Octogenarians affected by mitral regurgitation (MR) are an increasing high-risk population. MitraClip repair is emerging as a promising option for this kind of patients. In this retrospective study, the outcomes of patients aged ≥80 years, affected by isolated degenerative MR, who underwent isolated transcatheter (n = 25) or surgical (n = 35, 29 repairs and 6 replacements) mitral intervention from September 2008 to February 2014 were compared. MitraClip patients had higher mean age (84.5 ± 3.2 vs 81.9 ± 2.0 years, p <0.01), median Logistic Euroscore 19.4 (11.1 to 29.0) versus 8.4 (7.0 to 10.1) (p <0.01), median Society of Thoracic Surgeons predicted mortality 5.3 (3.5 to 6.6) versus 2.7 (2.3 to 3.9) (p <0.01), and more advanced New York Heart Association class (III to IV in 68% vs 37%, p = 0.02). At 30 days, 1 death occurred in the MitraClip group (p = 0.2). MitraClip was associated with significantly less complications (p <0.05) but more residual MR >2 (p <0.01). Two-year actuarial survival rate was 90% for MitraClip versus 97% for surgery (p <0.01). Higher Society of Thoracic Surgeons mortality was associated with reduced follow-up survival rate (p = 0.01). Two-year actuarial freedom from MR >2 was 70% versus 100%, respectively (p <0.01). New York Heart Association class and quality of life improved after MitraClip and were similar to surgical patients. Recurrent MR >2 was not significantly associated with follow-up mortality in this elderly setting. After the introduction of MitraClip, octogenarian patients with isolated degenerative MR receiving mitral treatment significantly increased (p <0.01). In conclusion, MitraClip patients, despite being older, more symptomatic, and affected by more co-morbidities showed significantly reduced postoperative complications. Two-year mortality was higher in the MitraClip group likely because of co-morbidities. Transcatheter mitral repair resulted in more octogenarians being treated compared with the past.
Almost one-half of patients affected by severe mitral regurgitation (MR) have not been referred to surgery in recent years, mainly because of their advanced age, co-morbidities, and left ventricular dysfunction. Transcatheter mitral technologies are emerging as a viable option to treat high-risk and inoperable patients, having shown promising early outcomes, especially in terms of procedural safety. The results of transcatheter mitral repair often include high-risk old patients ; however, data in the subset of octogenarians affected by degenerative mitral regurgitation (DMR) are still scarce and frequently unspecified. Moreover, no direct comparison with a surgical cohort has ever been conducted in this setting. This study compares outcomes between percutaneous mitral repair using the MitraClip System (Abbott Vascular, Inc., Menlo Park, California) and conventional surgical treatment (repair and replacement) in octogenarian patients affected by isolated DMR in our single-center experience.
Methods
From September 2008 to April 2014, 205 high-risk patients underwent a percutaneous mitral repair with the MitraClip System at our institution. All MitraClip patients underwent a standardized prospective screening and data collection pathway, including baseline quality of life (QoL) assessment by means of the SF-36 questionnaire and follow-up enrollment in our dedicated outpatient clinic. We retrospectively selected patients >80 years affected by isolated DMR to be compared with a similar surgical population treated during the same time frame. Indication for transcatheter mitral repair was given by the Heart Team on the basis of a high estimated surgical risk according to current guidelines. Among the baseline patient features, frailty was assessed through the eyeball test and taken into account for preoperative patient evaluation. Patients with concomitant tricuspid regurgitation >2+ were excluded to equalize as much as possible to 2 patient populations regarding the received procedure (because surgical patients with tricuspid regurgitation would receive tricuspid repair, whereas MitraClip patients could not).
Surgical patients were searched for into our departmental surgical database, selecting patients >80 years, affected by isolated DMR who underwent an isolated mitral intervention (repair or replacement) during the same time frame as the MitraClip procedures (from September 2008 to April 2014, total of 2065 screened mitral valve repair procedures). Patients with etiologies other than degenerative (functional, endocarditis, previous prosthesis malfunction or degeneration) and patients who underwent concomitant procedures were excluded. In-hospital data were retrospectively retrieved from our Institutional Database. Follow-up data were retrieved from our outpatient clinic and completed with telephone calls; all surgical patients were asked to complete the SF-36 questionnaire through telephone call.
