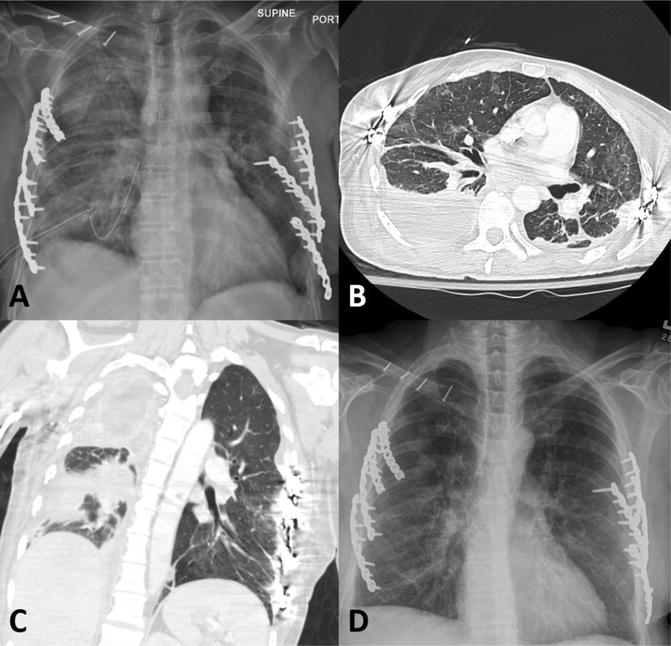
Fig. 12.1
A 50-year-old female patient was treated with bilateral rib fixation for bilateral flail chest injuries. (a, b, and c) AP chest radiograph and axial and coronal CT slices on postoperative day 21 showing complex fluid collection in right lung cavity. The patient was febrile, with purulent drainage from her chest tube. (d) AP chest radiograph 1 week post-thoracotomy and decortication of the right lung and antibiotic treatment demonstrating resolution of the patient’s empyema
There are several steps that can be taken to reduce the risk of deep infection and pleural empyema in the setting of rib fracture fixation for flail chest injuries. First, chest tubes that have been placed prior to surgery should be removed, as these tubes are frequently placed under semi-sterile conditions and have often been in place for several days prior to surgery. The authors generally perform our sterile preparation of the surgical field with the old chest tube in situ and then remove the tube once we have dissected down to the fractured ribs (this is done to reduce the risk of developing a tension pneumothorax during induction of anesthesia). Second, we position our new chest tube through an incision caudal to the surgical incision with tunneling of the chest tube in the subcutaneous tissues in order to maximize the distance between the chest tube incision and rib fixation hardware (see Fig. 12.2). Finally, we are aggressive in treating retained hemothoraces in patients who have undergone rib fracture fixation (see following section).


Fig. 12.2
Intraoperative photograph demonstrating positioning of the chest tube (red arrow) caudal to the surgical incision following rib fracture fixation for a flail chest injury
Retained Hemothorax
A retained hemothorax is defined as a radiographically apparent hemothorax 72 h after appropriate chest tube placement. There has only been a single case of retained hemothorax reported in the literature following rib fixation surgery (rate of 0.12 %). This is surprising, since previous trauma literature has suggested an 18–20 % rate of retained hemothorax in all patients who require chest tube placement for traumatic hemothoraces [10, 11]. It is possible that performing rib fracture fixation allows the surgeon the opportunity to surgically evacuate any hemothorax through the chest wall defect typically seen at the fracture site (Fig. 12.3), decreasing the risk of this complication. However, it is also possible that this complication is substantially underreported in the current literature on surgical fixation for flail chest injuries. The authors of this chapter routinely perform evacuation of any retained hemothorax at the time of rib fracture fixation (Fig. 12.3). In addition, we always place a large-bore (32–36 F) chest tube at the conclusion of the procedure in order to mitigate the risk of retained hemothorax or persistent pneumothorax.