The purpose of this study was to evaluate and compare the diagnostic accuracy and radiation dose of dual-source computed tomographic (DSCT) coronary angiography for assessment of coronary artery disease using prospective electrocardiographic triggering and retrospective electrocardiographically (ECG) gated spiral scans. One hundred sixteen patients who had undergone dual-source computed tomography and conventional coronary angiography were enrolled in this study. Fifty-four patients were scanned using retrospective ECG-gated protocols (group 1) and 62 patients using prospective ECG-triggered protocols (group 2). Diagnostic accuracy, image quality, and effective dose were compared between groups 1 and 2. Conventional coronary angiography was used as the reference standard. In total 1,709 (98.2%) coronary segments in the 116 patients were assessable with adequate image quality. Sensitivities and specificities of diagnosing coronary heart disease (≥50% stenosis) in a patient-based analysis of DSCT data were 93.3% and 88.9% in group 1 and 96.4% and 85.7% in group 2, respectively (p = 0.973 and 0.761). In vessel-based analysis, sensitivities and specificities were 77.4% and 94.1% in group 1 and 79.6% and 92.3% in group 2 (p = 0.983 and 0.985). Overall averaged image quality scores (using 1- to 4-point scale) in groups 1 and 2 were 3.3 ± 0.4 and 3.5 ± 0.9, respectively (p = 0.268). Prevalence of good (score 3.0) and excellent (score 4.0) image qualities of coronary vessels were 95.4% in group 1 and 92.4% in group 2 (p = 0.861). Effective doses were 8.82 ± 3.50 mSv (range 3.92 to 15.36) in group 1 and 2.95 ± 1.39 mSv (range 0.99 to 6.06) in group 2 (p <0.001). In conclusion, DSCT prospective ECG-triggered coronary angiography has equivalent image quality and diagnostic value compared to that of retrospective ECG-gated scans. Radiation dose was significantly decreased using prospective electrocardiographic triggering.
The radiation dose associated with computed tomographic coronary angiography (CTCA) has raised concerns that have led to the development of many dose-saving techniques for cardiac computed tomography in recent years. Hausleiter et al showed that the effective dose of CTCA could be decreased from 14.8 to 9.4 mSv using tailored retrospective electrocardiographically (ECG) gated scan protocols in 64-slice computed tomography. The recently developed prospective ECG-triggered sequential coronary scan protocol provides a new possibility to decrease dose. Previous studies have demonstrated that image quality can be maintained with significant dose savings using prospective electrocardiographic triggering. Estimated mean effective radiation dose using prospective electrocardiographic triggering in 64-slice computed tomography was higher than the conventional coronary angiographic (CCA) radiation dose (8.5 mSv, range 1.4 to 20.5, vs 2.1 mSv, range 1.0 to 3.3, p <0.001). However, most previous studies have compared only image quality and effective dosage in prospective and retrospective ECG-gated scans. This study investigated not only image quality and effective dose but also diagnostic efficacy of dual-source CT (DSCT) prospective electrocardiographic triggering compared to retrospective ECG-gated CT coronary angiography using conventional coronary angiography as the reference standard.
Methods
One hundred sixteen consecutive patients who had undergone DSCT coronary angiography and conventional coronary angiography were retrospectively analyzed in this study. Fifty-four patients (group 1) were scanned using retrospective ECG-gated DSCT protocols. Sixty-two consecutive patients (group 2) underwent prospective electrocardiographic triggering. All CT coronary angiographic studies were performed within 2 weeks of CCA examinations (most patients had undergone CCA examinations after CT coronary angiographic scans). Beta blockers and nitroglycerin were not used before CT angiographic scans. Exclusion criteria for this study in the 2 groups were coronary artery stenting or bypass grafting, severe arrhythmia (such as incessant atrial fibrillation and premature ventricular extra systole), and pacemaker implantation. All patients signed informed consents for CT coronary angiographic and CCA examinations.
A DSCT scanner (Somatom Definition, Siemens AG, Forchheim, Germany) was used for all CT examinations. The system was originally configured for only retrospective ECG-triggered scans (group 1) but was later upgraded to allow prospective ECG-triggered sequential scanning (group 2). Baseline heart rates of patients were comparable in groups 1 and 2.
