Innovative treatment strategies for decompensated heart failure (HF) are required to achieve cost savings and improvements in outcomes. We developed a decision analytic model from a hospital perspective to compare 2 strategies for the treatment of decompensated HF, ambulatory diuretic infusion therapy, and hospitalization (standard care), with respect to total HF hospitalizations and costs. The ambulatory diuretic therapy strategy included outpatient treatment with high doses of intravenous loop diuretics in a specialized HF unit whereas standard care included hospitalization for intravenous loop diuretic therapy. Model probabilities were derived from the outcomes of patients who were treated for decompensated HF at Brigham and Women’s Hospital (Boston, MA). Costs were based on Centers for Medicare and Medicaid reimbursement and the available reports. Based on a sample of patients treated at our institution, the ambulatory diuretic therapy strategy was estimated to achieve a significant reduction in total HF hospitalizations compared with standard care (relative reduction 58.3%). Under the base case assumptions, the total cost of the ambulatory diuretic therapy strategy was $6,078 per decompensation episode per 90 days compared with $12,175 per 90 days with standard care, for a savings of $6,097. The cost savings associated with the ambulatory diuretic strategy were robust against variation up to 50% in costs of ambulatory diuretic therapy and the likelihood of posttreatment hospitalization. An exploratory analysis suggests that ambulatory diuretic therapy is likely to remain cost saving over the long-term. In conclusion, this decision analytic model demonstrates that ambulatory diuretic therapy is likely to be cost saving compared with hospitalization for the treatment of decompensated HF from a hospital perspective. These results suggest that implementation of outpatient HF units that provide ambulatory diuretic therapy to well-selected subgroup of patients may result in significant reductions in health care costs while improving the care of patients across a variety of health care settings.
Fiscal pressures to limit readmissions as part of the Center for Medicare and Medicaid Services’ (CMS) Hospital Readmissions Reduction Program have focused attention on improving care transitions and exploring alternatives to hospitalization for treatment of patients with heart failure (HF) decompensation. Because intravenous (IV) loop diuretics are the primary therapy for many patients with decompensated HF and because these patients typically require limited bedside and laboratory monitoring, ambulatory IV loop diuretic treatment has been explored for selected patients with HF as a potentially lower cost alternative to hospitalization. In 1 study, 22% of all observed episodes of decompensated HF were treated with ambulatory IV loop diuretic treatment. Recent studies suggest that this strategy may avert hospitalization without serious adverse effects in hemodynamically stable patients with volume overload (i.e., “warm and wet”). Although the ambulatory approach is intuitively appealing, it remains unclear whether the costs of operating an outpatient HF unit are offset by savings from prevented hospitalizations. Thus, we compared the costs and outcomes of ambulatory diuretic therapy and standard care for patients with decompensated HF from a hospital perspective.
Methods
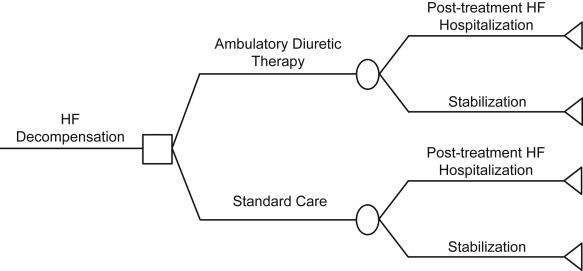
We created a decision analytic model based on experience with this approach at Brigham and Women’s Hospital (BWH) to determine the costs and outcomes of 2 strategies for the treatment of decompensated HF: standard care versus ambulatory diuretic therapy. The decision tree is presented as Figure 1 . The time horizon was 90 days and the hospital perspective was chosen.
The ambulatory diuretic therapy group was composed of consecutive patients treated for decompensated HF at the Ambulatory Cardiac Triage, Intervention, and Education (ACTIVE) unit from May 15, 2013 to May 14, 2014, if they had chronic HF, at least 1 sign and 1 symptom of decompensation (symptoms included dypnea, orthopnea, edema, and signs included rales, peripheral edema, or ascites) and, in the opinion of the referring clinician, a high likelihood of needing hospitalization in the near term. Patients were precluded from treatment in the ACTIVE unit if they had a systolic blood pressure less than 80 mm Hg, serum sodium less than 125 mmol/L, end-stage renal disease or a need for dialysis, significant comorbidities, or required emergent care (e.g., concern for acute coronary syndrome or life-threatening ventricular arrhythmia).
