Sinus of Valsalva aneurysm is a rare cardiac malformation that stems from incomplete fusion of the aortic media and the aortic valve annulus, a weakness that may result in rupture of the sinus, large left-to-right shunt, and severe congestive heart failure. Historically, this lesion has been repaired surgically, but percutaneous closure (PC) has emerged as a therapeutic intervention over the last 20 years. We review and contrast 34 studies detailing the PC approach with 16 studies on surgical closure (SC), together comprising a total of 877 patients who were treated for ruptured sinus of Valsalva aneurysm from 1956 to 2014. Both groups had similar sites of rupture, age distribution, and clinical symptoms at presentation. Selection bias ultimately prohibits a direct comparison between the 2 groups as patients who underwent SC often had worse aortic regurgitation and more complex associated lesions, including endocarditis, bicuspid aortic valve, tunnel-type fistulous connections, larger defect size, and multiple site of rupture. In conclusion, although SC is indicated and reserved for these more complicated patients, our review of previously published reports reveals that PC in patients who are too ill to undergo bypass, with mild or no aortic regurgitation and simple associated defects (muscular ventricular septal defects, secundum atrial septal defect, small patent ductus arteriosus), can be safe, effective, and practical.
Sinus of Valsalva aneurysm (SOVA) is a rare cardiac malformation that stems from incomplete fusion of the aortic media and the aortic valve annulus, the cause of which is a deficiency in the elastin layer of the aortic wall. A ruptured aneurysm in this location has historically been repaired surgically. However, since Cullen et al described the first percutaneous closure (PC) in 1994, this less invasive approach has been increasingly used and can be a viable alternative to closure in select cases. The rarity of SOVA and its scattered multinational incidence make it a difficult entity to track and study. We present a systemic review of 37 retrospective case studies (1994 to 2014) with a total of 136 patients who underwent PC of ruptured SOVA. We also reviewed 16 studies (1988 to 2013) from surgical cohorts, representing 741 individual patients. Although selection bias, difference in era of intervention, and limitations in long-term follow-up inevitably prohibit a direct comparison of outcomes between the 2 groups, we offer a discussion of the results and potential guidelines for management.
Pathophysiology
Edwards and Burchell described SOVA in autopsy specimens as defects above the level of the aortic cusps in which there is lack of continuity between the aortic media and the annulus fibrosis. This may later initiate aneurysm formation, leading to local flow turbulence, laminar flow separation, or dilatation of the annulus and valve cusps. Most commonly, the right coronary or noncoronary sinuses are implicated in rupture, communicating anteriorly with the right ventricle (through the outlet septum or crista supraventricularis) or posteriorly to the right atrium.
Rupture may be due to a gradual enlargement of a congenital defect or may be secondary to bacterial endocarditis or atherosclerosis. The incidence of acute endocarditis associated with rupture is unknown, although between 2% and 30% of patients reported remote histories of endocarditis in larger surgical series.
In patients undergoing open heart surgery, SOVA is more prevalent in Asian (1.2% to 4.9%) than in Western populations (0.14% to 1.5%). A ventricular septal defect is the most commonly associated defect (49% in surgical series), along with bicuspid aortic valve, infundibular pulmonary stenosis, patent ductus arteriosus, atrial septal defect, coarctation and aortic regurgitation (AR), or aortic stenosis. Asian populations more frequently had ventricular septal defects (VSDs) of the supracristal type.
Surgical Repair of Ruptured SOVA
Ruptured SOVA was always repaired, even if patients were asymptomatic and only diagnosed when a continuous murmur was found on routine examination. Although its natural history is not well understood, asymptomatic, unruptured SOVA, usually found during unrelated imaging studies, was almost always repaired in larger surgical series, and documented anecdotal cases advocate for early intervention. For example, a Jehovah’s Witness with an unruptured aneurysm had refused surgery, but over the next 4 years, he developed severe AR, extension of the aneurysm to the right and left coronary sinuses, and dilatation of the aortic annulus. Vural et al proposed that patients with unruptured, stable aneurysms should be anticoagulated, followed at 6-month intervals, and then repaired if symptoms develop or the size of the sinus is >50% of the average size of the other 2 normal Valsalva sinuses, compresses or distorts surrounding chambers or tissues, or increases in consecutive echocardiographic examinations.
