We compared the outcomes of a novel, thin-strut, cobalt-chromium, absorbable, polymer sirolimus-eluting stent (APSES; MiStent) to the durable polymer cobalt-chromium everolimus-eluting stent (EES; Xience). A propensity-matched analysis was performed comparing data from the DES With Sirolimus and a Bioabsorbable Polymer for the Treatment of Patients With De Novo Lesions in the Native Coronary Arteries (DESSOLVE) I and II studies, evaluating the APSES to the EES arm of the Intracoronary Stenting and Angiographic Results: Test Efficacy of 3 Limus-Eluting Stents-4 study. Target lesion failure (TLF) and its components were evaluated at 12 months and annually to 3 years; 805 patients (APSES = 153; EES = 652) were included with propensity matching in 204 patients (APSES = 102; EES = 102). APSES compared with EES had lower TLF at 1 year (3.0% vs 8.0%, p = 0.12) driven by a difference in target lesion revascularization (TLR; 1% vs 6%, p = 0.05), with no difference in target vessel myocardial infarction (p = 0.56) or stent thrombosis (p = 0.31). At 3 years, TLF (5.0% vs 12.5%, p = 0.07) and TLR (2.0% vs 8.4%, p = 0.04) remained lower with APSES. By landmark analysis, there was no significant difference in TLF between 1 and 3 years (p = 0.36). In conclusion, in a propensity-matched analysis, the APSES demonstrated reduced clinically indicated TLR rates at 1 and 3 years compared with the durable polymer EES, with minimal accrual of events between 1 and 3 years.
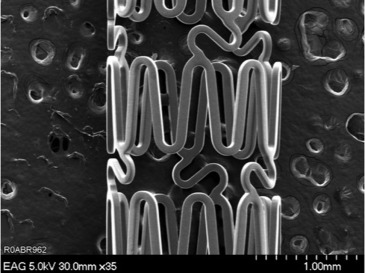
Drug-eluting stents (DES) have markedly reduced revascularization rates after percutaneous coronary interventions compared with bare metal stents. Despite these benefits, durable polymer DES exhibit delayed vessel healing, hypersensitivity reactions, and neoatheroma formation, resulting in delayed restenosis and repeat revascularization and late and very late stent thrombosis. Bioabsorbable polymer coatings degrade over months to years and allow delivery of an antiproliferative drug until the polymer disappears leaving behind a bare metal stent. Limiting the duration of polymer exposure to the endothelial wall is intuitively attractive as this limits the inflammatory exposure to the duration necessary to deliver the antiproliferative drug, thus offering potential for improved late safety and efficacy in comparison with durable polymer stents. The absorbable polymer sirolimus-eluting stent (APSES, MiStent; Micell Technologies, Durham, North Carolina) is a thin-strut, cobalt-chromium stent coated with crystalline sirolimus in a bioabsorbable polymer ( Figure 1 ). The combination of crystalline sirolimus within the bioabsorbable polymer enables the deposition of drug into the surrounding tissue and prolonged elution at a controlled rate, providing therapeutic tissue concentrations of sirolimus up to 9 months after implantation, without an initial burst of drug release. The coating is cleared from the stent in 45 to 60 days—leaving behind a bare metal stent—and is absorbed into the tissue within 90 days. However, comparative efficacy data against benchmark durable polymer DES remain scant. The purpose of this analysis was to compare the 3-year clinical outcomes of the MiStent APSES with the durable polymer everolimus-eluting stent (EES; Xience; Abbot Vascular, Abbott Park, Illinois) using pooled data from 3 trials and propensity score matching to account for baseline differences in patient risk.
