The objective of this prospective cohort study was to describe real-life use of lipid-lowering drugs and low-density lipoprotein cholesterol (LDL-C) target-attainment rates 1 year after acute myocardial infarction (AMI). LDL-C was recorded at hospital admission for AMI and at follow-up at 2 and 12 months after AMI in 17,236 patients in the Swedish heart registry, SWEDEHEART, from 2004 through 2009. Lipid-lowering treatments were identified using the Swedish Prescribed Drug Register. More than 90% of patients received statins after AMI. Simvastatin ≤40 mg was used by 80% of patients at discharge and at 2 months and 68% at 1 year after AMI. Intensive statin therapy (LDL-C-lowering capacity >40%) was prescribed for 8.4%, 11.9%, and 12.2% at these time points, and combinations of statin/ezetimibe for 1.1%, 2.8%, and 5.0%, respectively. The LDL-C target of <2.5 mmol/L (97 mg/dl) was achieved in 74.5% of patients at 2 months and 72.3% at 12 months after AMI. Treatment was intensified for only 21.3% of patients with LDL-C above target at 2 months. In multivariate analysis, higher LDL-C levels at admission and at 2 months correlated to increased risk for under treatment at 12 months after AMI. In conclusion, statin treatment after AMI in Sweden has become standard, but titration to reach recommended LDL-C levels is still suboptimal. Strategies to further improve implementation of guidelines are needed.
Despite the overwhelming evidence for the benefit of lipid-lowering drugs in reducing cardiovascular events in patients with established cardiovascular disease or high risk profile and clear recommendations for target levels in national and international guidelines, repeated surveys in Europe have shown substantial room for improvement regarding target achievement in routine clinical practice.
The objective of the present study was to describe real-life use of lipid-lowering drugs and resulting low-density lipoprotein cholesterol (LDL-C) target attainment rates at 2 and 12 months after acute myocardial infarction (AMI) in a large unselected cohort of AMI patients in Sweden.
Methods
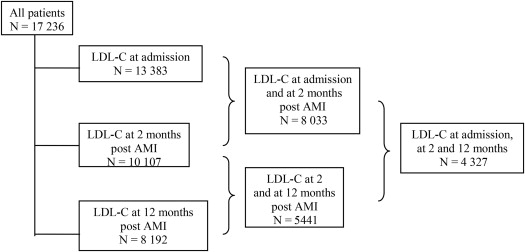
SWEDEHEART is a national registry prospectively collecting data regarding baseline characteristics, treatments in hospital, medication at discharge, and outcome for consecutive patients with acute coronary syndromes treated in all Swedish coronary care units (CCU). Participation in SWEDEHEART is voluntary for each hospital. Development and core management of the registry is funded by the Swedish Health Authorities, but participating hospitals receive no extra funding. A module covering secondary prevention and cardiac rehabilitation for patients up to 75 years of age in SWEDEHEART was launched in 2005, involving an increasing number of centers during the study period from 32 to 62 (84% of all Swedish hospitals providing care for AMI) in 2009. LDL-C was measured at admission to the CCU and at follow-up visits at 2 months and at 1 year after AMI, and recorded in the registry. LDL-C measurement was not mandatory in the registry, resulting in the differences in population sizes seen in Figure 1 .
The Swedish Prescribed Drug Register started in July 2005 and includes all dispensed prescriptions in Swedish pharmacies for all Swedish citizens. It contains prescription and dispensing dates, dispensed amount of the drug, and personal identification number of each individual. Drugs are coded according to the World Health Organization Anatomical Therapeutic Chemical Classification.
The database from SWEDEHEART for the period from December 2004 through June 2009 was merged with the Swedish Prescribed Drug Register creating an anonymous study database. December 2004 was chosen as study start to allow inclusion of baseline data for patients with their first follow-up visit in January 2005. Patients aged <75 years, participating in the 2-month and/or 1-year follow-up in the SWEDEHEART registry and with ≥1 purchase of any lipid-lowering drug (Anatomical Therapeutic Chemical Classification code C10 A) during the study period were identified (n = 17,236). This constituted nearly half of the total number of AMI patients (38,818) in this age group admitted to a CCU in Sweden during the study period.
