Acute coronary syndromes (ACS) in patients with diabetes mellitus (DM) are associated with a high risk for major adverse cardiovascular events (MACEs) despite statin treatment. The impact of combined bezafibrate and statin therapy in patients with DM and ACS has not been specifically investigated. The aim of this study was to evaluate the association of combined therapy with 30-day MACEs in patients with DM participating in the nationwide Acute Coronary Syndrome Israeli Surveys (ACSIS). The study population comprised 3,063 patients with DM from the ACSIS 2000, 2002, 2004, 2006, 2008, and 2010 enrollment waves who were alive at discharge and received statins. Of these, 225 (7.3%) received on discharge combined bezafibrate and statin therapy, and 2,838 (92.7%) were treated with statins alone. MACEs were defined as a composite measure of death, recurrent myocardial infarction, recurrent ischemia, stent thrombosis, ischemic stroke, and urgent revascularization. The development of 30-day MACEs was recorded in 8% patients receiving combination therapy and 14.2% of those receiving statins alone (p = 0.01). Crude 1-year mortality and 30-day rehospitalization rates were also significantly lower in patients receiving combination therapy: 4.0% versus 8.1% (p = 0.03) and 13.3% versus 21.6% (p = 0.003), respectively. Multivariate analysis identified combined therapy as an independent predictor of reduced risk for 30-day MACEs, with an odds ratio of 0.56 (95% confidence interval 0.34 to 0.92), corresponding to a 44% relative risk reduction. In conclusion, a significantly lower risk for 30-day MACEs was observed in statin-treated patients with DM who also received bezafibrate after ACS. Signals regarding improvement of 30-day rehospitalization and 1-year mortality rates emerged as well.
Acute coronary syndromes (ACS) are associated with a high risk for subsequent major adverse cardiovascular events (MACEs), and patients with diabetes mellitus (DM) are at especially elevated risk. The markedly increased level of MACEs associated with DM after the acute phase points out the important roles of several mechanisms, including excessive oxidative stress, enhanced inflammatory response, and procoagulatory state with elevated fibrinogen and C-reactive protein levels along with platelet hyperactivity. Early initiation of statins is one of the cornerstones of the treatment of patients with ACS. However, despite the almost ubiquitous use of statins after ACS, a significant number of recurrent MACEs still occur, and in particular, many patients with DM remain at high residual cardiovascular risk. Bezafibrate is a pan–peroxisome proliferator-activated receptor ligand with the ability to increase high-density lipoprotein cholesterol and reduce insulin resistance, the level of blood glucose, triglycerides, markers of systemic inflammation, and fibrinogen. Because of these effects, bezafibrate could be considered a good potential candidate for reducing residual cardiovascular risk in patients with DM after ACS. However, the possible impact of bezafibrate on MACEs in patients with DM within the setting of ACS has not been specifically investigated. The aim of this study was to evaluate the association of combined bezafibrate and statin treatment with the 30-day rate of MACEs in patients with DM participating in the nationwide Acute Coronary Syndrome Israeli Surveys (ACSIS). In addition, 30-day rehospitalization and 1-year mortality rates were assessed.
Methods
Our patients were drawn from the ACSIS 2000, 2002, 2004, 2006, 2008, and 2010 enrollment waves. Details of the ACSIS registry have been previously reported.
In brief, the ACSIS registry is a 2-month nationwide survey conducted biennially that prospectively collects data from all ACS admissions at all 25 coronary care units in Israel. Patient management was at the discretion of the attending physicians. Eligibility for the study was validated before discharge from the coronary care unit. Discharge diagnoses were recorded as determined by the attending physicians on the basis of clinical, electrocardiographic, and enzymatic criteria. Demographic, historical, and clinical data, including medical management, were recorded on prespecified forms by dedicated study physicians. The Central Data Coordinating Center (based at the Sheba Medical Center) was responsible for the collection of all case report forms, and the Israel Heart Society was responsible for keeping the survey database. Thirty-day outcome rates and 1-year mortality rate were ascertained by hospital chart review, telephone contact, and use of the Israeli National Population Registry. Of the 8,980 patients who were alive at discharge from the hospital and were receiving statins and for whom 30-day MACE rates were available, 3,063 (34.1%) were diagnosed with DM; 94.9% had type 2 DM, and 5.1% had type 1 DM. Of the 3,063 patients with DM, 225 (7.3%) received on discharge combined bezafibrate and statin treatment, and 2,838 (92.7%) were treated with statins alone.