Methods
This analysis included patients enrolled in the DES With Sirolimus and a Bioabsorbable Polymer for the Treatment of Patients With De Novo Lesions in the Native Coronary Arteries (DESSOLVE) I (enrolled 2010 to 2011) and II (enrolled 2012 to 2013) trials who received a MiStent APSES and a contemporary cohort of patients assigned to the EES from the Intracoronary Stenting and Angiographic Results: Test Efficacy of 3 Limus-Eluting Stents-4 (ISAR-TEST-4) trial (enrolled 2007 to 2008). Full details of the 3 trials have been published. DESSOLVE I was the first-in-human experience with the APSES, enrolling 30 patients at 5 centers with symptomatic coronary artery disease with stable or unstable angina pectoris and lesions with >50% diameter stenosis, amenable to coverage with a ≤23-mm-long stent in vessel sizes of 2.5 to 3.5 mm in diameter. Patients in consecutive groups of 10 underwent repeat angiography, intravascular ultrasound, and optical coherence tomography at 4, 6, or 8 months, and all patients had repeat angiography, intravascular ultrasound, and optical coherence tomography at 18 months of follow-up. The primary end point was angiographic in-stent late lumen loss. DESSOLVE II included 184 patients at 26 centers, randomized in a 2:1 manner to APSES or the zotarolimus-eluting stent (Endeavor Sprint; Medtronic Vascular, Santa Rosa, California). Patients were included if they had stable or unstable angina pectoris, a single, de novo, type A, B1, or B2 lesion of >50% diameter stenosis in a 2.5- to 3.5-mm diameter native coronary artery that could be covered with a ≤30-mm-long stent. Total occlusions, in-stent restenosis, highly calcified or thrombotic lesions, and lesions located at major bifurcations or in highly tortuous vessels were excluded from the study. The primary efficacy hypothesis was superiority of in-stent late lumen loss of APSES compared with ZES. The ISAR-TEST-4 trial was a randomized clinical trial with broad inclusion criteria, enrolling 2,603 patients at 2 clinics in Munich, Germany. Patients were randomized to either bioabsorbable polymer (n = 1,299) or durable polymer DES (n = 1,304); patients treated with durable polymer stents were randomly allocated to Xience EES (n = 652) or SES (Cypher; Cordis, Miami Lakes, Florida) (n = 652). We included only the EES arm of ISAR-TEST-4 in this analysis. The primary end point was the composite of cardiac death, target vessel–related myocardial infarction (MI), or target lesion revascularization (TLR). A detailed comparison of inclusion and exclusion criteria for the DESSOLVE and ISAR-TEST-4 studies is reported in Supplementary Table 1 . All patients were prescribed treatment with standard guideline-recommended dual antiplatelet therapy for 12 months.
Clinical end point measures were collected prospectively within each trial using standard definitions, and end points in this analysis are a combination of each study’s protocol-defined end points (detailed in Supplementary Table 2 ). All ISAR-TEST-4 MIs were independently re-adjudicated according to DESSOLVE trial definitions for poolablity of results. The primary clinical end point measure for this analysis was target lesion failure (TLF) defined as the composite of cardiac death, target vessel MI, and clinically indicated TLR. Secondary clinical end points include the patient-oriented composite of major adverse cardiac events defined as death, MI, and all target vessel revascularization. In addition, component end points are reported and include the following: all death, cardiac death, all MI, target vessel MI, clinically indicated TLR, and target vessel revascularization. Target vessel failure was defined as cardiac death, target vessel MI, and target vessel revascularization. Stent thrombosis was adjudicated according to the Academic Research Consortium criteria. An independent Clinical Event Committee adjudicated all events up to 3-year follow-up for each trial (DESSOLVE I and II; Harvard Clinical Research Institute, Boston, Massachusetts; ISAR-TEST-4; ISARESEARCH Center, Munich, Germany). Definitions of end points were similar across the 3 trials. Independent angiographic core laboratories assessed all angiographic end points (DESSOLVE I and II; Yale Cardiovascular Research Group, Yale University, New Haven, Connecticut; ISAR-TEST-4; ISARESEARCH Center) using the same software (CMS, version 7.1/7.2; Medis Medical Imaging Systems, Leiden, The Netherlands), and image acquisition was protocol guided. Baseline and postprocedure angiographic measures are reported in-stent and in-lesion defined as the stented segment and 5 mm on either edge of the stent.
