Implantation of cardiac implantable electronic devices (CIED) has dramatically increased over the past several years. Although several preventive measures have been implemented, there has been a disproportional increase in the number of CIED-related infections. To evaluate the adherence of bacteria to polyurethane and titanium, the 2 surfaces that coat the CIED, we proceeded with an in vitro study using the most common microorganisms responsible for CIED-related infections. Original, unused 1 × 1 centimeter titanium and polyurethane flat plates were incubated with coagulase-negative staphylococci, methicillin-resistant Staphylococcus aureus , and Pseudomonas aeruginosa . Each experiment was repeated 5 times. After incubating the titanium and polyurethane plates for 3, 6, 12, or 24 hours, all 3 organisms displayed a higher grade of bacterial adherence to the polyurethane versus titanium surfaces (p = 0.01). In conclusion, to decrease the rate of bacterial adherence, especially during the immediate postimplantation period when the CIED is at high risk for bacterial adherence, colonization, and infection, it may be prudent to consider constructing CIED surfaces with a higher proportion of titanium over polyurethane. Animal studies are warranted to explore the relevance of these laboratory findings.
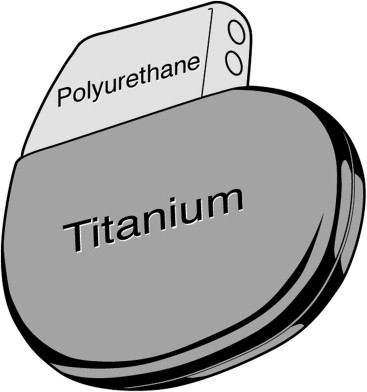
Implantation of cardiac implantable electronic devices (CIED) has dramatically increased over the past several years. Unfortunately, along with the rising use of these devices, there has been a disproportionate increase in the number of CIED-related infections. The rate of these infection ranges from 0.13% to 19.9%, with an average rate of 4%. Once the CIED has becomes infected, usually the entire device needs to be removed. The estimated average cost of combined medical-surgical treatment of an infected device ranges from $25,000 to $50,000. Several preventive measures have been implemented to decrease the rate of device-related infections, including the use of antisepsis and perioperative antimicrobials. The exterior surfaces of CIED are commonly made of titanium and polyurethane. An extensive evaluation of the intrinsic propensity of these 2 materials to promote bacterial adherence has not yet been conducted. We report the findings of an in vitro study assessing bacterial adherence of the most common pathogens causing CIED-related infections to both titanium and polyurethane surfaces.
Methods
Original, unused 1 × 1 centimeter flat plates made of polyurethane or titanium were obtained from Medtronic (Mounds View, Minnesota; Figure 1 ). The material was sterilized using an autoclave at 125°C for 20 minutes. Once sterilized, the polyurethane and titanium plates were each placed in an individual sterile tube. Each tube was then filled with 5 ml of trypticase soy broth. Thereafter, the tubes were filled with 10 5 colony-forming units of a CIED biofilm-producing clinical isolate of (1) coagulase-negative staphylococci (CNS), (2) methicillin-resistant Staphylococcus aureus (MRSA), or (3) Pseudomonas aeruginosa . The titanium and polyurethane plates were then individually incubated for 3, 6, 12, or 24 hours at 37°C in a low-velocity orbital shaker. After formation of biofilm, to remove any planktonic bacteria, the plates were removed from the tube, and washed 3 consecutive times with 10 ml of normal saline. Thereafter the washed plates were placed in a new sterile container with 5 ml of trypticase soy broth. Each tube was then sonicated for 5 minutes and then vortexed for 30 additional seconds. Subsequently, 0.1-ml aliquots of the sonicated-vortexed suspension were obtained, and then serial 10-fold dilutions were inoculated onto blood agar plates. The experiment was repeated 5 times. The Wilcoxon rank-sum tests were used for comparisons of the extent of bacterial adherence. All analyses were 2-sided tests at a significance level of 0.05. The statistical analyses were performed by using SAS version 9.1 (SAS Institute Inc., Cary, North Carolina).
Results
After incubating the titanium and polyurethane plates for 3, 6, 12, or 24 hours, CNS, MRSA, and Pseudomonas displayed a higher quantity of bacterial adherence on the polyurethane versus titanium plates ( Figure 2 ). At all time frames, this difference was statistically significant (p = 0.01). Although not statistically significant, within the first 3 and 6 hours of incubation, Pseudomonas had a higher bacterial adherence than CNS and MRSA to both materials, but the reverse was observed with longer incubation periods.
Results
After incubating the titanium and polyurethane plates for 3, 6, 12, or 24 hours, CNS, MRSA, and Pseudomonas displayed a higher quantity of bacterial adherence on the polyurethane versus titanium plates ( Figure 2 ). At all time frames, this difference was statistically significant (p = 0.01). Although not statistically significant, within the first 3 and 6 hours of incubation, Pseudomonas had a higher bacterial adherence than CNS and MRSA to both materials, but the reverse was observed with longer incubation periods.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


