We sought to compare the angiographic findings and mortality in patients with non–ST-segment elevation (NSTEMI) versus ST-segment elevation myocardial infarction (STEMI) undergoing early invasive intervention. Of 11,872 patients enrolled in the Korean Acute Myocardial Infarction Registry from November 2005 to January 2008, we studied patients with NSTEMI undergoing early invasive intervention (n = 1,486) and those with STEMI undergoing primary percutaneous coronary intervention (n = 4,392). Multivessel coronary disease, baseline Thrombolysis In Myocardial Infarction (TIMI) flow grade 3, and the left circumflex artery as a culprit lesion occurred more frequently in patients with NSTEMI than in those with STEMI. Those with NSTEMI had a significantly lower mortality rate than those with STEMI during a median follow-up of about 12 months (3.8% vs 6.7%, p <0.001). In the patients with NSTEMI, the independent predictors of mortality included postprocedural TIMI flow grade 0 to 2 (hazard ratio [HR] 3.07, 95% confidence interval [CI] 1.01 to 9.29, p = 0.047) and multivessel coronary disease (HR 3.83, 95% CI 1.36 to 10.81, p = 0.010) but not baseline TIMI flow or infarct location. However, baseline TIMI flow grade 0 to 2 (HR 1.56, 95% CI 1.03 to 2.36, p = 0.035), anterior infarction (HR 1.69, 95% CI 1.28 to 2.23, p <0.001), multivessel coronary disease (HR 1.45, 95% CI 1.10 to 1.91, p = 0.008), and postprocedural TIMI flow grade 0 to 2 (HR 2.00, 95% CI 1.42 to 2.82, p <0.001) were all independent predictors of mortality in the patients with STEMI. In conclusion, the angiographic findings in patients from NSTEMI differ from those in patients with STEMI. Postprocedural TIMI flow and multivessel coronary disease were independent predictors of mortality in patients with NSTEMI undergoing early invasive intervention.
Angiographic variables such as the baseline and postprocedural Thrombolysis In Myocardial Infarction (TIMI) flow grade, infarct vessel location, and the presence of multivessel disease are known to be independent predictors of mortality in patients with acute myocardial infarction (MI). However, these data have mostly been derived from patients with ST-segment elevation MI (STEMI) undergoing primary percutaneous coronary intervention (PCI). The association between the angiographic findings and clinical outcomes in patients with non–STEMI (NSTEMI) is not well known. Although the long-term clinical outcomes of patients with NSTEMI have seemed similar to those of patients with STEMI, it has been reported that the angiographic findings in patients with NSTEMI differ from those in patients with STEMI in some aspects. The effect of the baseline and postprocedural TIMI flow grade on mortality is not well understood in patients with NSTEMI. Moreover, a paucity of data is available on the association between the infarct vessel location or the presence of multivessel disease and the clinical outcomes of patients with NSTEMI. To investigate the effect of the angiographic findings on the clinical outcomes in patients with NSTEMI compared to those with STEMI, we studied patients who underwent early invasive intervention from the nationwide Korea Acute Myocardial Infarction Registry (KAMIR).
Methods
The KAMIR is a Korean prospective multicenter on-line registry designed to reflect the “real-world” practice for Asian patients presenting with acute MI, with support from the Korean Society of Cardiology. Since November 2005, 50 hospitals highly experienced in primary PCI with sufficient volume have registered consecutive patients with acute myocardial infarction on-line (at www.kamir.or.kr ). Before the initiation of the KAMIR study, several investigator meetings were held, and a steering committee was selected to standardize the care given in clinical practice to minimize the differences in medical care among the different hospitals. MI was defined as elevated cardiac enzymes (troponin or MB fraction of creatine kinase) with ischemic symptoms or electrocardiographic findings indicative of ischemia and was further classified by the ST-segment change (STEMI or NSTEMI). STEMI was defined as ST-segment elevation >1 mm in ≥2 contiguous leads or presumably new-onset left bundle branch block. All other electrocardiographic patterns, including ST-segment depression or T-wave inversion, were diagnosed as NSTEMI. The patients with NSTEMI who underwent coronary angiography and PCI within 48 hours after hospitalization were classified into the early invasive intervention group.