This registry-based analysis of preexisting data was conducted according to the ethical guidelines of the 1975 Declaration of Helsinki. The ACSIS registry was approved by the ethics committee of the each participating center. All patients provided written informed consent for the collection of data and subsequent analysis.
In our study, we used prespecified definitions of the ACSIS registry. The diagnosis of DM was made by the attending physician on the basis of the reported history, medical records, and/or for patients with fasting blood glucose levels ≥126 mg/dl (7 mmol/L) registered twice or taking any type of pharmacologic antidiabetic treatment before enrollment. The diagnosis of hypertension was made on the basis of the reported history, medical records, and/or for patients with blood pressures >140/90 mm Hg registered twice or treatment with antihypertensive drugs before enrollment. Attending physicians in all participating institutions were specifically instructed to use these uniform diagnostic criteria.
Primary end points of our study were the 30-day MACE rate (which was defined as a composite measure of 30-day all-cause mortality, recurrent myocardial infarction, recurrent ischemia, stent thrombosis, ischemic stroke, and urgent revascularization). Secondary end points were 30-day rehospitalization and 1-year mortality rates.
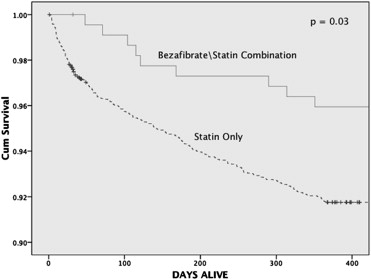
Statistical analysis was performed using SPSS version 19 (SPSS, Inc., Chicago, Illinois). Categorical variables are expressed as percentages and continuous variables as mean ± SD. Comparisons of variables were performed using chi-square and Fisher’s exact tests for categorical variables and unpaired analyses of variance for continuous variables. Survival curves were derived using the Kaplan-Meier approach, and unadjusted comparisons of survival curves were performed using the log-rank test.
To determine whether the combination of bezafibrate and statin versus statin only at discharge was an independent explanatory variable for 30-day MACEs, multivariate logistic regression analysis was applied with adjustment for the following prespecified variables: age, gender, smoking status, hypertension, and chronic renal failure. Results are presented as odds ratios with appropriate 95% confidence intervals. All tests were 2 sided, and p values <0.05 were considered statistically significant.
Results
Our population was categorized into 2 groups: (1) diabetic patients receiving on discharge statin monotherapy (n = 2,838) and (2) diabetic patients receiving on discharge combined bezafibrate and statin treatment (n = 225).
The main clinical and laboratory characteristics of patients are presented in Tables 1 and 2 . Most patients in the 2 groups were men. Patients who received bezafibrate were younger. However, these patients included significantly more current smokers and patients with hypertension, and they had unfavorable cardiometabolic profiles (with respect to weight, body mass index, and total cholesterol, triglyceride, and high-density lipoprotein cholesterol levels). Markedly elevated enzymes on admission (troponin and/or creatine kinase-MB) were registered in 99% of patients from the 2 groups. No significant differences between the groups were found for history of stroke, chronic renal failure, peripheral vascular disease, and in-hospital cardiac interventions.