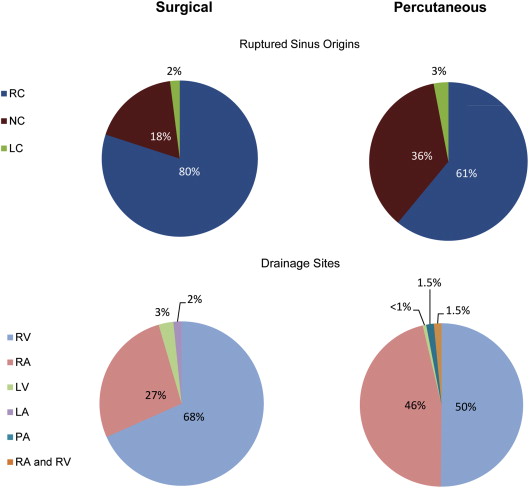
For the purpose of this discussion, only surgical series that investigated ruptured SOVA (n = 741, 67% men) were considered. The chambers of rupture and drainage are shown in Figure 1 . Until the use of routine 2-dimensional echocardiography, most patients were diagnosed with angiography. Several investigators report an echocardiographic accuracy rate of >90%, with the most error occurring in the accurate identification of the chamber of drainage. In the current era, angiography is typically reserved for characterization of coronary artery disease in older patients.
Of the 656 patients in whom symptoms were reported, 88% (n = 583) presented with exertional dyspnea, palpitations, fever, chest pain, fatigability, or a combination of these. Symptom onset was further characterized in 328 patients, with 36% (n = 121) of patients presenting suddenly, requiring early repair. The remaining patients were repaired electively within 2 to 4 months. New York Heart Association class was reported in 517 patients, with 52% (n = 269) presenting in class 3and 4, and mean Qp:Qs (reported in 140 patients) was 2.35 (range 1.9 to 2.9).
Investigators chose 1 of 3 accepted operative approaches to closure: through the ruptured cardiac chamber, through an aortotomy, or by a combined approach. The ruptured sites were closed directly or with prosthetic or pericardial patches. Some investigators describe a greater incidence of recurrent fistulas in patients who underwent direct closure, although others found no differences in recurrence or AR related to surgical approach, and this remains an area of contention.
Of the 741 patients ( Table 1 ), early mortality was low at 1.5% (n = 11). The range of follow-up tracking late deaths was extremely variable, from several months to 37 years. Abe and Komatsu reported a late actuarial survival rate at 25 years of 86 ± 7%. Typical causes of late death included anticoagulation-related hemorrhage, endocarditis, other organ failure, and congestive heart failure from myocardial disease. Total event-free survival has collectively improved over the last 2 decades.
| Publication (years of recruitment) | Number of patients | Age (years) | Aortic regurgitation | Aortic valve repair | New aortic regurgitation | Follow up (years) | Re-operation for aortic regurgitation | Progressive aortic regurgitation | Early/Late Death |
|---|---|---|---|---|---|---|---|---|---|
| Abe (1961-87) | 31 | 23 (3-58) | 12 (38%) | 5 (16%) | not reported | 11.1 ±7.6 | 4 (13%) | 4 (1.3%) | 1/4 (3.2%/13%) |
| Agrawal (1979-90) | 22 | 28.5 (15-45) | 8 (36%) | 5 (9%) | 0 | 5 (0.5-10) | 0 | 0 | 1/0 (4.5%/0%) |
| Au (1978-96) | 53 | 36 (13-65) | 23 (43%) | 14 (26%) | 0 | 6.5 ±4.9 | 2 (3.8%) | 1 (1.9%) | 0/5 (0%/9.4%) |
| Azakie (1970-98) | 34 | 31.6 (7-57) | 24 (70%) | 11 (32%) | not reported | 9.2 ±8.3 | 6 (18%) | 6 (1.8%) | 0/4 (0%/12%) |
| Choudhary (1977-96) | 104 | 27.5 (5-62) | 45 (43%) | 27 (26%) | 3 (2.9%) | 8.2 (1-20) | 0 | 2 (1.9%) | 2/1 (2%/2%) |
| Dong C (1996-01) | 67 | 32 (2-57) | 12 (17%) | 12 (18%) | not reported | 2.1 (0.1-4.9) | 0 | 1 (1.5%) | 1/1 (1.5%/1.5%) |
| Dong R (1997-07) | 43 | 29 (11-50) | 15 (34%) | not reported | not reported | 5.7 (1-10) | 2 (4.7%) | 2 (4.7%) | 0/0 |
| Hamid (1978-93) | 25 | 26 (11-49) | not reported | not reported | not reported | 5.5 (0.3-15) | 1 (4%) | 3 (12%) | 1/1 (4%/4%) |
| Jung (1990-06) | 56 | 33.2 (14-64) | 8 (14%) | 9 (16%) | 5 (9%) | 3.8 (0.1-15) | 4 (7.1%) | 11 (20%) | 0/2 (0%/3.6%) |
| Kirali (1985-99) | 20 | 28.3 (14-55) | 4 (20%) | 4 (20%) | 1 (5%) | 4.4 (1-13) | 1 (5%) | 0 | 1/0 (5%/0%) |
| Lin (1980-01) | 17 | 33.5 (22-59) | 8 (47%) | 8 (47%) | 0 | 11.5 (1-21) | 1 (5.9%) | 1 (5.9%) | 0/1 (0%/5.9%) |
| Lui (1993-03) | 20 | 37.5 (16-58) | not reported | 0 | not reported | 1.3 (1-20) | 0 | 0 | 1/0 (5%/0%) |
| Murashita (1963-98) | 35 | 27.5 (6-64) | 9 (26%) | 0 | 1 (2.9%) | 16.2 ±9.4 | 2 (5.7%) | 5 (14%) | 0/1 (0%/2.9%) |
| van Son (1956-93) | 31 | 29 (3-54) | 13 (42%) | 5 (1.6%) | not reported | 25.7 (0.3-37) | 4 (13%) | 3 (9.7%) | 0/1 (0%/3.2%) |
