South Asians in the Western world have a high prevalence of diabetes mellitus (DM) and an increased risk of coronary artery disease (CAD) and mortality compared with Caucasians. CAD in asymptomatic South Asian patients with type 2 DM has not been investigated. The aim of this observational cohort study was to investigate CAD in asymptomatic South Asian patients with type 2 DM and to compare with matched Caucasian patients. A total of 120 asymptomatic South Asian patients with type 2 DM and matched Caucasian patients (mean age 52 years, 55% men) were derived from an ongoing registry of cardiovascular risk stratification in asymptomatic patients with DM. Cardiovascular risk assessment included multidetector row coronary computed tomography angiography. CAD was assessed as the coronary artery calcium score and classified into no signs of atherosclerosis or minor wall irregularities <30%, nonsignificant CAD 30% to 50%, or significant CAD ≥50% stenosis. On a patient base, CAD was scored according to the severity and number of vessels and segments with significant CAD. Subsequently, CAD was assessed per coronary artery and per segment. Compared with Caucasian patients, South Asian patients had a significantly higher coronary artery calcium score and higher prevalence of significant CAD (41% vs 28%, respectively, p = 0.008), involving more coronary vessels and segments. Significant CAD was especially more frequent in the left anterior descending coronary artery. In conclusion, asymptomatic South Asian patients with type 2 DM have a higher prevalence and extent of CAD compared with matched Caucasian patients.
Several studies have demonstrated that South Asian patients in the Western world have more severe coronary artery disease (CAD) and higher cardiovascular mortality compared with Caucasian patients. However, differences in CAD between asymptomatic South Asian and asymptomatic Caucasian patients with type 2 diabetes mellitus (DM) have not been investigated. Multidetector row coronary computed tomography angiography (coronary CTA) is a well-validated method for the noninvasive assessment of CAD and allows assessment of the CAD and plaque composition. Therefore, the aim of the present study was to assess CAD in asymptomatic South Asian patients with type 2 DM with coronary CTA and to compare with matched asymptomatic Caucasian patients with type 2 DM.
Methods
South Asian patients with type 2 DM were enrolled from an ongoing registry of cardiovascular risk stratification in asymptomatic patients with DM in the Leiden University Medical Center, the Netherlands. These South Asians patients are “Surinamese South Asian immigrants” whose ancestors were recruited from North India from 1873 until 1916 to work on plantations in Suriname. In 1975 around the independence of Suriname, a large group of Surinamese South Asians settled in the Hague. Cardiovascular risk stratification contained a structured clinical history, physical examination, blood and urine laboratory testing, and coronary CTA for the evaluation of CAD. South Asian ethnicity was established in the anamnesis.
South Asian patients were individually matched with asymptomatic Caucasian patients with type 2 DM, based on age, gender, DM duration, and body mass index (BMI). Because South Asian patients have increased abdominal fat storage and higher insulin resistance at similar BMI levels, a lower obesity cutoff BMI is recommended by the World Health Organization. In line with this, South Asian patients were matched to Caucasian patients with a higher BMI.
Patients were diagnosed with type 2 DM in the absence of demonstrable auto-antibodies to islet cells, insulin, and glutamic acid decarboxylase or low levels of plasma C-peptide levels, according to the American Diabetes Association criteria. Inclusion criteria were type 2 DM, asymptomatic status as confirmed by the Rose questionnaire on chest pain, no previous myocardial infarction, coronary revascularization or cardiac surgery, and a coronary CTA of diagnostic image quality for the assessment of CAD.
Clinical and demographic data were prospectively collected in the departmental cardiology information system (EPD-Vision version 8.3.3.6; Leiden, the Netherlands) and were retrospectively analyzed. The Institutional Review Board of the Leiden University Medical Center approved the retrospective evaluation of clinically collected data and waived the need for written informed consent.
Coronary CTA was performed on a 64-detector row CT scanner (Aquilion 64; Toshiba Medical Systems, Otawara, Japan) or a 320-detector row CT scanner (Aquilion ONE; Toshiba Medical Systems, Otawara, Japan). Scan parameters of these CT scanners have been previously described.
One hour before the scan, heart rate and blood pressure were measured to administer β blockers (25 to 100 mg metoprolol, orally) in patients with a heart rate ≥65 beats/min, unless contraindicated. In addition, immediately before the coronary CTA scan, nitroglycerin 0.4 mg was administered sublingual.