For a prospective ECG-triggered sequential scan, tube voltage and current were 120 kV and 420 to 500 mA. Triggering phase was set at 70% of the RR interval. The “padding” option was used to extend the scan angle to 460°, which allows ±8% phase shift flexibility in electrocardiographic editing. DSCT retrospective ECG-gated scan protocols used a tube voltage of 120 kV and current of 330 to 430 mA. Pitch was 0.31 ± 0.5, adapted to heart rate. A radiation exposure-decrease algorithm, i.e., electrocardiographic pulsing, was used to decrease the radiation dose outside the pulsing window. Full exposure was set to 35% to 75% of the RR interval and decreased to 20% outside this window.
In the prospective and retrospective groups, detector collimations were 2 × 32 × 0.6 mm and acquisition slices were 2 × 64 × 0.6 mm by z-flying focus spot. Gantry rotation speed was 0.33 second. Data reconstruction was done with a slice thickness of 0.6 mm, kernel of B26f, and field of view of 20 to 25 cm.
Contrast medium was injected through a 20-gauge trocar in the antecubital vein using a power injector (Stellant, Medrad, Indianola, Pennsylvania). Depending on patient weight iohexol with iodine 350 mg/ml (Omnipaque 350, GE Healthcare) or iopromide with iodine 370 mg/ml (Ultravist 370, Bayers-Schering Pharma, Germany) was injected at a speed of 4 to 5.5 ml/s. Contrast medium was injected in 3 phases: 50 to 60 ml of contrast medium only in the first phase, 30-ml mixture of contrast medium (9 ml) and saline (21 ml) in the second phase, and saline 40 ml in the final phase. A bolus tracking technique was used to trigger the scan using the root of the aorta as the region of interest, 100 HU, and a 6-second delay.
A patient’s heart rate was recorded during the scan and an average heart rate was calculated afterward. Effective dose for CTCA was derived from the product of the dose–length product and the conversion coefficient k = 0.014 as previously suggested.
CCA procedures were performed by cardiologists. Left and right coronary artery angiography was performed through the right radial or femoral artery by an improved Seldinger technique. Six angiographic projections were taken at left anterior oblique and left cranial and caudal angulations and right anterior oblique and right cranial and caudal angulations. Additional projections were made, if needed, such as posteroanterior projections. Coronary arteries were named according to the American Heart Association model and segments with diameter <1.5 mm at the origin were excluded from the analysis. Degree of stenosis was quantified visually by 2 experienced cardiologists. For discrepancy between the 2 reviewers, a joint reading session was used to reach consensus. Radiation dose in conventional coronary angiography was not recorded and evaluated in this study.
The cardiac phase with the best image quality was selected manually by a radiologist to reconstruct raw DSCT images. Raw image data were transferred to a workstation (Multi-Modality Workplace, Siemens AG) for 3-dimensional reconstruction such as multiplanar reconstruction, maximum intensive projection, curved planar reformation, and volume rendering using commercially available software (Circulation and InSpace, Siemens AG).
Coronary arteries were evaluated on a segment, vessel, and patient level. Segments of coronary arteries were classified as previously reported. If a coronary artery was left dominant, more segments (posterior branch of left ventricle and posterior descending artery) of the left circumflex coronary artery were evaluated. Coronary artery branches were defined as left main, left anterior descending, left circumflex, and right coronary arteries. Degree of stenosis was defined visually by 2 experienced readers. Stenoses were graded at 5 levels: grade 0, no stenosis; grade 1, <50% stenosis; grade 2, 50% to 74% stenosis; grade 3, 75% to 99% stenosis; grade 4, 100% stenosis.
A 4-point scale was used to grade the image quality of CT coronary angiographic scans: score 1, unevaluable image quality caused by, e.g., poor opacification, blurred arterial wall, or severe motion artifacts; score 2, fair image quality but only evaluable if combined with transaxial images; score 3, good image quality with clear arterial wall and minor artifacts; score 4, excellent image quality and free of artifacts.