| Wang (1988-06) | 83 | 30.7 (3-69) | 21 (25%) | 10 (8.3%) | 0 | 9.6 ±3.8 | 0 | not reported | 0/1 (0%/1.2%) |
| Yan (1980-07) | 100 | 31 (14-57) | 34 (34%) | 22 (22%) | not reported | 15.6 ±3.9 | not reported | 6 (6%) | 3/2 (3%/2%) |
| TOTAL | 741 | 30.24 (3-69) | 236/696 (34%) | 132/673 (20%) | 7/390 (1.8%) | 9 (0.1-37) | 27/641 (4.2%) | 45/658 (6.8%) | 11/24 (1.5%/3.2%) |
When taking only studies that reported the incidence of AR (n = 696 patients), the occurrence was 34% (n = 236). Of patients with AR, severity was quantified in 144 and was moderate to severe in 74%, usually owing to cusp prolapse of the affected sinus.
In the 716 patients for whom it was documented, 19% (n = 132) required concurrent aortic valve repair or replacement, typically those with moderate or severe AR. Aortic valve procedures were reserved only for those patients with concurrent severe aortic root dilation, moderate-to-severe AR, fibrotic changes of the valve, or involvement of multiple sinuses. Investigators were reticent to intervene on minor aortic valve abnormalities as repair has been shown to increase operative mortality.
Taking the 641 patients for whom the incidence of reintervention was reported, only 3.2% (n = 18) had reoperation for a recurrent aneurysm and 4.2% (n = 27) had reintervention for AR. New or progressive AR was found in 6.8% (n = 45). Several investigators noted no progression of mild AR that was not treated at the time of SOVA closure.
Surgical Repair of Ruptured SOVA
Ruptured SOVA was always repaired, even if patients were asymptomatic and only diagnosed when a continuous murmur was found on routine examination. Although its natural history is not well understood, asymptomatic, unruptured SOVA, usually found during unrelated imaging studies, was almost always repaired in larger surgical series, and documented anecdotal cases advocate for early intervention. For example, a Jehovah’s Witness with an unruptured aneurysm had refused surgery, but over the next 4 years, he developed severe AR, extension of the aneurysm to the right and left coronary sinuses, and dilatation of the aortic annulus. Vural et al proposed that patients with unruptured, stable aneurysms should be anticoagulated, followed at 6-month intervals, and then repaired if symptoms develop or the size of the sinus is >50% of the average size of the other 2 normal Valsalva sinuses, compresses or distorts surrounding chambers or tissues, or increases in consecutive echocardiographic examinations.
For the purpose of this discussion, only surgical series that investigated ruptured SOVA (n = 741, 67% men) were considered. The chambers of rupture and drainage are shown in Figure 1 . Until the use of routine 2-dimensional echocardiography, most patients were diagnosed with angiography. Several investigators report an echocardiographic accuracy rate of >90%, with the most error occurring in the accurate identification of the chamber of drainage. In the current era, angiography is typically reserved for characterization of coronary artery disease in older patients.

Of the 656 patients in whom symptoms were reported, 88% (n = 583) presented with exertional dyspnea, palpitations, fever, chest pain, fatigability, or a combination of these. Symptom onset was further characterized in 328 patients, with 36% (n = 121) of patients presenting suddenly, requiring early repair. The remaining patients were repaired electively within 2 to 4 months. New York Heart Association class was reported in 517 patients, with 52% (n = 269) presenting in class 3and 4, and mean Qp:Qs (reported in 140 patients) was 2.35 (range 1.9 to 2.9).
Investigators chose 1 of 3 accepted operative approaches to closure: through the ruptured cardiac chamber, through an aortotomy, or by a combined approach. The ruptured sites were closed directly or with prosthetic or pericardial patches. Some investigators describe a greater incidence of recurrent fistulas in patients who underwent direct closure, although others found no differences in recurrence or AR related to surgical approach, and this remains an area of contention.