The population for analysis and propensity score modeling was defined using the following rules: (1) only patients with single-vessel intervention who received the study stent were included; (2) those presenting with acute MI were excluded; and (3) those with total occlusions, thrombus, bifurcation lesions requiring side branch intervention, and ostial lesions were excluded. These criteria were selected based on the inclusion and exclusion of the more selective DESSOLVE trial populations. Treatment groups were matched through propensity scores. A logistic regression was fit with treatment (APSES vs EES) as the dependent variable against the following baseline covariates: age, gender, diabetes, smoking, hypertension, hypercholesterolemia, previous MI, PCI, and bypass, and angina status (stable vs nonstable), and whether the lesion required >1 stent and target vessel location (LAD, LCX, and RCA), reference vessel diameter, lesion length, American College of Cardiology/American Heart Association classification, and moderate/severe calcification. The logistic regression model fit was assessed through Hosmer-Lemeshow test. Patients were matched using the “greedy” algorithm with the maximum distance set at 0.1. A box plot of propensity scores before (but after applying exclusion criteria) and after matching was examined ( Figure 2 ). The c-statistic of the propensity score matching was 0.865 demonstrating excellent discrimination.

All statistical analyses were performed using SAS statistical software, and all statistical tests were conducted at the 2-sided, 0.05 significance level. For categorical variables, the number and percentage within each category of the parameter are presented. For continuous variables, the mean, SD, and minimum and maximum values are presented. In the matched sample, data were compared between groups using methods appropriate for the matched (correlated) nature of the data. The primary outcome variable, TLF, is presented as Kaplan-Meier estimates and compared between groups through marginal hazard ratios (HRs) and 95% confidence intervals (CIs) from the Cox proportional hazards regression using robust sandwich estimates of the variance. The assumption of proportionality was tested using the method of Lin et al.
As late angiographic follow-up was not planned/conducted in the DESSOLVE II study, sensitivity analyses were carried out to assess the robustness of the results to late angiographic follow-up for the primary outcome as follows: (1) all patients were censored at the time of their actual late angiographic follow-up. Patients without late angiographic follow-up were analyzed as usual and censored at their last known follow-up if before 3 years; (2) it was assumed that the covariates “early angiographic follow-up” and “late angiographic follow-up” proportionally affect the hazard of an event. Early and late angiographic follow-up were included in the model for TLF and treated as time-updated covariates for this analysis.
Results
A total of 805 patients (APSES = 153; EES = 652) were included in the overall analysis. Propensity score matching was performed in 204 patients (APSES = 102; EES = 102). Clinical follow-up was available in 98% (100 of 102) of APSES patients versus 88% (90 of 102) of EES patients. Baseline patient characteristics between APSES and EES in the overall population are displayed in Table 1 . There were significant differences between the groups. After matching, characteristics were well balanced between the groups ( Table 1 ). Mean age of the matched population was 66.5 years, 21% of them had diabetes and 24% unstable angina. Overlap of the propensity scores was excellent as demonstrated by the box plots ( Figure 2 ). The propensity model fit was good as assessed by the Hosmer-Lemeshow test (p = 0.28). The assumption of proportionality was not violated.
