The Arab Middle East is a unique region of the developing world where little is known about the outcomes of patients hospitalized with an acute coronary syndrome (ACS), despite playing an important role in the global burden of cardiovascular disease. The primary objectives of this observational study were to compare patients with ACS hospitalized in the Arab Middle East to patients enrolled in a multinational non-Arabian ACS registry. The study cohort consisted of patients hospitalized in 2007 with an ACS including 4,445 from the Global Registry of Acute Coronary Events (GRACE) and 6,706 from the Gulf Registry of Acute Coronary Events (Gulf RACE). Average age of patients in Gulf RACE was nearly a decade younger than that in GRACE (56 vs 66 years). Patients in Gulf RACE were more likely to be men, diabetic, and smoke and less likely to be hypertensive compared to patients in GRACE. Patients in Gulf RACE had higher odds of receiving aspirin and a lower likelihood of receiving angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, β blockers, and clopidogrel during their index hospitalization. Although most eligible patients with ST-elevation myocardial infarction in Gulf RACE received thrombolytics, most of their counterparts in GRACE underwent a primary percutaneous coronary intervention. Multivariable adjusted in-hospital case–fatality rates were not significantly different between patients in Gulf RACE and those in GRACE. In conclusion, despite differences in patient characteristics and treatment practices, short-term mortality rates were comparable in patients with ACS enrolled in these 2 registries. Future studies should explore the effects of these differences on long-term prognosis and other pertinent patient outcomes.
The primary objectives of this observational study were to compare the characteristics, management, and short-term outcomes of patients hospitalized with an acute coronary syndrome (ACS) in the Arab Middle East to a large multinational sample of patients with ACS using patient-level data from 2 large ACS registries.
Methods
Full details of the Global Registry of Acute Coronary Events (GRACE) and Gulf Registry of Acute Coronary Events (Gulf RACE) projects have been previously published.
Gulf RACE is a prospective registry of all patients hospitalized with an ACS in 65 centers in 6 Arab Middle Eastern countries (Kuwait, Oman, United Arab Emirates, Yemen, Qatar, and Bahrain). Patients were enrolled in this observational study from January through June 2007. All hospitals that care for patients with ACS in Kuwait, Bahrain, and Qatar participated, as did most hospitals in Yemen, United Arab Emirates, and Oman.
GRACE is the largest multinational prospective registry designed to reflect an unselected population of patients hospitalized with an ACS. In total 123 hospitals located in 14 countries in North and South America, Europe, Australia, and New Zealand contributed data to this registry from 1999 through 2007. For the present analyses, we used contemporaneous individual patient data of patients with ACS enrolled in the 2 registries during calendar year 2007.
All patients with a clinical history of ACS accompanied by ≥1 of the following were included in the respective study samples: electrocardiographic changes consistent with ACS, serial increases in cardiac biomarkers of necrosis, or documented coronary artery disease. Patients were diagnosed with ST-segment elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), or unstable angina pectoris using standardized criteria based on clinical presentation, electrocardiographic findings, and cardiac biomarkers. In the 2 patient registries the diagnosis of ACS and definitions of key study variables and clinical complications were similar and were based on American College of Cardiology key data elements. Information about the use of coronary artery bypass grafting was not collected in Gulf RACE.
For ease of interpretation patients with STEMI and patients with left bundle branch block were combined in 1 category (STEMI) and patients with NSTEMI and those with unstable angina pectoris were combined in another category (NSTE-ACS).
Univariate comparisons of patient characteristics, clinical presentation, management practices, and outcome data were carried out using Wilcoxon rank-sum or chi-square tests. Short-term hospital survival rates were estimated using the Kaplan-Meier method. Cox proportional hazards models were employed to compare hazards of in-hospital death between patients enrolled in the 2 registries and control for potentially confounding variables of prognostic importance. Two multivariable adjusted models were built; in the first, we adjusted for age and gender only and in the second we also controlled for all baseline characteristics and clinical presentation variables that were significantly associated with in-hospital mortality in univariate analyses. Logistic regression modeling was used to more systematically examine differences in risk of adverse in-hospital outcomes other than death between patients enrolled in the 2 registries and control for potential confounding demographic and clinical characteristics. We did not control for use of hospital treatments because of the nonrandomized nature of this study and potential for confounding by indication.
Results
In total 11,151 patients (4,445 from GRACE and 6,706 from Gulf RACE) with a confirmed diagnosis of ACS admitted in 2007 constituted our study population. Of patients in Gulf RACE 39% had an STEMI; of patients enrolled in GRACE 34% developed STEMI.