Of the 741 patients ( Table 1 ), early mortality was low at 1.5% (n = 11). The range of follow-up tracking late deaths was extremely variable, from several months to 37 years. Abe and Komatsu reported a late actuarial survival rate at 25 years of 86 ± 7%. Typical causes of late death included anticoagulation-related hemorrhage, endocarditis, other organ failure, and congestive heart failure from myocardial disease. Total event-free survival has collectively improved over the last 2 decades.
| Publication (years of recruitment) | Number of patients | Age (years) | Aortic regurgitation | Aortic valve repair | New aortic regurgitation | Follow up (years) | Re-operation for aortic regurgitation | Progressive aortic regurgitation | Early/Late Death |
|---|---|---|---|---|---|---|---|---|---|
| Abe (1961-87) | 31 | 23 (3-58) | 12 (38%) | 5 (16%) | not reported | 11.1 ±7.6 | 4 (13%) | 4 (1.3%) | 1/4 (3.2%/13%) |
| Agrawal (1979-90) | 22 | 28.5 (15-45) | 8 (36%) | 5 (9%) | 0 | 5 (0.5-10) | 0 | 0 | 1/0 (4.5%/0%) |
| Au (1978-96) | 53 | 36 (13-65) | 23 (43%) | 14 (26%) | 0 | 6.5 ±4.9 | 2 (3.8%) | 1 (1.9%) | 0/5 (0%/9.4%) |
| Azakie (1970-98) | 34 | 31.6 (7-57) | 24 (70%) | 11 (32%) | not reported | 9.2 ±8.3 | 6 (18%) | 6 (1.8%) | 0/4 (0%/12%) |
| Choudhary (1977-96) | 104 | 27.5 (5-62) | 45 (43%) | 27 (26%) | 3 (2.9%) | 8.2 (1-20) | 0 | 2 (1.9%) | 2/1 (2%/2%) |
| Dong C (1996-01) | 67 | 32 (2-57) | 12 (17%) | 12 (18%) | not reported | 2.1 (0.1-4.9) | 0 | 1 (1.5%) | 1/1 (1.5%/1.5%) |
| Dong R (1997-07) | 43 | 29 (11-50) | 15 (34%) | not reported | not reported | 5.7 (1-10) | 2 (4.7%) | 2 (4.7%) | 0/0 |
| Hamid (1978-93) | 25 | 26 (11-49) | not reported | not reported | not reported | 5.5 (0.3-15) | 1 (4%) | 3 (12%) | 1/1 (4%/4%) |
| Jung (1990-06) | 56 | 33.2 (14-64) | 8 (14%) | 9 (16%) | 5 (9%) | 3.8 (0.1-15) | 4 (7.1%) | 11 (20%) | 0/2 (0%/3.6%) |
| Kirali (1985-99) | 20 | 28.3 (14-55) | 4 (20%) | 4 (20%) | 1 (5%) | 4.4 (1-13) | 1 (5%) | 0 | 1/0 (5%/0%) |
| Lin (1980-01) | 17 | 33.5 (22-59) | 8 (47%) | 8 (47%) | 0 | 11.5 (1-21) | 1 (5.9%) | 1 (5.9%) | 0/1 (0%/5.9%) |
| Lui (1993-03) | 20 | 37.5 (16-58) | not reported | 0 | not reported | 1.3 (1-20) | 0 | 0 | 1/0 (5%/0%) |
| Murashita (1963-98) | 35 | 27.5 (6-64) | 9 (26%) | 0 | 1 (2.9%) | 16.2 ±9.4 | 2 (5.7%) | 5 (14%) | 0/1 (0%/2.9%) |
| van Son (1956-93) | 31 | 29 (3-54) | 13 (42%) | 5 (1.6%) | not reported | 25.7 (0.3-37) | 4 (13%) | 3 (9.7%) | 0/1 (0%/3.2%) |
| Wang (1988-06) | 83 | 30.7 (3-69) | 21 (25%) | 10 (8.3%) | 0 | 9.6 ±3.8 | 0 | not reported | 0/1 (0%/1.2%) |
| Yan (1980-07) | 100 | 31 (14-57) | 34 (34%) | 22 (22%) | not reported | 15.6 ±3.9 | not reported | 6 (6%) | 3/2 (3%/2%) |
| TOTAL | 741 | 30.24 (3-69) | 236/696 (34%) | 132/673 (20%) | 7/390 (1.8%) | 9 (0.1-37) | 27/641 (4.2%) | 45/658 (6.8%) | 11/24 (1.5%/3.2%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