LDL-C was measured in 78% (13,383) of patients at admission for AMI, 63% (10,107) of the 15,995 patients completing the 2-month follow-up and in 66% (8,192) of the 12,355 patients completing the 1-year follow-up: 989 patients died during the study period, and 3,276 patients were censored for the 1-year, but not the 2-month, follow-up because of closure of the study database in June 2009. Treatment before admission for AMI was unknown for 3,027 patients admitted in 2004 through 2005 because the Swedish Prescribed Drug Register started in July 2005. These patients were included in the study to contribute to the description of current post-AMI treatment practices. Patients with registered LDL-C values at each time point are shown in Figure 1 .
According to Swedish law, no written informed consent is needed for registration of a patient in the SWEDEHEART registry. All patients are informed of their participation in the registry and have the right to withdraw their participation; no patients within this study have chosen to do so. This study was approved by the Uppsala Ethical Review Board.
On the basis of a meta-analysis of the relative effect of statins, statins at doses capable of lowering LDL-C by >40% were considered as a group (“intensive statin therapy”) compared with a group of statins at doses capable of LDL-C lowering of <40% (“moderate statin therapy”). Treatment with combinations of statin and ezetimibe were also analyzed.
To define the lipid-lowering drug treatment used before a visit, a run-in period of 6 months was used. This run-in period can be justified using the waiting-time distribution, in this case allowing for varying time intervals between patients drug purchases. The most potent statin (according to Table 1 ), if >1, dispensed at the latest dispensation date during the 6 months before the visit was selected. The same was done for nonstatins, allowing for combination treatments. Treatment after a follow-up visit was defined similarly, with a time interval from 2 weeks before the visit to 2 weeks after the visit. This 4-week interval was included because protocol allowed for LDL-C analyses during this period, and treatment could thus be altered accordingly. To describe the physician’s treatment strategy in response to current lipid status, prescription dates instead of dispensation dates were used. If there were no new prescriptions during these 4 weeks, the patient was considered to have continued the same treatment as before the visit.
| Daily Dose, mg (Reductions in LDL-C) | |||||
|---|---|---|---|---|---|
| Statin | 5 | 10 | 20 | 40 | 80 |
| Rosuvastatin | 1.84 (38%) | 2.08 (43%) | 2.32 (48%) | 2.56 (53%) | 2.80 (58%) |
| Atorvastatin | 1.51 (31%) | 1.79 (37%) | 2.07 (43%) | 2.36 (49%) | 2.64 (55%) |
| Simvastatin | 1.08 (23%) | 1.31 (27%) | 1.54 (32%) | 1.78 (37%) | 2.01 (42%) |
| Fluvastatin | 0.46 (10%) | 0.74 (15%) | 1.02 (21%) | 1.30 (27%) | 1.58 (33%) |
| Pravastatin | 0.73 (15%) | 0.95 (20%) | 1.17 (24%) | 1.38 (29%) | 1.60 (33%) |
Univariate comparison of target attainment rate for dichotomous variables was done using 2-sided Fischer’s exact test. For each follow-up visit, the probability of reaching the treatment target of LDL-C ≤2.5 mmol/L (97 mg/dl) was assessed, for patients with results greater than the LDL-C target at the previous visit, using a logistic regression model. As explanatory variables, the models included gender, age (linear term), diabetes, previous myocardial infarction, stroke, previous revascularization, hypertension, statin treatment before admission, smoking status, year of AMI, treated and untreated LDL-C (linear term), and statin treatment before follow-up visit. The model for the first follow-up thus included only patients with LDL-C >2.5 mmol/L at admission, and the model for the second follow up included only patients with LDL-C >2.5 mmol/L at the first follow-up. The model was applied to the subset of patients with LDL-C measured on 2 consecutive occasions and having complete information from the Prescribed Drug Registry. All analyses were performed with the statistical program R version 2.10.1.
