Echocardiography now plays a central guiding role in the management of patients with atrial fibrillation (AF). However, the current guidelines mention little about the presence AF during the assessment of echocardiographic variables in the clinical setting. AF itself may impact on tricuspid annular plane systolic excursion (TAPSE) as a right ventricular systolic function compared with sinus rhythm (SR). The aim of this study was to compare and assess the echocardiographic parameters including TAPSE in patients with AF and SR. From January 1, 2013, to September 30, 2014, patients with AF without any cardiovascular disease were retrospectively evaluated using echocardiography. Age-, gender-, and left ventricular ejection fraction–matched patients with SR were selected from our database on the basis of a comprehensive history, physical examination, and echocardiographic findings. During the study period, we identified 239 patients with AF (74 ± 9 years; 65% men) and without any cardiac disease who underwent echocardiography. We also included 281 patients in the SR group (74 ± 8 years; 67% men). In all study subjects, TAPSE in AF was smaller than in SR regardless of age (17 ± 3 vs 20 ± 3 mm, p <0.001). In the stepwise multiple regression model, TAPSE was strongly associated with the presence of AF (standardized β = −0.362, p <0.001) and stroke volume index (standardized β = 0.173, p <0.001) after adjustment for age, gender, heart rate, left ventricular ejection fraction, and tricuspid regurgitant grade. In conclusions, patients with AF had lower TAPSE than those with SR regardless of age. When we assess TAPSE in the clinical setting, we must pay attention to the presence of AF.
Recently, there has been increased recognition of the importance of information provided by right ventricular (RV) function in several heart diseases. In the clinical setting, tricuspid annular plane systolic excursion (TAPSE) is an easily obtainable, simple, and feasible measure of RV function that we use routinely, and TAPSE is also correlated with RV ejection fraction, which was a gold standard of RV function. Some investigators reported that deterioration of RV function was closely related with new onset of atrial fibrillation (AF) in patients with acute heart failure. In addition, one previous study revealed that reduced RV function returned to normal 1 month after cardioversion to sinus rhythm (SR). We suspected that AF itself may impact on TAPSE as a surrogate of RV function. The aim of this study was to compare and assess the echocardiographic parameters including TAPSE in patients with AF and SR.
Methods
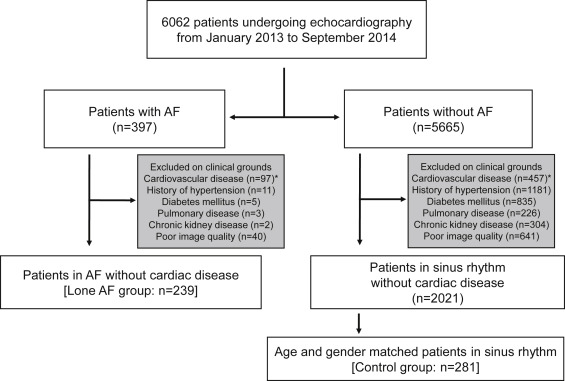
We designed a retrospective study to assess the echocardiographic parameters in 6,062 patients with SR and chronic AF referred to our echocardiographic examination center from January 1, 2013, to September 30, 2014. The exclusion criteria were as follows: patients with a history of hypertension, diabetes mellitus, pulmonary disease, chronic kidney disease, and cardiovascular disease. We defined each cardiovascular disease was as follows: cardiac arrhythmia except for AF, myocardial infarction based on electrocardiography/stress testing/coronary angiography/coronary computed tomography, cardiomyopathy, congenital heart disease, and more than mild valvular disease. Subjects were also excluded if they had poor echocardiographic images. From the patients in SR without cardiac disease, we matched each patient, using the following matching criteria: age (range 5 years), gender, and left ventricular ejection fraction (LVEF; range 5%). After the exclusions and matching, 281 patients with SR and 239 chronic patients with AF were included for final analysis ( Figure 1 ). The Institutional Review Board of the Tokushima University Hospital approved the study protocol.