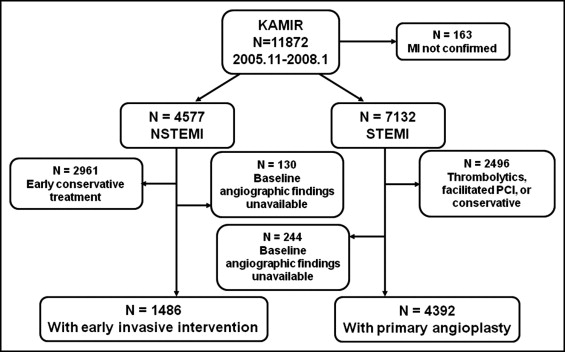
From November 2005 to January 2008, 11,872 patients were enrolled in the KAMIR. MI was confirmed in 11,709 patients at hospital discharge. NSTEMI and STEMI was diagnosed in 4,577 and 7,132 patients, respectively. In the NSTEMI group, 1,616 patients underwent early invasive intervention. Of these, angiographic data were available for 1,486 patients. In the STEMI group, 4,636 patients underwent primary PCI within 12 hours of symptom onset. Of these, angiographic data were available for 4,392 patients. The patient flow is shown in Figure 1 .
Coronary angiography and PCI were performed using standard techniques with appropriate antiplatelet therapy and heparin use. Patients received dual oral antiplatelet agents before PCI (300 mg aspirin and 300 to 600 mg clopidogrel). A bolus of 5,000 to 10,000 IU of unfractionated heparin was administered. Intravenous administration of glycoprotein IIb/IIIa receptor antagonists or the thrombectomy device used was at the operator’s discretion, and drug-eluting stents were used without restriction.
The demographic, clinical, laboratory, angiographic, procedural, and outcome data were collected by an Internet-based reporting system. Left ventricular systolic function was evaluated using echocardiography. The angiographic variables included the infarct vessel (left anterior descending artery vs left circumflex artery and right coronary artery), baseline and postprocedural TIMI flow grade of the infarct vessel (grade 0 to 2 vs grade 3), and extent of disease (multivessel vs single vessel). The infarct artery was determined by the operators, using the electrocardiographic and angiographic findings, as well as the echocardiographic findings, if available. The TIMI grade of the infarct vessel was determined from the angiograms obtained before and after the procedure. Multivessel coronary disease was defined as ≥50% stenosis of ≥2 major epicardial coronary arteries or their major branches.
The primary end point of the present study was mortality in patients with NSTEMI versus those with STEMI treated with early invasive intervention. Major cardiac adverse events, defined as death, reinfarction, or any revascularization, were also assessed. Death was defined as all-cause mortality, reinfarction as the recurrence of ischemic symptoms or electrocardiographic changes accompanied by elevated cardiac enzymes (troponin or CK-MB), and any revascularization as revascularization of either the target or nontarget vessels. All events were identified by the patient’s physician and confirmed by the principal investigator of each hospital. Clinical follow-up after the index MI was recommended at 1, 6, and 12 months. Calculation of the Global Registry of Acute Coronary Events score was determined from the admission data and calculated as previously described.
All analyses were performed using the Statistical Analysis Systems, software package, version 9.1 (SAS Institute, Cary, North Carolina). Continuous data are expressed as the mean ± SD or the median and interquartile range (twenty-fifth and seventy-fifth percentiles). Categorical data are expressed as percentages. Continuous variables were analyzed using Student’s t test or the Mann-Whitney U test, as appropriate, and categorical variables were compared using the chi-square test. Cumulative mortality event rates were evaluated using the Kaplan-Meier method and compared using the log-rank test. The influence of angiographic findings on mortality was evaluated using a Cox proportional hazards model with the following covariates: age, gender, body mass index, diabetes, hypertension, dyslipidemia, current smoking, renal dysfunction, systolic blood pressure, heart rate, number of stents used, total stent length, and stent diameter. p Values <0.05 were considered statistically significant.
