Coronary artery disease negatively affects the outcome of patients undergoing surgical aortic valve replacement and practice guidelines recommend revascularization at time of surgery. In patients undergoing transcatheter aortic valve implantation (TAVI), the impact of preprocedural percutaneous coronary intervention (PCI) on TAVI outcome has not been examined. We aimed in the present study to assess the feasibility and safety of performing PCI before TAVI and to evaluate procedural, 30-day, and 6-month clinical outcomes. We retrospectively analyzed 125 patients who underwent successful TAVI at a single institution and divided them into an isolated TAVI and a PCI + TAVI group. During the study period, a strategy of preprocedural PCI of all significant (>50%) lesions in major epicardial vessels was adopted. Study end points were adjudicated in accordance with the Valve Academic Research Consortium consensus on event definition. All patients were treated with the Medtronic CoreValve prosthesis (n = 55 with PCI + TAVI and n = 70 with isolated TAVI). Thirty-day mortality was 2% versus 6% for patients treated with PCI + TAVI versus isolated TAVI, respectively (p = 0.27). Neither periprocedural nor spontaneous myocardial infarction occurred in either group. Rates of 30-day stroke, major bleeding, major vascular complications, and the Valve Academic Research Consortium–defined combined safety end point (11% vs 13%, p = 0.74) did not differ between the 2 groups. Patients’ symptoms significantly improved in the first month after TAVI, and extent of improvement did not differ between groups. Adverse events at 6 months were comparable. In conclusion, PCI before TAVI appears feasible and safe. Based on these early results revascularization should become an important consideration in patients with coronary artery disease undergoing TAVI.
Transcatheter aortic valve implantation (TAVI) has recently emerged as a promising treatment method for patients with severe symptomatic aortic stenosis with high or prohibitive surgical risk. The presence of concomitant coronary artery disease (CAD) might have a negative impact on the safety of TAVI, and concerns about access to coronary arteries after TAVI argue for percutaneous coronary intervention (PCI) before TAVI. However, the impact of PCI before TAVI on the outcome of patients undergoing TAVI has not been examined, and there is no settled consensus about how these patients should be managed. Therefore, we aimed in the present study to assess the feasibility and safety of performing PCI before TAVI and to evaluate procedural, 30-day, and 6-month clinical outcomes in a consecutive series of patients at a single institution.
Methods
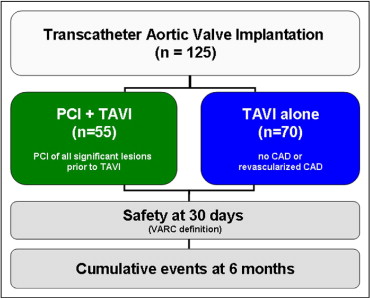
From September 2007 through March 2011, 129 consecutive patients with severe symptomatic aortic stenosis (aortic valve area <1.0 cm 2 or body surface area–indexed aortic valve area <0.6 cm 2 /m 2 ) were treated with TAVI at our institution. Surgical aortic valve replacement (SAVR) was not performed by a cardiac surgeon based on high morbidity and mortality scores (≥80 years of age and logistic European System for Cardiac Operative Risk Evaluation score ≥20% or logistic European System for Cardiac Operative Risk Evaluation score <20% in the presence of liver cirrhosis, chronic pulmonary disease, or porcelain aorta) or after discussing patients’ data within the institutional heart team. During this period a strategy of preprocedural percutaneous revascularization of all significant (>50%) lesions in the major epicardial coronary vessels was adopted. In 4 patients the valve could not be implanted in the proper anatomic position and these patients were excluded from analysis. Thus, the present study is based on 125 patients who were retrospectively divided into 2 groups; the first group included patients who underwent PCI before or combined with TAVI (PCI + TAVI group) and the second group included patients with no significant or previously revascularized CAD who underwent only TAVI (isolated TAVI group; Figure 1 ) .
A full laboratory assessment including cardiac markers of necrosis was performed before and immediately after TAVI and at 30 days and 6 months. Baseline transthoracic echocardiography and transesophageal echocardiography were performed in all patients, as were routine coronary angiography, right heart catheterization, and peripheral angiography. Transthoracic echocardiography was repeated after the procedure and at 30 days and 6 months. Clinical events were recorded for the in-hospital period, at 30 days, 6 months, and yearly thereafter.
Percutaneous revascularization was done in the preparatory stage before proceeding to TAVI (up to 3 months provided that TAVI was already planned at time of PCI) or as a combined procedure and was performed transfemorally. Patients were preloaded with clopidogrel 600 mg and intravenous aspirin 500 mg immediately before intervention and continued on aspirin indefinitely and on clopidogrel 75 mg for 6 months after TAVI. Patients with an indication for oral anticoagulation received a combination of an oral vitamin K antagonist and clopidogrel (no aspirin). During PCI patients received unfractionated heparin guided by the activated clotting time. Drug-eluting stents were used unless contraindicated. The femoral artery puncture site was closed using the Starclose vascular closure device (Abbott Vascular, Abbott Park, Illinois) at the end of the PCI procedure unless the 2 procedures were performed in combination.