Transthoracic echocardiography was performed by experienced sonographers/doctors using a commercially available ultrasound machine (iE33; Philips Healthcare, Amsterdam, The Netherlands; Vivid E9; GE Healthcare, Chalfont St. Giles, United Kingdom; and SSA-770A; Toshiba Medical, Tokyo, Japan). Measurements and recordings were obtained according to the American Society of Echocardiography recommendations. LV end-diastolic volume (LVEDV), LV end-systolic volume, maximum left atrial volume (LAV), and LVEF were calculated by the biplane Simpson disk method using 2-dimensional images in 2 apical view (4-chamber and 2-chamber) and indexed to body surface area (BSA; LVEDV index, LV end-systolic volume index, and LAV index [LAVi], respectively). Stroke volume was calculated as the product of the cross-sectional area of the LV outflow tract and the time velocity integral in the LV outflow tract and indexed to BSA (stroke volume index). The systolic annular tissue velocities were also measured in the apical 4-chamber view with the sample volume positioned at lateral mitral annulus (mitral annular motion systolic velocity) and lateral tricuspid annulus (right ventricular systolic velocity [RV S’]). TAPSE was measured as the distance of systolic movement of the junction between the tricuspid valve and the RV free wall using M-mode in accordance with current guidelines. Systolic pulmonary artery pressure was estimated from the systolic transtricuspid pressure gradient (PG) calculated by the modified Bernoulli’s equation using maximal continuous-wave Doppler velocity of the tricuspid regurgitant (TR) jet. Right atrial pressure was estimated from the inferior vena cava diameter and collapsibility ( Figure 2 ). The severity of TR was characterized by vena contracta (VC) as mild (grade 1, VC is not defined); moderate (grade 2, VC <7 mm); and severe (grade 3, VC ≥7 mm) according to the guideline. All measurements of heart structure and performance were averaged over 3 cardiac cycles in SR. In AF rhythm, an index beat, which was the beat after the nearly equal preceding and prepreceding intervals, was used for each measurement. Index-beat determination of ventricular systolic function was accurate in several studies (index-beat vs multibeats measurement, Pearson’s correlation r = 0.94 to 0.96, p <0.001). In our cohort, we have performed the comparison between the index-beat and multibeats measurement (average of 5 beats) TAPSE, in 30 selected patients. The correlation between 2 measurements is strong ( r = 0.97, p <0.001), and Bland–Altman analysis showed a mean difference of −0.3 mm with limit of agreement of ±1.5 mm.

Data are presented as mean ± SD. The Student t test was used to compare continuous variables, and the chi-square test was applied to compare categorical variables. Linear regression analysis was used to evaluate the associations between several potential variables and TAPSE. Identified variables (p <0.20 in the univariate model) were considered to enter in a stepwise manner into a multivariate linear regression model. Age, gender, LVEF, TR severity, and heart rate (HR) were forced into the final model regardless of a stepwise manner because we suspected to influence TAPSE. RV S’ was excluded in the final model because of strong collinearity of TAPSE. To assess the differences in changes of TAPSE between the age groups, we applied a linear mixed-effects model with unstructured covariance for random effects using standard statistical software (SPSS software 21.0; SPSS Inc., Chicago, Illinois). Subjects were divided into the following age groups: 50 to 59 years, 60 to 69 years, 70 to 79 years, and ≥80 years. We used TAPSE and the presence of AF as factors, categorical age groups as a covariate, as well as their first degree interactions (age × AF of TAPSE), with significance of corresponding parameter estimates reported in the results. Reproducibility was expressed as the mean percentage error (absolute difference divided by the average of the 2 observations). Measurement was performed in AF group of 20 randomly selected subjects by 1 observer and then repeated on 2 separate days by 2 observers who were unaware of the measurements of the others and of the study time point. The intraobserver and interobserver variability of the TAPSE were 6.4 ± 4.2% and 7.1 ± 5.1%. Statistical significance was defined by p <0.05.
Results
Baseline characteristics and echocardiographic variables of the study groups are presented in Table 1 . No significant differences were observed with regard to age, gender, and BSA between the SR group and the AF group. The AF group had a higher HR (72 ± 15 vs 65 ± 12 beats/min, p <0.001) and had larger LAVi (39 ± 18 vs 25 ± 7 ml/m 2 , p <0.001) compared with SR group. RV systolic parameters (TAPSE and RV S′) were smaller (17 ± 3 vs 20 ± 3 mm, p <0.001 and 10 ± 2 vs 12 ± 2 cm/sec, p <0.001), and TR grade and TR-PG were larger in AF group than in SR group (1.3 ± 1.1 vs 0.4 ± 0.7, p <0.001 and 25 ± 8 vs 21 ± 6 mm Hg, p <0.001).