| Characteristic | Statin Alone (n = 2,838) | Bezafibrate and Statin (n = 225) | p Value |
|---|---|---|---|
| Age (yrs) | 65.3 ± 11.3 | 60.3 ± 11.6 | <0.0001 |
| Body mass index (kg/m 2 ) | 28.31 ± 4.6 | 30 ± 4.6 | <0.0001 |
| Weight (kg) | 80.1 ± 14.4 | 86.6 ± 15.3 | <0.0001 |
| Women | 828 (29.2) | 59 (26.2%) | 0.35 |
| Hypertension | 2,038 (72%) | 176 (78%) | 0.046 |
| Current smokers | 782 (28%) | 84 (37%) | 0.002 |
| Past smokers | 623 (22%) | 59 (26%) | 0.16 |
| Previous stroke | 302 (11%) | 22 (9.8%) | 0.68 |
| Chronic renal failure | 434 (15%) | 38 (17%) | 0.52 |
| Peripheral vascular disease | 383 (14%) | 28 (12%) | 0.65 |
| Typical chest pain | 2,034 (72%) | 180 (80%) | 0.01 |
| Atypical chest pain | 561 (20%) | 45 (20%) | 0.99 |
| ST-segment elevation | 1,096 (39%) | 69 (31%) | 0.04 |
| Characteristic | Statin Alone (n = 2,838) | Bezafibrate and Statin (n = 225) | p Value |
|---|---|---|---|
| Coronary bypass | 145/2,833 (5.1%) | 13/225 (5.8%) | 0.667 |
| Percutaneous coronary intervention | 1,158/2,511 (46.1%) | 107/205 (52.2%) | 0.093 |
| Only angiography | 487/2,225 (21.9%) | 40/180 (22.2%) | 0.917 |
| Systolic blood pressure (mm Hg) | 146.40 ± 29.4 | 146.50 ± 23.9 | 0.960 |
| Diastolic blood pressure (mm Hg) | 81.58 ± 16.4 | 82.57 ± 13.9 | 0.380 |
| Heart rate (beats/min) | 84.40 ± 20.4 | 81.85 ± 18.2 | 0.07 |
| Glucose (mg/dl) | 202.25 ± 93.9 | 203.02 ± 97.7 | 0.916 |
| Total cholesterol (mg/dl) | 181.33.27 ± 47.9 | 197.84 ± 49.6 | <0.0001 |
| High-density lipoprotein cholesterol (mg/dl) | 40.25 ± 13.6 | 34.92 ± 8.9 | <0.0001 |
| Low-density lipoprotein cholesterol (mg/dl) | 103.63 ± 38.2 | 101.78 ± 44.2 | 0.575 |
| Triglycerides (mg/dl) | 176.24 ± 179.5 | 374.0 ± 259.5 | <0.0001 |
| Creatinine (mg/dl) | 1.27 ± 0.9 | 1.20 ± 0.6 | 0.237 |
Data regarding treatment with cardiovascular drugs among the study groups are presented in Table 3 . There were no significant differences in the proportion of patients receiving cardiovascular drugs.
| Medication | Statin Alone (n = 2,838) | Bezafibrate and Statin (n = 225) | p Value |
|---|---|---|---|
| Aspirin | 96% | 95% | 0.52 |
| Clopidogrel | 68% | 71% | 0.28 |
| β blockers | 83% | 88% | 0.94 |
| Nitrates | 24% | 23% | 0.83 |
| Calcium channel blockers | 22% | 24% | 0.48 |
| Diuretics | 32% | 30% | 0.60 |
| Aldosterone antagonist | 8% | 7% | 0.40 |
| Angiotensin-converting enzyme inhibitors | 72% | 78% | 0.16 |
| Angiotensin receptor blockers | 12% | 15% | 0.53 |
| Insulin | 22% | 25% | 0.23 |
During the follow-up period of 30 days, MACEs were recorded in 14.2% patients from the statin monotherapy group and 8% from the combined bezafibrate and statin group (p = 0.01; Table 4 ).
| Outcome | Frequency Missing | Statin Alone (n = 2,838) | Bezafibrate and Statin (n = 225) | p Value |
|---|---|---|---|---|
| 30-day MACEs | — | 402 (14.2%) | 18 (8%) | 0.01 |
| 30-day rehospitalization | — | 614 (21.6%) | 30 (13.3%) | 0.003 |
| 1-yr all-cause mortality | 16 | 228 (8.1%) | 9 (4.0%) | 0.03 |
Crude 1-year mortality and 30-day rehospitalization rates were also significantly lower in patients from the bezafibrate and statin group than in their counterparts from the statin monotherapy group: 4.0% versus 8.1% (p = 0.03) and 13.3% versus 21.6% (p = 0.003), respectively.
Kaplan-Meier analysis ( Figure 1 ) showed that the cumulative probability of survival at 1 year of follow-up (in accordance with the time of occurrence) was significantly higher in patients who received combined bezafibrate and statin therapy compared with those who received statin monotherapy, with early separation of event rates between the 2 treatment groups (log-rank p = 0.03 for the overall difference during follow-up).