Results
Baseline characteristics of the total study population are outlined in Table 2 , including sociodemographic factors, medical history, previous and new coronary interventions, and mean LDL-C-levels at admission for AMI and at the first and second follow-ups. The proportion of patients using lipid-lowering treatment before admission for AMI was 27.4%, and LDL-C at admission was ≤2.5 mmol/L (97 mg/dl) for 63.8% of those patients (data not shown).
| Total (n = 17,236) | |
|---|---|
| Percentage (n) Mean ± SD | |
| Male | 73.9% (12,745) |
| Female | 26.1% (4,491) |
| Age (yrs) | 61.9 ± 8.5 |
| Diabetes mellitus | 19.7% (3,392) |
| Previous myocardial infarction | 15.9% (2,741) |
| Previous percutaneous coronary intervention | 10.1% (1,736) |
| Previous coronary artery bypass surgery | 6.4% (1,111) |
| Hypertension | 40.4% (6,958) |
| Statin treatment before admission ∗ | 27.4% (3,888) |
| Smoker at admission | 31.6% (5,444) |
| Body mass index † | 27.4 ± 4.3 |
| Percutaneous coronary intervention during hospital stay | 69.8% (12,031) |
| LDL-C at admission † (n = 13,383) | 3.1 ± 1.1 |
| LDL-C at 2 months after AMI † (n = 10,107) | 2.2 ± 0.7 |
| LDL-C at 1 year after AMI † (n = 8192) | 2.3 ± 0.8 |
∗ Statin treatment before admission (n = 14,209) was unknown for patients with AMI in 2005, which was before initiation of the Prescribed Drug Register.
† BMI (n = 13,604) and LDL-C were not recorded for all patients.
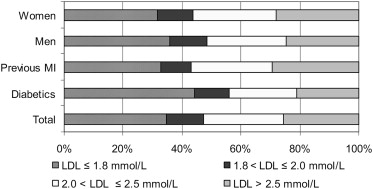
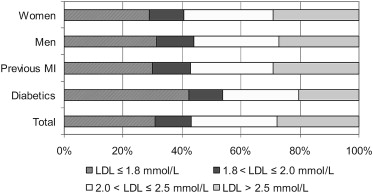
Target LDL-C was achieved in 74.5% of all patients 2 months after AMI and in 72.3% at 1 year. Patients with diabetes had better lipid control rates: 79.1% and 79.5% versus 73.4% and 70.6% at 2 and 12 months after AMI (p <0.001 for both time points). There were only small differences in lipid control rates between men and women (31.3% vs 29.1% at admission, 75.4% vs 72.1% at 2 months and 72.8% vs 70.8% at 12 months; Figures 2 and 3 ).
Within 14 days of the discharge date after AMI, 95.3% of all patients used a lipid-lowering drug, according to definition of treatment in the Methods section. This proportion decreased to 92.9% at 1 year. Among patients not reaching LDL-C treatment target at follow-up 2, the corresponding proportion was 88.7% at 1 year.
The most frequent lipid-lowering drug after AMI was simvastatin 20 or 40 mg, which was prescribed for 80.5% of patients at discharge, 78.0% after 2 months, and 68.0% after 1 year. Intensive statin therapy (simvastatin 80 mg, atorvastatin 20 to 80 mg, or rosuvastatin 10 to 80 mg) was prescribed for 8.4% of the patients at discharge, 11.9% after 2 months, and 12.2% after 1 year. Corresponding proportions for the combination of a statin and ezetimibe were 1.1%, 2.8%, and 5.0%. Total use of nonstatins other than ezetimibe was <2.5% at all time points (data not shown). The most frequent drug in the intensive statin therapy group was 80 mg atorvastatin at discharge and after 2 months (3.9% and 4.7%) and atorvastatin 40 mg after 1 year (4.0%).