Patients in Gulf RACE were on average nearly a decade younger than patients enrolled in GRACE. The proportion of patients <55 years old in Gulf RACE was approximately 2 times that in GRACE, whereas the proportion of patients ≥75 years old in Gulf RACE was <1/3 that of GRACE ( Table 1 ).
| Characteristic | All ACS | STEMI | NSTE-ACS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| GRACE (n = 4,445) | Gulf RACE (n = 6,706) | p Value | GRACE (n = 1,504, 34%) | Gulf RACE (n = 2,619, 39%) | p Value | GRACE (n = 2,941, 66%) | Gulf RACE (n = 4,087, 61%) | p Value | |
| Age (years), mean ± SD | 65.5 ± 13 | 56.4 ± 13 | <0.01 | 63.8 ± 14 | 54.4 ± 13 | <0.01 | 67.3 ± 13 | 57.3 ± 13 | <0.01 |
| Age (years) | |||||||||
| <55 | 1,039 (23%) | 3,099 (46%) | 428 (28%) | 1,399 (53%) | 611 (21%) | 1,700 (42%) | |||
| 55–64 | 1,136 (26%) | 1,830 (27%) | 389 (26%) | 656 (25%) | 747 (25%) | 1,174 (29%) | |||
| 65–74 | 1,061 (24%) | 1,232 (18%) | 331 (22%) | 395 (15%) | 730 (25%) | 837 (21%) | |||
| ≥75 | 1,209 (27%) | 545 (8%) | <0.01 | 356 (24%) | 169 (7%) | <0.01 | 853 (29%) | 376 (9%) | <0.01 |
| Men | 3,072 (69%) | 5,071 (76%) | <0.01 | 1,099 (73%) | 2,250 (86%) | <0.01 | 1,973 (67%) | 2,821 (69%) | 0.08 |
| Body mass index (kg/m 2 ), mean ± SD | 28.1 ± 5.7 | 27.6 ± 5.4 | <0.01 | 27.5 ± 5.0 | 26.8 ± 4.8 | <0.01 | 28.4 ± 6.0 | 28.1 ± 5.6 | 0.03 |
| Diabetes mellitus | 1,181 (27%) | 2,745 (41%) | <0.01 | 328 (22%) | 841 (32%) | <0.01 | 853 (29%) | 1,904 (47%) | <0.01 |
| Hypertension | 2,929 (66%) | 3,364 (50%) | <0.01 | 851 (57%) | 890 (34%) | <0.01 | 2,078 (71%) | 2,474 (61%) | <0.01 |
| Previous percutaneous coronary intervention or coronary artery bypass grafting | 1,227 (28%) | 1,049 (16%) | <0.01 | 217 (15%) | 173 (7%) | <0.01 | 1,010 (35%) | 876 (22%) | <0.01 |
| Current smoker | 1,217 (28%) | 2,452 (37%) | <0.01 | 536 (36%) | 1,318 (50%) | <0.01 | 681 (23%) | 1,134 (28%) | <0.01 |
| Renal impairment | 691 (16%) | 1,170 (18%) | 0.01 | 188 (13%) | 459 (18%) | <0.01 | 503 (17%) | 711 (18%) | 0.40 |
| Length of stay (days), mean ± SD | 6.6 ± 6.8 | 5.6 ± 4.6 | <0.01 | 6.6 ± 6.9 | 6.1 ± 4.3 | <0.01 | 6.6 ± 6.8 | 5.2 ± 4.7 | <0.01 |
Patients in Gulf RACE were more likely to be men, diabetic, currently smoke, and have renal impairment than patients enrolled in GRACE; in contrast, these patients were less likely to be hypertensive or have previously undergone coronary revascularization. These differences remained when we examined the distribution of these characteristics between the 2 registry populations according to ACS type ( Table 1 ).
Patients developing STEMI in Gulf RACE were more likely to have longer prehospital delays in seeking medical care compared to patients included in GRACE. Of 2,540 patients with STEMI in Gulf RACE who presented within 24 hours of acute symptom onset, 784 (31%) presented >12 hours after symptom onset; in GRACE 1,381 patients with STEMI presented within 24 hours of symptom onset, of which 139 (10%) presented >12 hours after acute symptom onset. Average hospital stay was significantly shorter for patients with ACS included in Gulf RACE by nearly 1 day ( Table 1 ).