| Variable | All Patients | Matched Population | |||||||
|---|---|---|---|---|---|---|---|---|---|
| APSES (N=153) | EES (N=652) | Total (N=805) | P-Value | APSES (N=102) | EES (N=102) | Total (N=204) | P- Value | P- Value From GEE | |
| Age (years) | 64.49 ± 10.35 | 66.74 ± 10.29 | 66.31 ± 10.34 | 0.02 | 65.55 ± 9.48 | 66.32 ± 9.79 | 65.93 ± 9.62 | 0.57 | 0.55 |
| Male | 70% (107/153) | 78% (507/652) | 76% (614/805) | 0.04 | 71% (72/102) | 75% (76/102) | 73% (148/204) | 0.53 | 0.48 |
| Diabetes | 20% (30/151) | 28% (184/652) | 27% (214/803) | 0.04 | 22% (22/100) | 20% (20/102) | 21% (42/202) | 0.68 | 0.66 |
| Insulin Rx | 2% (3/151) | 9% (60/652) | 8% (63/803) | 0.003 | 2% (2/100) | 4% (4/102) | 3% (6/202) | 0.42 | 0.44 |
| Hypertension | 72% (109/152) | 68% (442/652) | 69% (551/804) | 0.35 | 73% (74/101) | 77% (78/102) | 75% (152/203) | 0.60 | 0.61 |
| Hyperlipidemia | 76% (114/151) | 65% (423/652) | 67% (537/803) | 0.01 | 72% (72/100) | 74% (75/102) | 73% (147/202) | 0.81 | 0.8 |
| Current smoker | 20% (30/151) | 16% (101/652) | 16% (131/803) | 0.19 | 15% (15/101) | 13% (13/102) | 14% (28/203) | 0.66 | 0.68 |
| Prior Myocardial Infarction | 22% (33/151) | 29% (191/652) | 28% (224/803) | 0.07 | 24% (24/101) | 21% (21/102) | 22% (45/203) | 0.59 | 0.6 |
| Prior Coronary Bypass | 3% (5/152) | 11% (69/652) | 9% (74/804) | 0.005 | 5% (5/102) | 6% (6/102) | 5% (11/204) | 0.76 | 0.74 |
| Prior PCI | 28% (42/153) | 53% (348/652) | 48% (390/805) | <0.0001 | 33% (34/102) | 31% (32/102) | 32% (66/204) | 0.76 | 0.75 |
| Unstable angina pectoris | 16% (24/153) | 31% (199/652) | 28% (223/805) | 0.0002 | 18% (18/102) | 29% (30/102) | 24% (48/204) | 0.048 | 0.045 |
| Stable angina pectoris | 77% (117/153) | 59% (383/652) | 62% (500/805) | <0.0001 | 75% (76/102) | 71% (72/102) | 73% (148/204) | 0.53 | 0.52 |
| Silent ischemia | 8% (12/153) | 0% (0/0) | 8% (12/153) | NA | 8% (8/102) | 0% (0/0) | 8% (8/102) | n/a | n/a |
Baseline lesion characteristics between APSES and EES in the overall population are displayed in Table 2 . There were significant differences between the groups. After matching, characteristics were well balanced between the groups ( Table 2 ). The number of stents implanted and procedure success per patient was similar, but the maximum deployment pressure was higher in the EES group. The preprocedure MLD was larger and the postprocedure MLD was smaller in the EES group (p <0.0001), resulting in a higher final in-stent and lesion diameter stenosis in the EES compared with the APSES group ( Table 2 ).
| Patients/Lesions | All Patients/Lesions | Matched Patients/Lesions | |||||||
|---|---|---|---|---|---|---|---|---|---|
| APSES (N=153/152) | EES (N=652/850) | Total (N=805/1002) | P-Value | APSES (N=102/101) | EES (N=102/105) | Total (N=204/206) | P-Value | P-Value GEE | |