Similarly, the standard care group was based on patients who were treated for decompensated HF as an inpatient at BWH on a specialized HF service. The postdischarge HF care for these patients is provided by the same disease management team that manages the ACTIVE unit. Patients for this cohort were identified with International Classification of Diseases codes and selected using the same inclusion and exclusion criteria as the ambulatory diuretic therapy cohort (see in the previous section). The selected codes are available in the Supplementary Material .
In this model, we defined standard care as hospitalization for IV loop diuretic therapy. The outcomes of standard care were based on the outcomes of patients treated at BWH ( Supplementary Material ). Ambulatory diuretic therapy was defined as treatment in a specialized outpatient HF unit with repeat courses of high-dose IV loop diuretic therapy. For the ambulatory diuretic therapy strategy, the model is based on our previously published experience of BWH’s outpatient HF unit (ACTIVE unit). Based on our past experience of patients treated at the ACTIVE unit (who received a median of 2 treatment sessions per 90 days), the ambulatory diuretic therapy strategy was assumed to include 2 treatment sessions during the 90-day time horizon of the model. The ACTIVE unit facilities include 2 infusion chairs, cardiac telemetry, local medication storage, infusion equipment, and an en-suite bathroom. The ACTIVE unit is open 4 days weekly and is capable of providing 4 treatment sessions per day (2 in the morning session and 2 in the afternoon session) or 16 total per week. High-dose IV loop diuretic therapy (mean dose = 260 mg of IV furosemide equivalent per treatment session) is administered intravenously in a standardized fashion based on the patient’s home diuretic dose. Routine clinic staff include a nurse practitioner, a registered nurse and a clinical pharmacist. A basic metabolic panel is drawn before the diuretic infusion and again within 7 days of the treatment session. Each patient receives telephone follow-up at 7 and 30 days after the treatment session. Additional in-person follow-up occurs as needed.
The model inputs are summarized in Table 1 . Total HF hospitalizations included all hospital admissions for HF during the 90-day time horizon. Post-treatment HF hospitalizations were defined as the subset of total HF hospitalizations that occurred after the index decompensation. Only direct hospital health care costs were included in the analysis, were derived from the reports, and converted to 2014 US dollars using the US consumer price index. Due to the short time horizon, costs and outcomes were not discounted.
| Parameter | Base Case | Range Tested in SA | Source(s) |
|---|---|---|---|
| Probabilities | |||
| Hospitalization during the 90 days following treatment | |||
| Ambulatory diuretic therapy | 0.48 | 0.24-0.72 | Institutional experience |
| Standard Care | 0.20 | 0.10-0.30 | Institutional experience |
| Costs, 2014 USD | |||
| HF hospitalization, $ | 10,146 | 5,073-15,219 | |
| Ambulatory diuretic infusion, $ | 604 | 302-906 | Calculated from individual components |
| Staff salaries, $ | 409 | 205-614 | |
| Laboratory testing, $ | 30 | 15-45 | |
| Diuretic infusion, $ | 25 | 13-38 | |
| Operating costs, $ | 140 | 70-210 | |
The costs for 1 treatment session for ambulatory diuretic therapy were calculated as follows. Staff salaries (1 nurse practitioner, 1 registered nurse, 1 pharmacist, and 1 physician) were calculated from the median publicly reported salary in Boston, Massachusetts. The physician salary cost was calculated under the assumption of 10% time annually dedicated to direct clinic activities, whereas other team members dedicated 100% of time annually to direct clinic activities. The cost of the loop diuretic infusion included the average wholesale prices for 2 100 mg vials of furosemide and 1 250 ml normal saline infusion bag based on observed usage in the ACTIVE unit. The cost of the 2 metabolic panels was based on publically available CMS reimbursement. The operating costs from a study of an HF disease management program were used to estimate the operating costs (e.g., utilities, information technology, administration fees).
The cost of an HF hospital admission was based on CMS reimbursement. The costs of other outpatient care (e.g., routine office visits) were assumed to be equal for both treatment strategies and were not included in the model. The indirect costs, such as patients’ time and travel expenses, were excluded from the analysis. However, we anticipate that the indirect costs would be less for ambulatory diuretic therapy than for standard of care.
We systematically tested the key assumptions of the model and the robustness of the base case in a series of 1- and 2-way sensitivity analyses. One-way sensitivity analysis was conducted for a given parameter by varying that parameter ±50% of its base case value and recalculating the model’s prediction. The following parameters were subject to these 1-way sensitivity analyses: total cost of ambulatory diuretic therapy, probability of posttreatment HF hospitalization after ambulatory diuretic therapy, probability of posttreatment HF hospitalization after standard care and the cost of an HF hospital hospitalization.
