Anemia is common in hospitalized cardiac patients and is associated with adverse outcomes. The aim of this study was to identify the association of anemia with early and long-term outcomes in patients with acute coronary syndromes (ACSs). Included were 5,304 consecutive patients (73% men, 61 ± 12 years of age) admitted to a coronary care unit from 1985 through 2008 for ACS. According to the World Health Organization, anemia was defined as serum hemoglobin levels <13 g/dl for men and <12 g/dl for women. Anemia was divided into tertiles to compare mild, moderate, and severe anemia to nonanemia. For trend analyses the study population was categorized in 3 groups: 1985 to 1990, 1991 to 2000, and 2001 to 2008. Outcome measurements were all-cause mortality at 30-days and 20 years. Anemia was present in 2,016 patients (38%), of whom 655 had mild anemia, 717 moderate anemia, and 646 severe anemia. Median follow-up duration was 10 years (range 2 to 25). Compared to nonanemia, adjusted hazard ratios (HRs) for mortality at 30 days were 1.40 for moderate anemia (95% confidence interval [CI] 1.04 to 1.87) and 1.67 for severe anemia (95% CI 1.25 to 2.24). At 20 years HRs were 1.13 for moderate anemia (95% CI 1.01 to 1.27) and 1.39 for severe anemia (95% CI 1.23 to 1.56). In addition, survival during hospitalization improved over time. Compared to 1985 to 1990 adjusted HRs were 0.52 for 1991 to 2000 (95% CI 0.41 to 0.66) and 0.36 for 2001 to 2008 (95% CI 0.25 to 0.51). In conclusion, presence and severity of anemia is an important predictor of higher in-hospital and long-term mortality after ACS. In addition, since the 1980s in-hospital outcome of patients with ACS and anemia has improved.
Anemia is common in patients hospitalized for acute coronary syndromes (ACSs) and its prevalence ranges from 6.4% to 45%. It is associated with adverse outcomes during hospitalization. Although adverse outcomes in other populations owing to anemia have been described, only a very few studies have examined the long-term effects of anemia in ST-segment elevation myocardial infarction (STEMI) and nothing is yet known of whether this association has changed over the previous 25 years. In previous decades new therapeutic and medical treatment interventions were introduced that decreased morbidity and increased survival after acute MI. These strategies include the use of reperfusion therapy, antiplatelet agents, angiotensin-converting enzyme inhibitors, and β blockers. Furthermore, percutaneous coronary intervention (PCI) became the therapeutic procedure of first choice in patients with STEMI. The effect of anemia in these patients has not been studied yet. Therefore, the main goal of this study was to identify the association of anemia with early and long-term outcomes in a cohort of patients with ACS hospitalized from 1985 through 2008 and whether this association was independent of renal insufficiency.
Methods
All patients >18 years of age admitted with a first admission for STEMI or non-STEMI (NSTEMI) in the coronary care unit of the Thoraxcenter, Erasmus University Medical Center from January 1985 through December 2008 from whom the first hemoglobin value was obtained were included.
The primary discharge diagnosis of STEMI was made in the presence of the following characteristics: chest pain or equivalent symptoms in combination with dynamic electrocardiographic changes consistent with MI and a serial increase and decrease in serum biochemical markers of cardiac necrosis such as creatine kinase-MB and troponin T. Patients were diagnosed as having STEMI in the presence of STE >0.1 mV in ≥2 extremity leads or >0.2 mV in ≥2 precordial leads; otherwise NSTEMI was diagnosed.
Data were acquired retrospectively by retrieving hospital medical records. Demographic characteristics (age, gender), cardiac history (previous MI, PCI, or coronary artery bypass grafting), risk factors (hypertension, diabetes, hypercholesterolemia, family history, smoking status, renal dysfunction), discharge diagnosis (STEMI or NSTEMI), and therapy (PCI, antithrombotic treatment) were collected.
The primary end point was mortality at 30 days and at 20-year follow-up. Survival status was assessed through municipal civil registries.
Hemoglobin value was determined on first admission. We adopted the definition of anemia by the World Health Organization, which defines anemia as a serum hemoglobin level <13 g/dl for men and a level <12 g/dl for women. Patients with anemia were divided into tertiles to compare the prognosis of patients with mild (12.2 to 13.0 g/dl in men, 11.2 to 12.0 g/dl in women), moderate (10.9 to 12.1 g/dl in men, 10.3 to 11.1 g/dl in women), and severe (≤10.8 g/dl in men, ≤10.2 g/dl in women) anemia to that of subjects without anemia.