| Lesions Treated | 1.14 ± 0.35 | 1.30 ± 0.54 | 1.27 ± 0.51 | 0.0003 | 1.14 ± 0.35 | 1.03 ± 0.17 | 1.08 ± 0.28 | 0.005 | 0.003 |
| Stents Implanted | 1.07 ± 0.28 | 1.26 ± 0.52 | 1.23 ± 0.50 | <0.0001 | 1.08 ± 0.30 | 1.04 ± 0.19 | 1.06 ± 0.25 | 0.25 | NA |
| Target lesion location | |||||||||
| Left Anterior Descending | 43% (65/153) | 44% (372/850) | 44% (437/1003) | 0.77 | 45% (46/102) | 41% (43/105) | 43% (89/207) | 0.55 | 0.55 |
| Left Circumflex | 22% (34/153) | 26% (223/850) | 26% (257/1003) | 0.30 | 28% (28/102) | 29% (30/105) | 28% (58/207) | 0.86 | 0.96 |
| Right | 35% (54/153) | 30% (255/850) | 31% (309/1003) | 0.19 | 28% (28/102) | 31% (32/105) | 29% (60/207) | 0.63 | 0.67 |
| ACC/AHA classification | |||||||||
| A | 32% (49/153) | 4.5% (38/850) | 8.7% (87/1003) | <0.0001 | 24% (24/102) | 23% (24/105) | 23% (48/207) | 0.91 | 0.95 |
| B1 | 45% (69/153) | 25% (208/850) | 28% (277/1003) | <0.0001 | 48% (49/102) | 50% (52/105) | 49% (101/207) | 0.83 | 0.69 |
| B2 | 22% (33/153) | 46% (390/850) | 42% (423/1003) | <0.0001 | 27% (27/102) | 24% (25/105) | 25% (52/207) | 0.66 | 0.48 |
| C | 1.3% (2/153) | 25% (214/850) | 22% (216/1003) | <0.0001 | 2% (2/102) | 3.8% (4/105) | 2.9% (6/207) | 0.43 | 0.4 |
| TIMI flow grade 3 | |||||||||
| Pre-TIMI | 92% (140/152) | 82% (693/850) | 83% (833/1002) | 0.001 | 89% (90/101) | 93% (98/105) | 91% (188/206) | 0.28 | 0.92 |
| Post-TIMI | 99% (150/152) | 96% (818/850) | 97% (968/1002) | 0.12 | 98% (99/101) | 99% (104/105) | 99% (203/206) | 0.54 | 0.55 |
| Pre-Procedure | |||||||||
| Lesion Length (mm) | 13.50 ± 4.77 | 15.18 ± 8.89 | 14.93 ± 8.41 | 0.02 | 13.47 ± 4.66 | 12.97 ± 6.61 | 13.22 ± 5.73 | 0.53 | 0.35 |
| RVD (mm) | 2.87 ± 0.37 | 2.80 ± 0.45 | 2.81 ± 0.44 | 0.09 | 2.83 ± 0.37 | 2.84 ± 0.41 | 2.84 ± 0.39 | 0.78 | 0.58 |
| MLD (mm) | 0.84 ± 0.22 | 0.99 ± 0.49 | 0.97 ± 0.47 | 0.0002 | 0.83 ± 0.22 | 1.11 ± 0.35 | 0.97 ± 0.33 | <0.0001 | NA |
| DS (%) | 70.48 ± 7.79 | 64.85 ± 15.98 | 65.71 ± 15.15 | <0.0001 | 70.31 ± 7.97 | 60.81 ± 11.69 | 65.49 ± 11.08 | <0.0001 | NA |
| Post Procedure In Stent | |||||||||
| MLD (mm) | 2.83 ± 0.34 | 2.59 ± 0.43 | 2.63 ± 0.43 | <0.0001 | 2.80 ± 0.34 | 2.66 ± 0.39 | 2.73 ± 0.37 | 0.005 | 0.15 |
| DS (% ) | 3.19 ± 7.29 | 11.83 ± 6.30 | 10.51 ± 7.17 | <0.0001 | 3.05 ± 7.64 | 10.92 ± 6.10 | 7.02 ± 7.93 | <0.0001 | <0.0001 |
| Post Procedure In-Lesion | |||||||||
| MLD, mm | 2.54 ± 0.38 | 2.25 ± 0.51 | 2.30 ± 0.50 | <0.0001 | 2.52 ± 0.40 | 2.29 ± 0.48 | 2.40 ± 0.46 | 0.0003 | 0.0009 |
| DS, (%) | 13.47 ± 7.55 | 23.60 ± 11.44 | 22.04 ± 11.52 | <0.0001 | 13.20 ± 7.61 | 23.70 ± 10.20 | 18.50 ± 10.42 | <0.0001 | <0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