Finally, the number of octogenarians submitted for mitral intervention (surgical or percutaneous) for a period of 5 years before and 5 years after the introduction of MitraClip therapy at our institution (September 2008) was retrospectively assessed.
MR was graded according to current European Society of Cardiology guidelines as: 1+ mild, 2+ moderate, 3+ medium, and 4+ severe. Procedural success was defined as acute MR reduction to MR ≤2. Ethics approval for the study was obtained from our Institutional Ethics Committee.
Statistical analyses were conducted using the SPSS Statistics software, v20 (IBM Corp., Armonk, New York). The distribution of variables was evaluated using the 1-sample Kolmogorov-Smirnov test. Continuous variables are presented as mean ± sample SD for data with a normal distribution or as median (25th and 75th percentile limits in brackets) for data with a non-Gaussian distribution. Categorical variables are expressed as proportions. Univariable comparisons have been performed using the unpaired t test for normally distributed data. For non-normally distributed data, Wilcoxon signed-rank test was used for paired continuous and Mann-Whitney test for unpaired continuous variables. Likelihood ratio test and Fisher’s exact test were used as appropriate for categorical data. Univariate Cox hazard model was used for follow-up mortality and recurrent MR >2+ prediction; results were tested using Wald test statistics. Hazard ratio (HR) of continuous variables are expressed as “per unit,” and numbers in brackets denote 95% confidence interval (CI). Long-term survival rate and freedom from MR >2+ were evaluated using the Kaplan-Meier curve. A 2-sided p value <0.05 was considered statistically significant.
Results
From September 2008 to February 2014, 60 octogenarians with isolated DMR underwent an isolated mitral intervention at our institution. MitraClip repair was conducted in 25 and cardiac surgery in 35 cases. In the surgical group, 29 patients underwent mitral repair and 6 patients replacement as intention to treat. Reasons for replacement were severe annular calcification in 4, previous mitral repair failure in 1 (performed in another center), and previous MitraClip failure in 1 patient (performed in another center).
Baseline clinical and echocardiographic features of the groups are listed in Table 1 . MitraClip patients were older (p <0.01), more symptomatic (p = 0.02), and had more co-morbidities, with a higher Logistic EuroScore and Society of Thoracic Surgeons (STS) score of 19.4 versus 8.4 (p <0.01) and 5.3 versus 2.7 (p <0.01), respectively.
| Variable | MitraClip (n=25) | Surgery (n=35) | p value |
|---|---|---|---|
| Age (years) | 84.5 ± 3.2 | 81.9 ± 2.0 | <0.01 |
| New York Heart Association class III-IV | 17 (68%) | 13 (37%) | 0.02 |
| Body Mass Index (Kg/m 2 ) | 22.3 ± 3.6 | 20.8 ± 4.2 | 0.18 |
| Logistic EuroScore (%) | 19.4 [11.1-29.0] | 8.4 [7.0-10.1] | <0.01 |
| Society of Thoracic Surgeons mortality (%) | 5.3 [3.5-6.6] | 2.7 [2.3-3.9] | <0.01 |
| Society of Thoracic Surgeons morbidity and mortality (%) | 25.9 ± 10.0 | 18.7 ± 5.8 | <0.01 |
| Previous cardiac surgery | 3 (12%) | 2 (6%) | 0.38 |
| Coronary Artery Disease | 7 (28%) | 7 (20%) | 0.47 |
| Serum creatinine (mg/dL) | 1.2 ± 0.4 | 1.0 ± 0.3 | 0.03 |
| Glomerular Filtration Rate (ml/min) | 46.7 ± 16.0 | 54.9 ± 19.8 | 0.04 |