Patients’ characteristics were presented as mean ± SD for continuous variables and compared by 1-way analysis of variance and Bonferroni correction. Pearson chi-square test was used for categorical variables, which were presented as percentage. Cumulative survival was constructed using the Kaplan–Meier method. Log-rank tests were used to compare curves. Logistic regression analyses were performed to adjust anemia for other baseline characters of 30-day outcome. Cox regression analyses were performed to identify 20-year outcome. Adjustments were made for the variables age, gender, hypertension, diabetes, renal insufficiency defined as a creatinine value >150 mmol/L, hypercholesterolemia, smoking status, clinical presentation, treatment, previous coronary artery bypass grafting, previous MI, previous percutaneous transluminal coronary angioplasty, and trends. Results are reported as hazard ratios (HRs) of mortality and their respective 95% confidence intervals (CIs). All statistical tests were 2-tailed, and p values were statistically significant at <0.05. When analyzing for trends, the study population was categorized in 3 groups of patients hospitalized from 1985 to 1990, 1991 to 2000, and 2001 to 2008. Furthermore, when analyzing for trends, we tried to find a possible interaction with anemia or renal insufficiency. All data were analyzed with SPSS 17.0 (SPSS, Inc., Chicago, Illinois).
Results
Of the 5,304 patients included in the study, 73% were men. Mean age was 61 years. In total 38% of patients were anemic. When this last group was divided in tertiles, 655 had mild anemia (12.3%), 717 moderate anemia (13.5%), and 646 severe anemia (12.2%). Mean hemoglobin levels were 14.2 ± 1.2 g/dl in nonanemic patients and 11.0 ± 1.6 g/dl in patients with anemia.
Patients with anemia were more likely to be older, have more co-morbidities, and more often treated with cardiac medication ( Table 1 ). Furthermore, patients with anemia received less additional therapy at admission. Prevalence of mild anemia increased from 8.5% in 1985 to 1990 to 12.6% in 1991 to 2000 and to 16.0% in 2001 to 2008 (p <0.001). Prevalence of moderate anemia increased from 10.2% in 1985 to 1990 to 14.2% in 1991 to 2000 and to 15.6% in 2001 to 2008 (p <0.001). Prevalence of severe anemia increased from 10.5% in 1985 to 1990 to 13.3% in 1991 to 2000 and to 11.8% in 2001 to 2008 (p <0.05).
| Variable | Nonanemia | Mild Anemia | Moderate Anemia | Severe Anemia | p Value |
|---|---|---|---|---|---|
| (n = 3,288, 61.9%) | (n = 655, 12.3%) | (n = 715, 13.5%) | (n = 646, 12.2%) | ||
| Age (years), mean ± SD | 60 ± 12.0 | 63 ± 11.6 | 64 ± 11.3 | 65 ± 11.8 | <0.001 |
| Men | 76% | 65% | 72% | 68% | <0.001 |
| Diabetes mellitus | 11% | 12% | 14% | 16% | 0.001 |
| Hypertension | 33% | 32% | 35% | 40% | 0.01 |
| Hypercholesterolemia | 29% | 21% | 22% | 22% | 0.2 |
| Smoking | 40% | 33% | 31% | 25% | <0.001 |
| Family history | 27% | 24% | 23% | 20% | <0.001 |
| Renal insufficiency | 4% | 6% | 14% | 27% | <0.001 |
| Previous myocardial infarction | 29% | 34% | 34% | 36% | <0.001 |
| Previous percutaneous coronary intervention | 8% | 9% | 11% | 10% | 0.1 |
| Previous coronary artery bypass grafting | 8% | 8% | 9% | 8% | 0.6 |
| Arrhythmia | 1.7% | 2.6% | 2.7% | 3.4% | 0.02 |
| Clinical presentation | 0.1 | ||||
| ST-segment elevation myocardial infarction | 53% | 50% | 49% | 49% | |
| Non–ST-segment elevation myocardial infarction | 47% | 50% | 51% | 51% | |
| Medication | |||||
| Aspirin | 54% | 57% | 56% | 51% | 0.05 |
| Angiotensin-converting enzyme inhibitor | 20% | 19% | 21% | 22% | 0.5 |
| Antiarrhythmics | 5% | 6% | 7% | 9% | 0.004 |
| β Blocker | 64% | 60% | 56% | 52% | <0.001 |
| Calcium antagonist | 33% | 34% | 35% | 33% | 0.7 |
| Digitalis | 5% | 6% | 7% | 8% | 0.01 |
| Diuretics | 16% | 18% | 21% | 25% | <0.001 |
| Oral anticoagulant | 57% | 57% | 56% | 51% | 0.03 |
| Treatment | <0.001 | ||||
| Percutaneous coronary intervention | 35% | 43% | 42% | 36% | |
| Antithrombotic treatment | 16% | 15% | 12% | 9% | |
| None | 49% | 41% | 45% | 55% |
In the total study population mean follow-up duration was 10 years (range 2 to 25). Overall cumulative survivals were 91% at 30 days and 49% at 20 years. Cumulative 30-day survivals were 93% in nonanemic patients and 88% in anemic patients (p <0.001; Figure 1 ) . Cumulative 30-day survival rate in patients with anemia increased from 87.2% in 1985 to 1990 to 91.3% in 1991 to 2000 (p = 0.002) and to 94.1% in 2001 to 2008 (p <0.001; Figure 2 ) .