Stenosis and image quality of coronary arteries on CT coronary angiogram were assessed independently by 2 reviewers. A discrepancy between the 2 reviewers was solved in a second session in which the 2 reviewers read the image together and reached a final diagnosis. CT coronary angiographic reviewers were blinded to CCA results. Another 2 reviewers who were blinded to CT coronary angiographic results evaluated CCA data. CT coronary angiographic results were compared to CCA results, which was the gold standard.
All statistical analysis was performed using SPSS 16.0 (SPSS, Inc., Chicago, Illinois). Unpaired t tests were used to compare age, body mass index, baseline heart rate, contrast medium used, and image quality scores between these 2 groups. Mann–Whitney tests were used to compare coronary calcium scores, which were non-normally distributed data in these 2 groups. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were derived using regular formulas and compared using chi-square tests in different subgroups. Interobserver agreements for detection of ≥50% stenosis on CT coronary angiogram and conventional coronary angiogram were tested with Cohen kappa values at patient and vessel levels. Area under the receiver operating characteristic curve was used to compare diagnostic efficacy between group 1 and group 2. A p value <0.05 was considered statistically significant.
Results
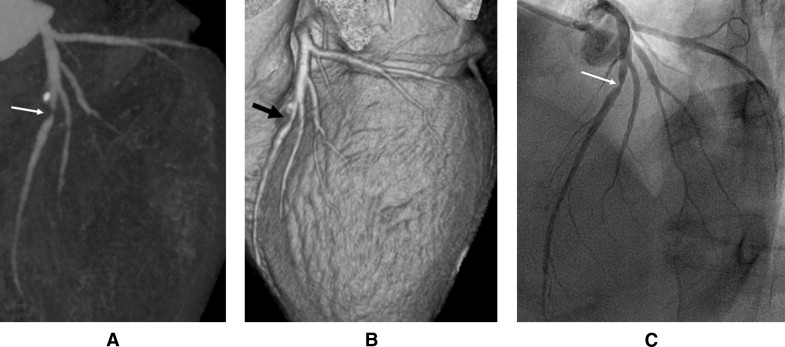
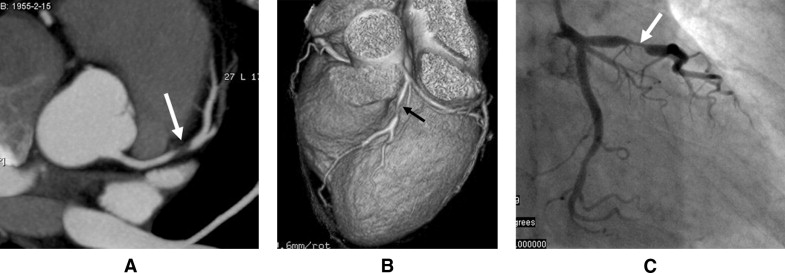
All 116 patients successfully underwent CT coronary angiographic and CCA examinations. Characteristics and risk factors of patients are presented in Table 1 . In this study, conventional coronary angiography confirmed that 100 of 116 patients (86.2%), 196 of 456 (42.9%) coronary vessels, and 296 of 1,709 (17.3%) coronary segments had ≥50% luminal stenosis. On a group level 45 of 54 patients in group 1 and 55 of 62 patients in group 2 were diagnosed as positive for coronary artery disease (CAD; Figures 1 and 2 , Table 2 ). The high prevalence of disease shown in this study was probably because more patients with positive CT coronary angiographic studies were referred to CCA examinations.
| Variable | Retrospective Electrocardiographic Gating | Prospective Electrocardiographic Triggering | p Value |
|---|---|---|---|
| (n = 54) | (n = 62) | ||
| Men | 42 (77.8%) | 42 (67.7%) | 0.735 |
| Age (years) | 56.8 ± 11.5 | 55.7 ± 9.7 | 0.562 |
| Body mass index (kg/m 2 ) | 26.0 ± 2.8 | 25.3 ± 3.0 | 0.206 |
| Previous myocardial infarction | 7 (13.0%) | 8 (12.9%) | 0.790 |
| Angina pectoris | 45 (83.3%) | 50 (80.6%) | 0.984 |
| Hypertension | 29 (53.7%) | 39 (62.9%) | 0.719 |
| Diabetes mellitus | 12 (22.2%) | 14 (22.6%) | 0.857 |
| Hypercholesterolemia ⁎ | 25 (46.3%) | 38 (61.3%) | 0.198 |
| Smoker | 28 (51.9%) | 31 (50.0%) | 0.963 |
| Heart rate during computed tomographic scanning (beats/min) | 71.2 ± 11.3 | 67.7 ± 10.5 | 0.313 |
| Contrast medium used (ml) | 65.5 ± 3.1 | 67.4 ± 2.7 | 0.782 |
| Calcium score † | 197.8 ± 422.6 | 254.9 ± 396.3 | 0.397 |
⁎ Serum total cholesterol ≥230 mg/dl and/or serum triglycerides ≥200 mg/dl or use of lipid-lowering agents.