| Variable | SR group (n=281) | AF group (n=239) | p value |
|---|---|---|---|
| Age (years) | 74±8 | 74±9 | 0.69 |
| Men | 188 (67%) | 155 (65%) | 0.62 |
| Body surface area (m 2 ) | 1.6±0.2 | 1.6±0.2 | 0.21 |
| Heart rate (bpm) | 65±12 | 72±15 | <0.001 |
| Systolic Blood pressure (mmHg) | 128±11 | 126±10 | 0.14 |
| Diastolic Blood pressure (mmHg) | 71±13 | 72±14 | 0.13 |
| Left ventricular parameters | |||
| Left ventricular end-diastolic volume index (ml/m 2 ) | 56±16 | 51±15 | <0.001 |
| Left ventricular end-systolic volume index (ml/m 2 ) | 22±8 | 19±7 | <0.001 |
| Left ventricular ejection fraction (%) | 61±5 | 62±6 | 0.24 |
| Stroke volume index (ml/m 2 ) | 34±8 | 31±9 | 0.001 |
| Systolic lateral mitral annular motion velocity (cm/s) | 7.5±2.3 | 6.7±2.4 | <0.001 |
| Left ventricular mass index (g/m 2 ) | 81±17 | 80±22 | 0.56 |
| Left atrial volume index (ml/m 2 ) | 25±7 | 39±18 | <0.001 |
| Right ventricular parameters | |||
| Tricuspid annular plane systolic excursion (mm) | 20±3 | 17±3 | <0.001 |
| Systolic lateral tricuspid annular motion velocity (cm/s) | 12±3 | 10±2 | <0.001 |
| Tricuspid regurgitant grade | 0.1±0.3 | 0.7±0.8 | <0.001 |
| Tricuspid regurgitant pressure gradient (mmHg) | 21±6 | 25±8 | <0.001 |
| Inferior vena cava (mm) | 11±3 | 14±4 | <0.001 |
To determine the factors of decreased TAPSE, we performed univariate and multivariate analysis of association of clinical and echocardiographic variables with TAPSE. In the univariate model, TAPSE was correlated with the presence of AF, RV S’ and several echocardiographic parameters ( Table 2 ). In the stepwise multiple regression model, TAPSE was correlated with the presence of AF (standardized β = −0.362, p <0.001), stroke volume index (standardized β = 0.173, p <0.001) after adjustment for age, gender, HR, LVEF, and TR grade ( Table 2 ).
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| ß Unstandardised (SE) | ß Standardised | p value | ß Unstandardised (SE) | ß Standardised | p value | |
| Presence of AF | -2.711 (0.295) | -0.379 | <0.001 | -2.577 (0.324) | -0.362 | <0.001 |
| Age | -0.045 (0.018) | -0.108 | 0.015 | -0.032 (0.018) | -0.078 | 0.077 |
| Men | 1.080 (0.332) | 0.143 | 0.001 | 0.617 (0.334) | 0.082 | 0.066 |
| Body surface area | 2.231 (0.768) | 0.129 | 0.004 | |||
| Heart rate | -0.045 (0.012) | -0.171 | <0.001 | -0.015 (0.011) | -0.058 | 0.176 |
| Systolic Blood pressure | 0.014 (0.007) | 0.081 | 0.071 | |||
| Diastolic Blood pressure | -0.027 (0.012) | -0.101 | 0.024 | |||
| Echocardiographic parameters | ||||||
| Left ventricular end-diastolic volume index | 0.045 (0.010) | 0.194 | <0.001 | |||
| Left ventricular end-systolic volume index | 0.064 (0.021) | 0.134 | 0.003 | |||
| Left ventricular ejection fraction | 0.051 (0.032) | 0.071 | 0.11 | 0.087 (0.030) | 0.121 | 0.004 |
| Stroke volume index | 0.089 (0.017) | 0.223 | <0.001 | 0.040 (0.010) | 0.173 | <0.001 |
| Systolic lateral mitral annular motion velocity | 0.166 (0.068) | 0.109 | 0.016 | |||
| Left ventricular mass index | -0.006 (0.007) | -0.037 | 0.411 | |||
| Left atrial volume index | -0.061 (0.01) | -0.254 | <0.001 | |||
| Systolic lateral tricuspid annular motion velocity | 0.617 (0.053) | 0.463 | <0.001 | |||
| Tricuspid regurgitant grade | -0.941 (0.251) | -0.165 | <0.001 | -0.855 (0.364) | -0.116 | 0.010 |
| Tricuspid regurgitant pressure gradient | -0.019 (0.024) | -0.037 | 0.422 | |||
| Inferior vena cava | -0.041 (0.038) | -0.047 | 0.293 | |||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


