Available data suggest that thrombolytic therapy facilitated percutaneous coronary intervention (FPCI) is not beneficial, and recent analyses have shown a correlation between mortality risk and outcomes of patients with ST elevation myocardial infarctions treated with FPCI. The aim of this study was to analyze the impact of the mortality risk on the survival benefit of primary percutaneous coronary intervention (PPCI) compared to FPCI. A total of 13 trials enrolling 5,789 patients were pooled for analyses. PPCI survival benefit was calculated as the 30-day mortality after FPCI minus the 30-day mortality after PPCI, and the mortality rate of FPCI was interpreted as a proxy for mortality risk. A weighted metaregression was used to test the relation between mortality risk and explanatory variables. A fixed-effect linear regression analysis modeling the log odds ratio (PPCI/FPCI) as a linear function of the log odds of FPCI mortality was used to estimate the mortality risk that nullified the 30-day survival benefit of PPCI over FPCI. Across all studies, the absolute survival benefit ranged from −5.6 (favoring FPCI) to +7.2 (favoring PPCI). According to the slope of the regression line (−0.7, x-axis intercept −2.1) for the patients with baseline mortality risk > 4.2%, it is unlikely to obtain a survival benefit by FPCI compared to PPCI. In conclusion, the higher the mortality risk of patients with ST elevation myocardial infarctions, the higher the likelihood of a survival advantage of PPCI over FPCI.
Recent post hoc analyses of the Facilitated Intervention With Enhanced Reperfusion Speed to Stop Events` (FINESSE) trial have shown a favorable interaction between risk and the outcomes of patients with ST elevation myocardial infarctions (STEMIs) treated with facilitated percutaneous coronary intervention (FPCI). In contrast, a recent subanalysis of the Assessment of the Safety and Efficacy of a New Treatment Strategy with Percutaneous Coronary Intervention (ASSENT-4) study showed the benefit of FPCI in case of short prehospital delays, but not in high-risk patients. Thus, we aimed in the present study to analyze whether mortality risk affects the survival benefit of primary percutaneous coronary intervention (PPCI) compared to FPCI.
Methods
We identified all randomized trials, published and unpublished, comparing PPCI to FPCI that enrolled ≥50 patients. Electronic databases (Medline, Central, Embase, the Cochrane Central Register of Controlled Trials [ http://www.mrw.interscience.wiley.com/cochrane/cochrane_clcentral_articles_fs.html ], and http://www.clinicaltrialresults.org ) were used to identify randomized controlled trials published from January 1990 to December 2009 using a broad range of key words, including “(acute) myocardial infarction,” “fibrinolytic”, “thrombolytic”, “accelerated tissue plasminogen activator,” “t-PA,” “rt-PA,” “facilitated,” “primary,” “angioplasty,” “stent,” “percutaneous coronary intervention (PCI),” “reperfusion,” and “randomized.” We also searched for abstracts of scientific sessions reported in the New England Journal of Medicine , Circulation , the European Heart Journal , the Journal of the American College of Cardiology , Heart , the American Journal of Cardiology , and the American Heart Journal . Reference lists of the identified reports, relevant studies, and meta-analyses were scanned. Furthermore, oral presentations and/or expert slide presentations identified at http://www.theheart.org , http://www.tctmd.com , http://www.crtonline.com , http://www.clinicaltrialresults.org , http://www.esccardio.org , http://www.europcr.com , and http://www.acc.org were examined. Non-English-language reports were not excluded. Each trial identified through this search was then critically and independently evaluated by 2 investigators (GT, MF) for patient population, study treatment, protocol, and end point selection for data extraction and inclusion into the final analysis. Divergences were resolved by consensus. The flowchart of the trial selection process is shown in Figure 1 .