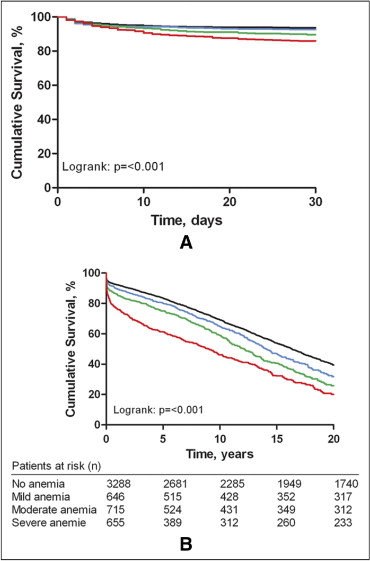
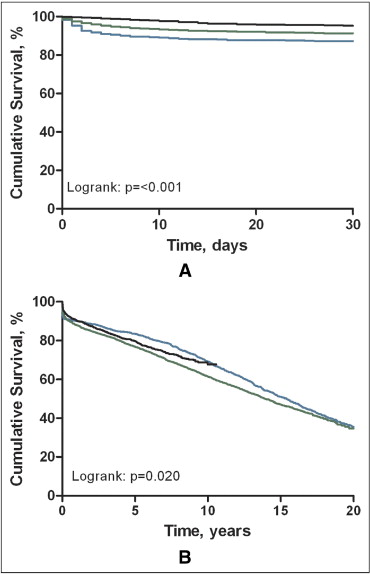
Cumulative 20-year survivals were 52.9% for nonanemic patients and 42.8% for anemic patients (p <0.001; Figure 1 ). The difference was predominant in the first year. Thereafter, the curves were parallel. Over time, cumulative 20-year survival rate was 33.8% in 1985 to 1990, which decreased to 33.7% in 1991 to 2000 ( Figure 2 ). In addition, cumulative 10-year survival was 66.8% in 2001 to 2008 ( Figure 2 ).
After adjusting for baseline characteristics including renal insufficiency, moderate and severe anemias were associated with an increased risk of 30 day-mortality (adjusted HR 1.40, 95% CI 1.04 to 1.87; adjusted HR 1.67, 95% CI 1.25 to 2.24; Table 2 ).
| Univariate | Multivariate ⁎ | |
|---|---|---|
| HR (95% CI) | HR (95% CI) | |
| Nonanemia | Reference | Reference |
| Mild anemia | 0.82 (0.60–1.11) | 0.99 (0.71–1.39) |
| Moderate anemia | 1.40 (1.09–1.80) | 1.40 (1.04–1.87) |
| Severe anemia | 2.16 (1.71–2.73) | 1.67 (1.25–2.24) |
| Renal insufficiency | 3.31 (2.96–3.70) | 4.11 (3.14–5.38) |
| 1985–1990 | Reference | Reference |
| 1990–2000 | 1.10 (1.02–1.18) | 0.52 (0.41–0.66) |
| 2000–2008 | 0.86 (0.77–0.97) | 0.36 (0.25–0.51) |
⁎ Adjusted for age, gender, hypertension, diabetes mellitus, hypercholesterolemia, smoking, previous myocardial infarction, percutaneous coronary intervention, coronary artery bypass grafting, renal insufficiency, and trends and tertiles of anemia.
Hospital mortality during the 1990s and 2000s was lower than in the 1980s (adjusted HR 0.52, 95% CI 0.41 to 0.66; adjusted HR 0.36, 95% CI 0.25 to 0.51).
For long-term outcome, moderate and severe anemias were associated with higher mortality (adjusted HR 1.13, 95% CI 1.01 to 1.27; adjusted HR 1.39, 95% CI 1.23 to 1.56) despite the effect of predictor renal insufficiency on mortality (HR 2.28, 95% CI 2.02 to 2.57; Table 3 ).