After informed consent TAVI using the CoreValve bioprosthesis (Medtronic, Inc., Minneapolis, Minnesota) through the transfemoral route was performed (1 patient underwent TAVI through the trans-subclavian route). Description of the valve and a review of the implantation technique have been described elsewhere. Clinical and anatomic selection criteria and device size selection were in line with the published investigational study for the third-generation (18f) CoreValve device. Selection of the prosthetic valve size was based on measurements of aortic valve annulus diameter obtained by transesophageal echocardiography. Femoral artery puncture site was closed using the Progilde vascular closure device (Abbott Vascular) at the end of the TAVI procedure.
Baseline clinical, echocardiographic, and procedural characteristics (for TAVI and PCI) were prospectively recorded for all enrolled patients and entered into an institutional database. Thirty-day and 6-month clinical assessments and transthoracic echocardiographic and laboratory evaluations were routinely performed at our institution. Thirty-day outcomes were adjudicated in accordance with the Valve Academic Research Consortium (VARC) consensus on event definition. Cardiovascular mortality was defined as any death from a proximate cardiac cause, nonwitnessed death, death of unknown cause, or procedure-related death. Periprocedural myocardial infarction (<72 hours after index procedure) was defined as new ischemic symptoms or new ischemic signs with increased cardiac biomarkers (creatine kinase-MB) within 72 hours after the index procedure. Spontaneous myocardial infarction (>72 hours after index procedure) was defined as an increase of cardiac biomarkers (troponin) and evidence of myocardial ischemia with ≥1 of the following: electrocardiographic changes indicative of new ischemia (new ST-T changes, new left bundle branch block, or new pathologic Q waves in ≥2 contiguous leads), imaging evidence of new loss of viable myocardium, or a new wall motion abnormality. Sudden unexpected cardiac death involving cardiac arrest with symptoms suggestive of myocardial ischemia and accompanied by presumably new ST-segment elevation or new left bundle branch block and/or evidence of fresh thrombus by coronary angiography and/or at autopsy examination was also defined as spontaneous myocardial infarction according to the VARC. The combined safety end point at 30 days included all-cause mortality, major stroke, life-threatening (or disabling) bleeding, stage 3 acute kidney injury (including renal replacement therapy), periprocedural myocardial infarction, major vascular complication, and repeat procedure for valve-related dysfunction (surgical or interventional therapy). Other end points are defined in detail elsewhere.
Results are reported according to the adopted treatment strategy (PCI + TAVI vs isolated TAVI). Continuous variables are expressed as mean ± SD or median and interquartile range and were analyzed with Student’s t test or Mann–Whitney test, as appropriate. Discrete variables are presented as count and percentage and were analyzed by Pearson chi-square or Fisher’s exact test, as appropriate. Kaplan–Meier survival plots were constructed from index procedure up to 3 years of follow-up and compared using log-rank test. A p value <0.05 was deemed statistically significant. Statistical analysis was performed using SPSS 13.0 for Windows (SPSS, Inc., Chicago, Illinois).
Results
Of 125 patients treated with TAVI, 55 patients received PCI before TAVI (PCI + TAVI group) and 70 patients were treated with isolated TAVI. Most baseline clinical characteristics were comparable between groups. Men constituted 47% of patients in the PCI + TAVI group compared to 49% in the isolated TAVI group (p = 0.89) and diabetes mellitus was prevalent in 33% versus 20% (p = 0.11). Overall, 91 patients (73%) had CAD. In the isolated TAVI group 51% of patients had a history of CAD; 33% had previous PCI and 23% had previous coronary artery bypass grafting. Patients who underwent PCI plus TAVI were more symptomatic at baseline, with a larger percentage with Canadian Cardiovascular Society class III/IV angina (21% vs 8%, p = 0.1) and a significantly larger percentage with New York Heart Association class IV dyspnea (36% vs 16%, p = 0.008) at presentation. Baseline clinical and angiographic data are presented in Table 1 .
| Variable | PCI + TAVI (n = 55) | Isolated TAVI (n = 70) | p Value |
|---|---|---|---|
| Age (years) | 81 ± 7.06 | 81 ± 6.20 | 0.99 |
| Men | 26 (47%) | 34 (49%) | 0.89 |
| Weight (kg) | 78.84 ± 16.64 | 75.17 ± 13.51 | 0.18 |
| Height (cm) | 168.51 ± 8.59 | 167.87 ± 8.55 | 0.68 |
| Body mass index (kg/m 2 ) | 27.87 ± 6.52 | 26.40 ± 4.27 | 0.13 |
| Diabetes mellitus | 18 (33%) | 14 (20%) | 0.11 |
| Hypertension | 46 (84%) | 56 (80%) | 0.6 |
| Dyslipidemia | 39 (71%) | 42 (60%) | 0.21 |
| Peripheral vascular disease | 11 (20%) | 10 (14%) | 0.4 |
| Carotid disease | 9 (16%) | 12 (17%) | 0.91 |
| Previous stroke | 4 (7%) | 9 (13%) | 0.31 |
| Logistic EuroSCORE (%) | 25.08 ± 12.58 | 23.62 ± 15.10 | 0.56 |
| Coronary artery disease ⁎ | 55 (100%) | 36 (51%) | <0.0001 |
| Number of diseased coronary arteries | |||
| 1 | 15 (27%) | 9 (13%) | |
| 2 | 26 (47%) | 6 (8%) | |
| 3 | 14 (26%) | 21 (30%) | |
| Previous myocardial infarction | 14 (26%) | 18 (26%) | 0.97 |
| Previous percutaneous coronary intervention | 15 (27%) | 23 (33%) | 0.5 |
| Previous coronary bypass surgery | 8 (15%) | 16 (23%) | 0.24 |
⁎ Defined as presence of lesions with ≥50% diameter stenosis on angiogram before transcatheter aortic valve implantation and/or previous myocardial infarction, percutaneous coronary intervention, or bypass surgery.