By clinical presentation patients in Gulf RACE were more likely to present with higher heart rate and initial glucose values, and in a higher Killip class compared to patients enrolled in GRACE. These differences persisted when comparing the respective study populations across types of ACS ( Table 2 ).
| Characteristic | All ACS | STEMI | NSTE-ACS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| GRACE (n = 4,445) | Gulf RACE (n = 6,706) | p Value | GRACE (n = 1,504, 34%) | Gulf RACE (n = 2,619, 39%) | p Value | GRACE (n = 2,941, 66%) | Gulf RACE (n = 4,087, 61%) | p Value | |
| Heart rate (beats/min), mean ± SD | 79.0 ± 21 | 86.0 ± 23 | <0.01 | 79.0 ± 22 | 85.1 ± 23 | <0.01 | 79.0 ± 21 | 87.0 ± 23 | <0.01 |
| Systolic blood pressure (mm Hg), mean ± SD | 140.0 ± 29 | 140.0 ± 31 | 0.70 | 136.0 ± 30 | 134.0 ± 31 | 0.30 | 142.0 ± 29 | 143.0 ± 30 | 0.30 |
| Initial glucose (mg/dl), mean ± SD | 158.0 ± 267 | 196.0 ± 193 | <0.01 | 168.0 ± 155 | 200.0 ± 154 | <0.01 | 153 ± 310 | 193 ± 214 | <0.01 |
| Initial creatinine (mg/dl), mean ± SD | 1.21 ± 0.9 | 1.22 ± 1.1 | 0.50 | 1.17 ± 0.8 | 1.2 ± 0.9 | 0.30 | 1.24 ± 0.9 | 1.24 ± 1.2 | 0.80 |
| Killip class | |||||||||
| I | 3,756 (85%) | 5,219 (78%) | <0.01 | 1,251 (83%) | 2,068 (79%) | <0.01 | 2,505 (85%) | 3,151 (77%) | <0.01 |
| II | 416 (9%) | 874 (13%) | <0.01 | 152 (10%) | 322 (12%) | 0.03 | 264 (9%) | 552 (14%) | <0.01 |
| III | 167 (3.8%) | 460 (6.9%) | <0.01 | 56 (3.8%) | 139 (5.3%) | 0.02 | 111 (3.8%) | 321 (7.9%) | <0.01 |
| IV | 46 (1.1%) | 137 (2.1%) | <0.01 | 24 (1.6%) | 86 (3.3%) | <0.01 | 22 (0.8%) | 51 (1.3%) | 0.04 |
| Cardiac arrest | 161 (3.7%) | 168 (2.5%) | <0.01 | 75 (5.0%) | 125 (4.8%) | 0.70 | 86 (3.0%) | 43 (1.1%) | <0.01 |
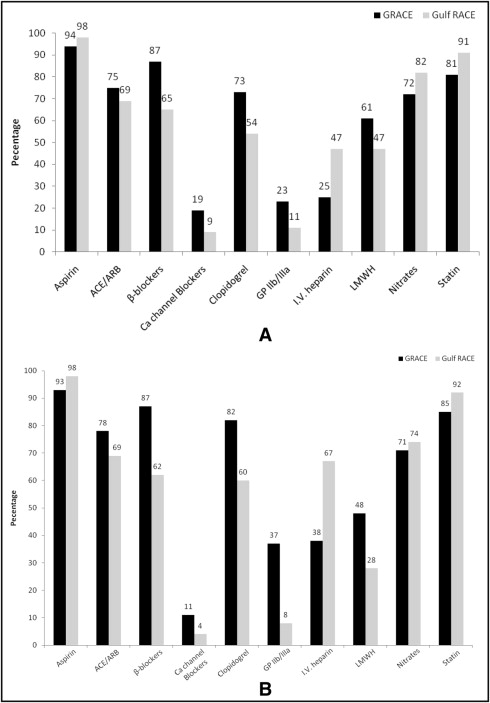
Although patients in Gulf RACE were more likely to have been prescribed aspirin, nitrates, and statins, they were less likely to have received β blockers, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, calcium channel blockers, clopidogrel, or glycoprotein IIb/IIIa antagonists compared to patients enrolled in GRACE during the first 24 hours of hospital admission. Patients in Gulf RACE were more likely to have been managed with intravenous heparin compared to patients enrolled in GRACE who were more likely to have been managed with low-molecular-weight heparin. Similar patterns were observed when comparing patients with STEMI between the 2 registries ( Figure 1 ) . Nearly 75% of GRACE hospitals had on-site catheterization facilities compared to only 20% of Gulf RACE hospitals. In addition, nearly all hospitals in GRACE had coronary care units compared to <65% of hospitals in Gulf RACE.