| Chronic Kidney Disease | 19 (76%) | 20 (57%) | 0.13 |
| Chronic Obstructive Pulmonary Disease | 6 (24%) | 3 (9%) | 0.09 |
| Cerebro Vascular Disease | 6 (24%) | 3 (9%) | 0.09 |
| Atrial Fibrillation | 10 (40%) | 7 (20%) | 0.09 |
| Echocardiography | |||
| Left Ventricle End Diastolic Diameter (mm) | 56.1 ± 6.5 | 55.0 ± 5.9 | 0.54 |
| Left Ventricle Ejection Fraction (%) | 59.8 ± 9.9 | 61.1 ± 8.0 | 0.60 |
| systolic Pulmonary Artery Pressure (mmHg) | 49 ± 12 | 42 ± 13 | 0.07 |
| Anterior leaflet | 6 (24%) | 1 (3%) | 0.01 |
| Bileaflet | 1 (4%) | 7 (20%) | 0.07 |
| Calcific annulus | 2 (8%) | 10 (29%) | 0.04 |
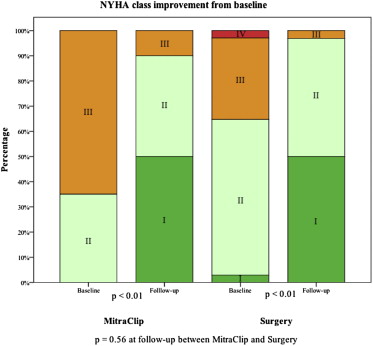
No procedural death occurred in either group; 1 conversion to surgery was needed in the MitraClip group because of entanglement of the clip into the mitral subvalvular apparatus. In the surgical group, 2 patients required a second pump run because residual MR (both receiving a successful repair revision) and 1 case required replacement because of leaflet fibrosis. Therefore, in the 54 patients, overall submitted to mitral repair (percutaneous and surgical), MR was immediately effectively reduced to ≤2+ in 22 (88%) patients after MitraClip and in 28 (97%) after surgical repair ( Figure 1 , p <0.01). Another surgical patient required a second pump run because of aortic wall rupture at the site of cannulation. In the replacement subgroup, 1 case of bleeding from the atrioventricular groove required multiple blood transfusion and prolonged hemostasis. Good prosthesis function without any paravalvular leak and MR was observed in all patients.
At 30 days, 1 death occurred in the MitraClip group in the patient who had required the conversion to surgery (p = 0.23 vs surgery); further postoperative in-hospital outcomes are listed in Table 2 .
| Variable | MitraClip (n=25) | Surgery (n=35) | p value |
|---|---|---|---|
| Death | 1 (4%) | 0 (0%) | 0.23 |
| Low Cardiac Output Syndrome | 1 (4%) | 13 (37%) | <0.01 |
| Acute Kidney Failure | 3 (12%) | 18 (51%) | <0.01 |
| Transfusions | 3 (12%) | 17 (48%) | <0.01 |
| New Atrial Fibrillation | 2 (8%) | 13 (37%) | 0.01 |
| Stroke | 0 (0%) | 0 (0%) | – |
| Transient neurological dysfunction | 0 (0%) | 3 (9%) | 0.13 |
| Prolonged respiratory support | 1 (4%) | 7 (20%) | 0.07 |
| Intensive Care Unit Length of Stay (days) | 1.4 ± 1.6 | 2.8 ± 3.6 | 0.04 |
| Post-operative Length of Stay (days) | 4.9 ± 1.8 | 10.6 ± 6.9 | <0.01 |
| Home discharge | 22 (88%) | 0 (0%) | <0.01 |
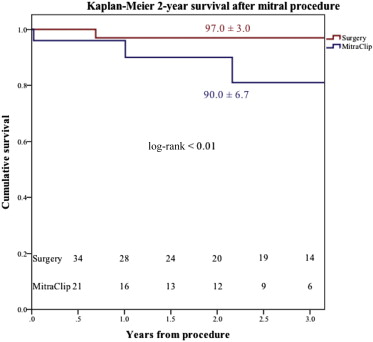
Follow-up was 100% complete, with a mean follow-up time of 1.8 ± 1.3 years for MitraClip versus 2.5 ± 1.5 years for surgery (p = 0.06). Actuarial survival rate at 2 years was 90.0 ± 6.7% for MitraClip versus 97.0 ± 3.0% for surgery, p <0.01 ( Figure 2 ). Five deaths occurred after the first 30 days, 1 of which was cardiac related; causes of death in the remaining patients were 2 strokes, 1 pneumonia, and 1 bleeding after major trauma. At univariable Cox regression, transcatheter mitral repair (HR 12.6, CI 1.4 to 112.7, p = 0.02) and baseline STS predicted mortality (HR 1.3, CI 1.1 to 1.7, p = 0.01) were found to be the only predictors of increased follow-up mortality. Acute residual MR (p = 0.27) and follow-up recurrent MR (p = 0.33) were not significantly associated with increased follow-up mortality.