† Mann–Whitney rank-sum test was used to compare calcium scoring in the prospective and retrospective groups.
| Retrospective Electrocardiographic Gating | Prospective Electrocardiographic Triggering | p Value | |
|---|---|---|---|
| (n = 54) | (n = 62) | ||
| Patient level | |||
| Sensitivity | 93.3% (42/45) | 96.4% (53/55) | 0.973 |
| Specificity | 88.9% (8/9) | 85.7% (6/7) | 0.761 |
| Positive predictive value | 97.7% (42/43) | 98.1% (53/54) | 0.898 |
| Negative predictive value | 72.7% (8/11) | 75.0% (6/8) | 0.727 |
| Accuracy | 92.6% (50/54) | 95.2% (59/62) | 0.972 |
| Vessel level | |||
| Sensitivity | 77.4% (72/93) | 79.6% (82/103) | 0.983 |
| Specificity | 94.1% (111/118) | 92.3% (131/142) | 0.985 |
| Positive predictive value | 91.1% (72/79) | 88.2% (82/93) | 0.970 |
| Negative predictive value | 84.1% (111/132) | 86.2% (131/152) | 0.958 |
| Accuracy | 86.7% (183/211) | 86.6% (213/246) | 0.955 |
| Segment level | |||
| Sensitivity | 78.9% (112/142) | 76.6% (118/154) | 0.939 |
| Specificity | 96.2% (629/654) | 97.4% (739/759) | 0.902 |
| Positive predictive value | 81.8% (112/137) | 85.5% (118/138) | 0.871 |
| Negative predictive value | 95.4% (629/659) | 95.4% (739/775) | 0.980 |
| Accuracy | 93.1% (741/796) | 93.9% (857/913) | 0.933 |
Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of CTCA were calculated on patient, vessel, and segment levels in the 2 groups ( Table 2 ). Results indicated that no statistically significant differences were found between groups 1 and 2 (p >0.05 for all comparisons).
Positive test likelihood ratios at the patient level (8.41 in group 1 and 6.74 in group 2) were worse than that at the vessel level (13.12 in group 1 and 10.34 in group 2). However, negative test likelihood ratios at the patient level (0.08 in group 1 and 0.04 in group 2) were better than those at the vessel level (0.24 in group 1 and 0.22 in group 2).
At the segment level, there were 111 (6.5%) segments with a conflicting diagnosis of stenosis by conventional coronary angiography in these 111 segments, 25 segments had a mismatch of segment terminology between CTCA and conventional coronary angiography in the other 86 segments, 38 were misdiagnosed as false positive (overestimated stenosis), and 48 segments were misdiagnosed as false negative (underestimated stenosis). No statistical differences were found between group 1 and group 2 for false positive (21 vs 17, p = 0.565) compared to false negative (26 vs 22, p = 0.332).
Using results of conventional coronary angiography as the gold standard, true-positive, true-negative, false-positive, false-negative diagnoses and assessable coronary arteries are presented in Table 3 . Unassessable coronary segments on CT coronary angiogram were caused by inadequate visualization owing to proximal luminal total occlusion (in 24 segments) and motion artifact (in 7 segments). Receiver operating characteristic analyses demonstrated that DSCT retrospective ECG-gated and prospective ECG-triggered scan protocols had similar diagnostic efficacy for detecting ≥50% stenosis on patient and vessel levels ( Figures 3 and 4 , respectively).