Results
The patients with NSTEMI treated with early invasive intervention were older, more likely to be women, and more likely to have coronary risk factors, except for smoking, than the patients with STEMI treated with primary PCI ( Table 1 ). The angiographic and procedural variables stratified by MI type are presented in Table 2 . The median interval to treatment in patients with NSTEMI undergoing early invasive intervention was as follows: symptom onset-to-balloon time, 29 hours (interquartile range 13 to 64) and door-to-balloon time 18 hours (interquartile range 4 to 39). Compared to patients with STEMI, those with NSTEMI more frequently had baseline TIMI grade 3 flow and multivessel coronary disease and the left anterior descending artery was less often the infarct vessel. The median Global Registry of Acute Coronary Events risk score was significantly lower in the patients with NSTEMI than in those with STEMI (132, interquartile range 111 to 156, vs 152, interquartile range 130 to 176, p <0.001). Drug-eluting stents were implanted in >90% of patients in both groups. Glycoprotein IIb/IIIa inhibitors were used less frequently in the patients with NSTEMI than in those with STEMI. Although postprocedural TIMI grade 3 flow was achieved more often in patients with NSTEMI who had undergone early invasive intervention than in patients with STEMI treated with primary PCI, the TIMI 3 flow rate was fairly high in both groups.
| Variable | NSTEMI (n = 1,486) | STEMI (n = 4,392) | p Value |
|---|---|---|---|
| Age (years) | 63.3 ± 12.0 | 61.6 ± 15.3 | <0.001 |
| Men | 68.4% | 73.4% | <0.001 |
| Body mass index (kg/m 2 ) | 24.3 ± 3.1 | 24.0 ± 3.2 | <0.001 |
| Diabetes mellitus | 31.6% | 25.1% | <0.001 |
| Hypertension ⁎ | 54.4% | 46.1% | <0.001 |
| Dyslipidemia † | 28.2% | 18.2% | <0.001 |
| Current smoker | 40.5% | 48.5% | <0.001 |
| Renal dysfunction ‡ | 3.8% | 2.8% | 0.04 |
| Previous myocardial infarction | 3.6% | 2.5% | 0.03 |
| Previous percutaneous coronary intervention | 6.8% | 3.3% | <0.001 |
| Previous coronary artery bypass surgery | 0.8% | 0.3% | 0.02 |
| Killip class ≥2 | 18.4% | 24.5% | <0.001 |
| Hypotension § | 2.6% | 8.4% | <0.001 |
| Tachycardia ¶ | 9.8% | 8.8% | 0.24 |
⁎ Currently receiving antihypertensive therapy or systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg.
† Total cholesterol >200 mg/dl or low-density lipoprotein cholesterol >130 mg/dl or high-density lipoprotein cholesterol <40 mg/dl or receiving antilipidemic treatment.
‡ Serum creatinine >2.0 mg/dl.
§ Systolic blood pressure <90 mm Hg.
| Variable | NSTEMI (n = 1,486) | STEMI (n = 4,392) | p Value |
|---|---|---|---|
| Baseline Thrombolysis In Myocardial Infarction flow grade 3 | 592 (39.8%) | 695 (15.8%) | <0.001 |
| Infarct-related coronary artery | <0.001 | ||
| Left main | 38 (2.6%) | 45 (1.0%) | |
| Left anterior descending | 591 (39.8%) | 2,253 (51.3%) | |
| Left circumflex | 443 (29.8%) | 418 (9.5%) | |
| Right | 414 (27.9%) | 1,676 (38.2%) | |
| Multivessel coronary disease | 973 (65.5%) | 2,288 (52.1%) | <0.001 |
| Lesion type B2/C | 1,118 (75.2%) | 3,340 (76.0%) | 0.59 |
| Drug-eluting stents implanted | 1,348 (90.7%) | 3,928 (89.4%) | 0.22 |
| Glycoprotein IIb/IIIa inhibitors | 202 (13.6%) | 770 (17.5%) | <0.001 |
| Stent length (mm) | 24.6 ± 6.3 | 25.1 ± 6.2 | 0.002 |