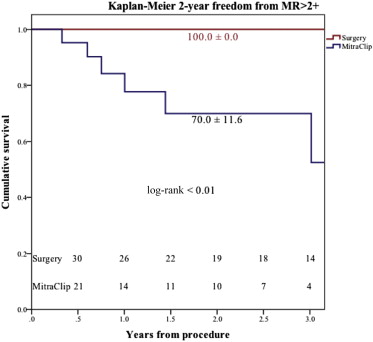
Overall actuarial freedom from MR >2 at 2 years was 70.0 ± 11.6% for MitraClip versus 100.0 ± 0.0% for surgery, p <0.01 ( Figure 3 ). In the MitraClip group, 2 partial clip detachments occurred (7.3 and 11.9 months after the procedure); no patient underwent mitral surgery or re-MitraClip. In patients who underwent mitral repair (percutaneous or surgical) and who had residual MR ≤2 at discharge (n = 50), no significant predictive factor for MR >2 recurrence was found except for the degree of acute residual MR (p = 0.02). All implanted mitral prostheses showed good function without signs of degeneration or paravalvular leak.
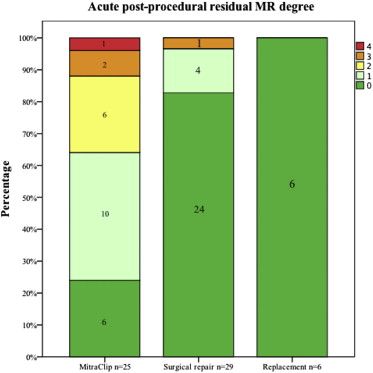
At last follow-up, New York Heart Association (NYHA) class improved compared with baseline both after MitraClip (p <0.01, NYHA >II in 2 [10%] patients) and after surgery (p <0.01, NYHA >II in 1 [3%] patient) and was similar between the 2 groups (p = 0.56, Figure 4 ). In the MitraClip group, the SF-36 Physical score significantly increased from mean 38.2 ± 6.5 to 45.1 ± 4.5 (p <0.01), whereas the increase in SF-36 Mental score was not significant compared with baseline (from mean 44.2 ± 8.9 to 49.4 ± 4.7, p = 0.07). SF-36 baseline data were not available for surgical candidates; however, at last follow-up, the surgical Physical (45.7 ± 5.7) and Mental (47.2 ± 7.6) scores were similar compared with those of MitraClip patients, respectively, p = 0.70 and p = 0.30. In MitraClip patients with recurrent MR >2, NYHA class I, II, to III were observed, respectively, in 0 (0%), 3 (75%), and 1 (25%) patient versus 10 (62%), 5 (31%), and 1 (6%) patient without MR >2, p = 0.07. Mean Physical SF-36 score was 42.0 versus 46.2 (p = 0.12) and mean SF-36 Mental score was 45.7 versus 50.7 (p = 0.06), respectively, in patients with and without follow-up MR >2.