Cardiac catheterization was performed nearly 4 times as frequently in GRACE compared to Gulf RACE in patients with STEMI (81.1% vs 18.0%) and those with NSTE-ACS (59.4% vs 13.1%). Thrombolysis was the reperfusion strategy of choice in patients with STEMI enrolled in Gulf RACE compared to GRACE. Patients who developed STEMI in GRACE were more likely to receive primary percutaneous coronary intervention (PCI). In total 1,242 patients with STEMI in GRACE presented within 12 hours of symptom onset, of whom 163 (13%) received thrombolytics, 805 (65%) received primary PCI, 13 (1%) underwent coronary artery bypass grafting, and 261 (21%) did not receive any reperfusion procedure. In Gulf RACE 1,756 patients with STEMI presented within 12 hours of symptom onset, of whom 1,364 (78%) received thrombolytics, 227 (13%) received primary PCI, and 165 (9%) did not receive any form of coronary reperfusion therapy ( Figure 2 ) .
Although patients in Gulf RACE, irrespective of their ACS diagnosis, were at higher risk for developing heart failure during their index hospitalization, only patients with STEMI in Gulf RACE had a significantly higher risk of developing cardiogenic shock compared to patients included in GRACE. In contrast, patients in Gulf RACE had a significantly lower risk of developing major bleeding during their hospitalization ( Table 3 ). Patients in Gulf RACE had higher in-hospital case fatality rates compared to those in GRACE (1.3% vs 1.9%, 1.9% vs 3.5%, 3.7% vs 5.4%, and 7.7% vs 10.8%) in each age stratum examined (<55, 55 to 64, 65 to 74, and ≥75 years old), respectively (p ≤0.05 for all comparisons except for the <55-year-old group).
| In-Hospital Outcome | All ACS | STEMI | NSTE-ACS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GRACE (n = 4,445) | Gulf RACE (n = 6,706) | Adjusted OR (95% CI) | p Value | GRACE (n = 1,504, 34%) | Gulf RACE (n = 2,619, 39%) | Adjusted OR (95% CI) | p Value | GRACE (n = 2,941, 66%) | Gulf RACE (n = 4,087, 61%) | Adjusted OR (95% CI) | p Value | |
| Cardiogenic shock | 142 (3.2%) | 347 (5.2%) | 1.39 (1.06–1.83) | <0.01 | 83 (5.5%) | 252 (9.6%) | 1.69 (1.42–1.93) | <0.01 | 59 (2.0%) | 95 (2.3%) | 1.26 (1.09–1.48) | 0.37 |
| Heart failure | 384 (9%) | 1,099 (16%) | 2.23 (1.91–2.56) | <0.01 | 177 (12%) | 454 (17%) | 1.92 (1.54–2.39) | <0.01 | 207 (7%) | 645 (16%) | 2.81 (2.33–3.39) | <0.01 |
| Echocardiography done | 2,634 (60%) | 4,146 (62%) | 0.03 | 1,098 (74%) | 1,845 (71%) | 0.04 | 1,536 (53%) | 2,301 (56%) | <0.01 | |||
| Left ventricular ejection fraction ≤40% | 709 (16%) | 1,283 (19%) | <0.01 | 322 (21%) | 620 (24%) | <0.01 | 387 (13%) | 663 (16%) | <0.01 | |||
| Major bleeding | 89 (2.0%) | 52 (0.8%) | 0.37 (0.25–0.54) | <0.01 | 36 (2.4%) | 31 (1.2%) | 0.49 (0.30–0.81) | <0.01 | 53 (1.8%) | 21 (0.5%) | 0.27 (0.16–0.44) | <0.01 |
| Stroke | 21 (0.5%) | 49 (0.7%) | 2.45 (1.25–4.82) | 0.09 | 9 (0.6%) | 32 (1.2%) | 3.32 (1.28–8.63) | 0.054 | 12 (0.4%) | 17 (0.4%) | 1.59 (0.66–3.83) | 0.96 |
| Death | 167 (3.8%) | 247 (3.7%) | 1.09 (0.84–1.41) | 0.84 | 93 (6.2%) | 172 (6.6%) | 1.29 (0.92–1.79) | 0.63 | 74 (2.5%) | 75 (1.8%) | 0.77 (0.53–1.13) | 0.06 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