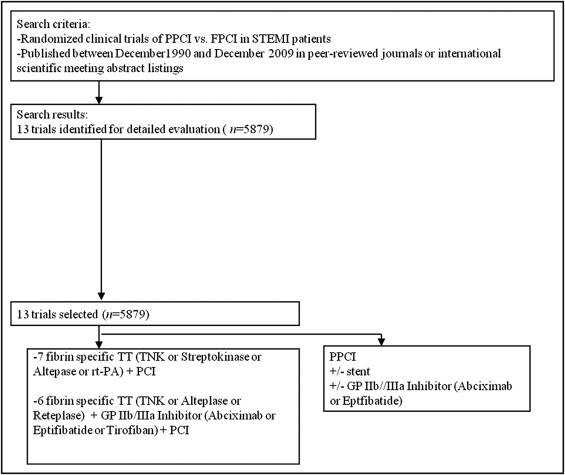
A total of 13 trials that enrolled 5,789 patients were pooled for analyses. The Which Early ST-Elevation Myocardial Infarction Therapy (WEST) trial included 3 randomized groups, but for the purposes of our analysis, we considered only the data from the FPCI and PPCI groups. Similarly, for the FINESSE trial, we considered only the data of fibrinolysis FPCI and PPCI groups. The main characteristics of interest of the selected randomized trials are listed in Table 1 . The quality of the studies was evaluated by the same 2 investigators for adequacy of allocation concealment, performance of the analysis according to the intention-to-treat principle, and blind assessment of the outcomes of interest. The study was performed in compliance with the Quality of Reporting of Meta-Analyses statement.
| Study | Inclusion Criteria | Patients | Symptom to Door (Minutes) | Type of Thrombolytic Agent | Type of Glycoprotein IIb/IIIa Inhibitor | 30-Day Mortality (%) | |||
|---|---|---|---|---|---|---|---|---|---|
| PPCI | FPCI | PPCI | FPCI | PPCI Benefit | |||||
| ASSENT IV | STEMI < 6 h | 1667 | 135 | 140 | Tenecteplase | 0 | 3.8 | 6 | +2.2 |
| SAMI | STEMI < 4 h | 122 | — | — | Streptokinase | 0 | 0 | 0 | 0 |
| PRAGUE | STEMI < 6 h | 201 | 120 | 112 | Streptokinase | 0 | 7 | 12 | +5 |
| Vermeer et al. | STEMI < 6 h | 149 | 130 | 140 | Alteplase | 0 | 7 | 8 | +1 |
| PACT | STEMI < 6 h | 606 | 84 | 84 | rt-PA | 0 | 3.3 | 3.6 | +0.3 |
| GRACIA 2 | STEMI < 12 h | 212 | 192 | 198 | Tenecteplase | 0 | 5 | 3 | −2 |
| WEST | STEMI < 6 h | 204 | 100 | 114 | Tenecteplase | 0 | 1 | 1 | 0 |
| FINESSE | STEMI < 6 h | 1634 | 150 | 150 | Reteplase | Abciximab | 5.6 | 5.2 | −0.4 |
| SPEED | STEMI < 12 h | 304 | — | — | Reteplase | Abciximab | 3.2 | 3.3 | +0.1 |
| BRAVE | STEMI < 12 h | 253 | 140 | 130 | Reteplase | Abciximab | 1.6 | 1.6 | 0 |
| ADVANCE MI | STEMI < 6 h | 146 | 132 | 150 | Tenecteplase | Eptifibatide | 0 | 7 | +7 |
| APAMIT | STEMI < 6 h | 70 | 145 | 135 | Alteplase | Abciximab | 3 | 3 | 0 |
| ATAMI | STEMI < 6 h | 311 | — | 150 | Alteplase | Tirofiban | 6.3 | 0.7 | −5.6 |
Survival benefit was calculated as the 30-day mortality after FPCI minus the 30-day mortality after PPCI. Because the outcome was mortality, the control (i.e., facilitated) mortality rate was interpreted as a proxy for mortality risk. Moreover, not only can this value be considered a surrogate of the underlying risk, but it also has the advantage of being a measure that reflects multiple factors contributing to outcome occurrence after FPCI (e.g., hemorrhage, reinfarction).
We used a weighted metaregression to test the relation between mortality risk and explanatory variables. A fixed-effect linear regression analysis modeling the log odds ratio (PPCI/FPCI) as a linear function of the log odds of FPCI mortality was used to estimate the mortality risk that nullified the 30-day survival benefit of PPCI over FPCI. A sensitivity analysis was carried out excluding alternatively from the set of studies the trials with the minimum and the maximum effects. The magnitude and statistical significance of all relations were estimated using weighted least squares regression, in which the results of each trial were weighted by the inverse of the variances within the study. The heterogeneity of the studies was tested using the Q statistic, complemented by the I 2 index. Statistical tests were 2 tailed and conducted at a significance level of 0.05. All the analyses were conducted using SAS version 9.1.3 for Windows (SAS Institute Inc., Cary, North Carolina).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