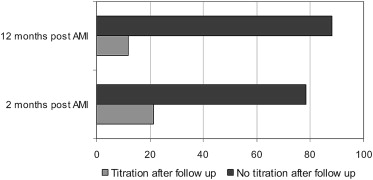
Treatment was intensified (i.e., increased dose or switch to a more potent drug) for 21.3% of patients with LDL-C above recommended level at the first follow-up, and for 12.0% of such patients at the second follow-up ( Figure 4 ).
At the 2-month follow-up, patients with diabetes were more likely to reach the target, whereas previous statin treatment, higher LDL-C at admission (both treated and untreated values), smoking at admission, and history of myocardial infarction were factors correlating to increased risk of not reaching treatment target. At the 1-year follow-up, higher LDL-C at admission (both treated and untreated values) and higher LDL-C at follow-up 1 were associated with increased risk of not reaching treatment target ( Table 3 ).
| Variable | Follow-up 1 | Follow-up 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate OR (95% CI) | p Value | Multivariate OR (95% CI) | p Value | Univariate OR (95% CI) | p Value | Multivariate OR (95% CI) | p Value | |
| Female gender | 1.19 (1.04-1.37) | 0.013 | 1.12 (0.96–1.32) | 0.14 | 0.99 (0.75–1.30) | 0.94 | 0.83 (0.60–1.15) | 0.26 |
| Age (by SD) | 0.95 (0.89–1.01) | 0.10 | 0.95 (0.89–1.03) | 0.20 | 1.07 (0.94–1.21) | 0.30 | 0.93 (0.79–1.08) | 0.34 |
| Diabetes mellitus | 0.88 (0.72–1.07) | 0.20 | 0.72 (0.57–0.90) | 0.004 | 0.84 (0.59–1.20) | 0.34 | 0.69 (0.44–1.07) | 0.097 |
| Previous MI | 2.15 (1.75–2.64) | <0.001 | 1.56 (1.15–2.10) | 0.004 | 1.20 (0.85–1.70) | 0.30 | 1.12 (0.66–1.92) | 0.67 |
| Previous stroke | 1.55 (1.12–2.15) | 0.009 | 1.31 (0.91–1.91) | 0.15 | 1.27 (0.71–2.29) | 0.41 | 1.10 (0.56–2.14) | 0.79 |
| Previous revascularization | 1.98 (1.58–2.47) | <0.001 | 1.03 (0.74–1.44) | 0.87 | 1.46 (0.99–2.13) | 0.053 | 1.50 (0.82–2.74) | 0.19 |
| Hypertension | 0.97 (0.85–1.11) | 0.66 | 0.86 (0.74–1.00) | 0.051 | 1.16 (0.89–1.51) | 0.27 | 1.01 (0.74–1.38) | 0.95 |
| Smokers | 1.47 (1.26–1.72) | <0.001 | 1.62 (1.36–1.93) | <0.001 | 0.99 (0.73–1.35) | 0.96 | 0.99 (0.69–1.43) | 0.97 |
| LDL-C measured at admission; treated; by 1 mmol/L | 2.20 (2.01–2.40) | <0.001 | 2.46 (2.23–2.71) | <0.001 | 2.46 (1.61–3.76) | <0.001 | 3.24 (1.94–5.40) | <0.001 |
| LDL-C measured at admission; untreated; by 1 mmol/L | 1.29 (1.03–1.62) | 0.027 | 1.36 (1.06–1.75) | 0.014 | 1.37 (1.16–1.62) | <0.001 | 1.62 (1.33–1.98) | <0.001 |
| Statin treatment before admission | 2.94 (2.47–3.50) | <0.001 | 32.7 (13.1–82.1) | <0.001 | ||||
| LDL-C measured at follow-up 1; treated; by 1 mmol/L | — | — | 2.18 (1.57–3.03) | <0.001 | 2.22 (1.49–3.31) | <0.001 | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