Most baseline echocardiographic characteristics were similar in the 2 groups. Significant baseline aortic regurgitation was higher in patients who underwent isolated TAVI (9%), whereas no patients in the PCI + TAVI cohort had a baseline aortic regurgitation higher than grade 2. Other echocardiographic data are presented in Table 2 .
| Variable | PCI + TAVI (n = 55) | Isolated TAVI (n = 70) | p Value |
|---|---|---|---|
| Ejection fraction (%) | 46.92 ± 13.85 | 48.54 ± 15.25 | 0.55 |
| Aortic valve area (cm 2 ) | 0.68 ± 0.20 | 0.69 ± 0.21 | 0.75 |
| Indexed aortic valve area (cm 2 /m 2 ) | 0.36 ± 0.11 | 0.38 ± 0.12 | 0.38 |
| Mean pressure gradient (mm Hg) | 49.88 ± 13.74 | 50.32 ± 16.90 | 0.88 |
| Peak pressure gradient (mm Hg) | 77.00 ± 19.85 | 78.54 ± 26.14 | 0.74 |
| Aortic regurgitation | 0.03 | ||
| 0 | 13 (24%) | 23 (33%) | |
| 1 | 38 (69%) | 34 (49%) | |
| 2 | 4 (7%) | 7 (10%) | |
| >2 | 0 (0%) | 6 (8%) | |
| Mitral regurgitation | 0.55 | ||
| 0 | 9 (16%) | 10 (14%) | |
| 1 | 34 (62%) | 38 (54%) | |
| 2 | 11 (20%) | 18 (26%) | |
| 3 | 1 (2%) | 4 (6%) | |
| Systolic pulmonary artery pressure (mm Hg) | 46.81 ± 16.93 | 46.72 ± 14.12 | 0.98 |
Median duration from PCI to TAVI was 10 days (range 0 to 90); only 3 patients had PCI at the time of TAVI. Thirty-nine patients (71%) of those who underwent PCI before TAVI received drug-eluting stents, 13 patients (24%) received bare-metal stents, and only 3 patients (5%) were treated with drug-eluting and bare-metal stents. No valve-related complications (low cardiac output, pulmonary edema, or need for urgent valvular intervention) occurred during PCI. Only 1 patient underwent TAVI through the trans-subclavian approach; all other patients underwent TAVI through the transfemoral route. Procedural time for TAVI was similar in the 2 groups, namely 71.3 ± 23.3 minutes in patients who underwent PCI compared to 69.7 ± 25.0 minutes in the other group. Further procedural details are listed in Table 3 .
| Stents/patient | 2.04 ± 1.37 |
| Minimal stent diameter (mm) | 2.91 ± 0.41 |
| Total stent length (mm) | 30.89 ± 22.68 |
| Target vessel | |
| Left main coronary artery | 7 (9%) |
| Left anterior descending coronary artery | 24 (30%) |
| Left circumflex coronary artery | 22 (28%) |
| Right coronary artery | 20 (25%) |
| Vein graft | 6 (8%) |
| 26-mm inflow CoreValve device | 22 (40%) |
| Operative time for transcatheter aortic valve implantation (minutes) ⁎ | 71.3 ± 23.3 |
Thirty-day follow-up data were available for 100% of patients. Overall, all VARC-adjudicated end points did not differ between the patient cohorts. Thirty-day all-cause mortality was 2% versus 6% for patients treated with PCI plus TAVI versus isolated TAVI, respectively (p = 0.27). Neither periprocedural nor spontaneous myocardial infarction occurred in either group. Rates of 30-day stroke (2% vs 6%, p = 0.27), life-threatening bleeding (7% vs 6%, p = 0.72), and major vascular complications (6% vs 3%, p = 0.46) did not differ significantly between the 2 groups. The VARC-defined combined safety end point did not differ between the 2 groups (11% vs 13% for patients treated with PCI plus TAVI vs isolated TAVI, respectively, p = 0.74). In contradiction to baseline symptom status, symptoms according to Canadian Cardiovascular Society and New York Heart Association classes did not differ between the 2 groups ( Figures 2 and 3 ) . Thirty-day outcomes are listed in Table 4 .