| Stent diameter (mm) | 3.1 ± 0.4 | 3.2 ± 0.4 | <0.001 |
| Total stent number | 1.6 ± 0.9 | 1.4 ± 0.7 | <0.001 |
| Final Thrombolysis In Myocardial Infarction flow grade 3 | 1,448 (97.4%) | 4,103 (93.4%) | <0.001 |
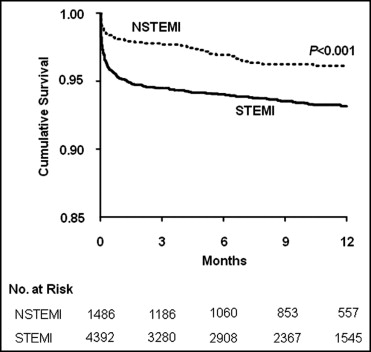
Clinical follow-up data were obtained for 97.5% of the patients. The median follow-up was 330 days (interquartile range 125 to 384). During the entire study period, 348 patients died (292 in the STEMI group and 56 in the NSTEMI group). The mortality rate was significantly lower for the patients with NSTEMI than for those with STEMI during the index hospitalization (1.7% vs 4.5%, p <0.001) and during follow-up (3.8% vs 6.7%, p <0.001), respectively ( Figure 2 ). The patients with NSTEMI with postprocedural TIMI flow grade 0 to 2 or multivessel coronary disease had a significantly greater mortality rate than those with postprocedural TIMI flow grade 3 or single-vessel disease, respectively ( Table 3 ). The baseline TIMI flow grade and the location of the infarct vessel were not significantly associated with mortality in those with NSTEMI. However, a baseline TIMI flow grade of 0 to 2 (hazard ratio [HR] 1.56, 95% confidence interval [CI] 1.03 to 2.36, p = 0.035), anterior infarction (HR 1.69, 95% CI 1.28 to 2.23, p <0.001), multivessel coronary disease (HR 1.45, 95% CI 1.10 to 1.91, p = 0.008), and postprocedural TIMI flow grade 0 to 2 (HR 2.00, 95% CI 1.42 to 2.82, p <0.001) were all independent predictors of mortality in those with STEMI. The incidence of major cardiac adverse events and any revascularization was significantly lower in the patients with multivessel coronary disease and NSTEMI undergoing complete revascularization than in those undergoing incomplete revascularization ( Table 4 ). Although it was not statistically significant, a trend was seen toward lower mortality in patients undergoing complete revascularization than in those undergoing incomplete revascularization.
| Outcome | Variable | p Value | |
|---|---|---|---|
| Preprocedural Thrombolysis In Myocardial Infarction flow grade | Grade 3 (n = 592) | Grade 0–2 (n = 894) | |
| Death | 17 (2.9%) | 39 (4.4%) | 0.14 |
| Reinfarction | 8 (1.4%) | 7 (0.8%) | 0.28 |
| Any revascularization | 32 (5.4%) | 47 (5.3%) | 0.90 |
| Major adverse cardiac events | 56 (9.5%) | 94 (10.5%) | 0.52 |
| Postprocedural Thrombolysis In Myocardial Infarction flow grade | Grade 3 (n = 1,448) | Grade 0–2 (n = 38) | |
| Death | 51 (3.5%) | 5 (13.2%) | 0.01 |
| Reinfarction | 15 (1.0%) | 0 | 0.99 |
| Any revascularization | 77 (5.3%) | 2 (5.3%) | 0.99 |
| Major adverse cardiac events | 143 (9.9%) | 7 (18.4%) | 0.09 |
| Infarct-related artery: left anterior descending artery | No (n = 895) | Yes (n = 591) | |
| Death | 33 (3.9%) | 23 (3.7%) | 0.84 |
| Reinfarction | 7 (0.8%) | 8 (1.3%) | 0.39 |
| Any revascularization | 48 (5.6%) | 31 (4.9%) | 0.57 |
| Major adverse cardiac events | 87 (10.2%) | 63 (10.0%) | 0.93 |
| Disease extent | Single-vessel disease (n = 513) | Multivessel disease (n = 973) | |
| Death | 6 (1.2%) | 50 (5.1%) | <0.001 |
| Reinfarction | 2 (0.4%) | 13 (1.3%) | 0.08 |
| Any revascularization | 19 (3.7%) | 60 (6.2%) | 0.04 |
| Major adverse cardiac events | 27 (5.3%) | 123 (12.7%) | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