For each parameter included in the 1-way sensitivity analysis, we also calculated a threshold value. The threshold value of a parameter is the value of that parameter, which when exceeded, changes the model’s favored strategy. We also modified the base case to determine the effects of increased ambulatory diuretic therapy usage, assuming a total of 4 treatment sessions during the 90-day time horizon instead of 2.
In addition, we conducted a 2-way sensitivity analysis by simultaneously varying the cost of ambulatory diuretic therapy and the probability of posttreatment HF hospitalization after ambulatory diuretic therapy ±50% of their base case values. We then repeated this 2-way analysis 2 additional times: once with a lower probability (0.10) of posttreatment HF hospitalization after standard care and again with a higher probability (0.30) of the same outcome. Finally, we generated a model which varied the risk of a posttreatment HF hospitalization for both strategies proportionally along a continuous scale. This analysis allowed us to estimate the costs and outcomes of each strategy across varying degrees of patient acuity, thus estimating whether ambulatory diuretic therapy would be cost saving in a patient more or less sick than the base case patient.
Because HF is by nature a chronic disease and our available data were limited to 90 days, we developed an exploratory analysis to provide the best possible estimate of the costs of both strategies over a longer time horizon, considering the limitations of extrapolating the data available. For this analysis, we modeled a theoretical scenario with a 180-day time horizon. For the days 0 through 90, the base case parameters were applied. For the days 91-180, the ambulatory diuretic therapy posttreatment hospitalization rate was increased by 50% and the standard care posttreatment hospitalization rate was kept unchanged, to enact a conservative model of long-term outcomes. We do not expect that costs would change meaningfully on a per unit basis over a 180-day period and so the costs remained unchanged.
Results
The characteristics of patients in the model’s ambulatory diuretic therapy (n = 80) and standard care (n = 77) groups are provided in Table 2 .
| Characteristic | Ambulatory Diuretic Therapy (n = 80) | Standard Care (n = 77) | p-value |
|---|---|---|---|
| Age, median (interquartile range) (years) | 70 (62-80) | 75 (64-84) | 0.08 |
| Women | 34 (43%) | 37 (48%) | 0.48 |
| Black | 6 (8%) | 18 (23%) | 0.01 |
| White | 58 (73%) | 47 (61%) | 0.12 |
| Heart failure with preserved ejection fraction | 37 (46%) | 33 (43%) | 0.36 |
| Ejection fraction (heart failure with preserved ejection fraction only), median (interquartile range) | 56% (55%-60%) | 55% (50%-60%) | 0.13 |
| Ejection fraction (heart failure with reduced ejection fraction only), median (interquartile range) | 20% (20%-30%) | 26% (20%-35%) | 0.11 |
| New York Heart Association Class | |||
| I | 1/70 (1%) | 0/30 (0%) | 0.54 |
| II | 11/70 (16%) | 9/30 (30%) | 0.05 |
| II | 41/70 (59%) | 18/30 (60%) | 0.41 |
| IV | 17/70 (24%) | 3/30 (10%) | 0.17 |
| Heart failure hospitalization within previous 1 year | 46 (58%) | 29 (38%) | 0.01 |
| Comorbidities | |||
| Atrial fibrillation | 30 (38%) | 28 (36%) | 0.88 |
| Chronic kidney disease | 25 (31%) | 20 (26%) | 0.47 |
| Coronary artery disease | 45 (56%) | 35 (46%) | 0.18 |
| Diabetes mellitus | 37 (46%) | 35 (46%) | 0.92 |
| Hypertension | 57 (71%) | 50 (65%) | 0.40 |
| Home medications | |||
| Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker | 40 (50%) | 44 (57.1%) | 0.37 |
| Aldosterone antagonist | 33 (41%) | 19 (25%) | 0.03 |
| Beta-blocker | 61 (76%) | 54 (70%) | 0.39 |
| Digoxin | 14 (18%) | 14 (18%) | 0.91 |
| Isosorbide | 11 (14%) | 15 (20%) | 0.33 |
| Hydralazine | 2 (3%) | 4 (5%) | 0.38 |
| Loop diuretic | 68 (85%) | 63 (82%) | 0.59 |
| Presentation | |||
| Heart rate, median (interquartile range) (beats per minute) | 74 (65-82) | 78 (64-89) | 0.40 |
| Systolic blood pressure, median (interquartile range) (mm Hg) | 120 (106-132) | 130 (116-148) | 0.003 |
| Serum sodium, median (interquartile range) (mmol/L) | 137 (135-140) | 138 (136-140) | 0.22 |
| Serum creatinine, median (interquartile range) (mg/dL) | 1.45 (1.15-1.88) | 1.15 (0.96-1.51) | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