The scan protocol commenced with a noncontrast scan of the heart with slice thickness of 3.0 mm for the coronary artery calcium (CAC) score. Subsequently, coronary CTA was started with the injection of nonionic contrast media (Iomeron 400; Bracco, Milan, Italy) in the antecubital vein in a bolus of 60 to 110 ml with a flow rate of 5 to 6 ml/s (adjusted to patient’s weight), followed by a saline flush. Coronary CTA image acquisition was triggered using automated peak enhancement detection with the region of interest in the left ventricle. Scanning was completed during a single breath hold of approximately 10 seconds. Data were retrospectively (64-detector row scanner) or prospectively (320-detector row scanner) gated by recording the electrocardiogram during the scan. An initial data set was automatically reconstructed at 75% phase of the R-R interval. In the case of limited image quality or motion artifacts, additional data sets of different phases in the R-R interval were reconstructed.
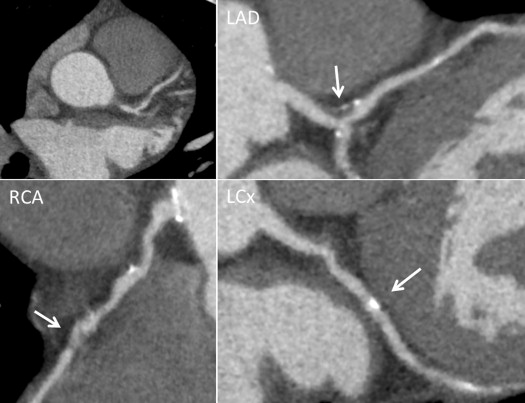
Coronary CTA scans were postprocessed and evaluated on a remote work station using dedicated coronary CTA analysis software (Vitrea 2 or Vitrea FX 1.0; Vital Images, Minnetonka, Minnesota). First, the Agatston CAC score was measured on the noncontrast calcium scan. Thereafter, the coronary CTA data set with the best image quality was selected for the evaluation of the coronary arteries. Coronary CTA scans were analyzed by 2 experienced observers in consensus, blinded to patient’s clinical and demographic characteristics. The coronary artery system was divided according to the modified American Heart Association classification into a 17-segment model. All segments were evaluated for the presence of atherosclerotic plaque, defined as a structure >1 mm 2 within and/or adjacent to the coronary artery lumen that could clearly be distinguished from the coronary artery lumen and surrounding tissue. For each atherosclerotic plaque, the severity of luminal stenosis was visually determined from the axial images and curved multiplanar reconstructions in at least 2 orthogonal planes (see Figure 1 ). Per segment luminal stenosis was graded based on the most severe stenosis as follows: (1) no signs of atherosclerosis or minor wall irregularities <30% stenosis, (2) nonsignificant CAD 30% to 50% stenosis, or (3) significant CAD ≥50% stenosis. In addition, the predominant atherosclerotic plaque composition was scored as noncalcified plaque (consisting of only low-density plaque), calcified plaque (consisting of only high-density plaque), or mixed plaque (consisting of both low- and high-density plaques). Local noninterpretable segments were excluded from further analysis.
Patients were stratified according to the segment with the most severe stenosis grade. Significant narrowing was assessed per coronary artery and significant 1-, 2-, and 3-vessel CAD. In addition, the Gensini score was calculated. Subsequently, the location of CAD narrowing in proximal and distal coronary segments was determined. Finally, the presence of any CAD (≥30% stenosis) was assessed per coronary artery and per segment.
Continuous data were checked for normal distribution with the Kolmogorov-Smirnov test. Normal distributed continuous data are presented as mean ± SD and nonnormally distributed continuous data as median (twenty-fifth and seventy-fifth percentiles). Categorical data are presented as frequencies and percentages. Comparisons of continuous data between asymptomatic South Asian and Caucasian patients with type 2 DM were performed with the independent Student t test, 1-way analysis of variance or Mann-Whitney U test, as appropriate. Categorical data were compared with the chi-square test. A p value of <0.05 was considered statistically significant. All statistical analyses were performed with SPSS (version 20.0; SPSS Inc., Chicago, Illinois).
Results
A total of 120 asymptomatic South Asian patients with type 2 DM were included and individually matched with asymptomatic Caucasian patients with type 2 DM. The baseline clinical and demographic patient characteristics are listed in Table 1 . The overall mean age was 53 ± 10 years, 55% were men, and mean DM duration was 11 ± 8 years. Because South Asian patients were matched to Caucasian patients with a higher BMI, they had a significantly lower BMI and waist circumference. Furthermore, South Asian patients had a significantly higher prevalence of peripheral artery disease (21% vs 10%, respectively, p = 0.04). Other baseline clinical risk factors were similar.
| Variable | Overall (n = 240) | South Asian (n = 120) | Caucasian (n = 120) | p Value |
|---|---|---|---|---|
| Age (yrs) | 53 ± 10 | 52 ± 10 | 53 ± 9 | 0.4 |
| Men | 132 (55) | 66 (55) | 66 (55) | 1 |
| DM duration (yrs) | 11 ± 8 | 12 ± 8 | 11 ± 8 | 0.5 |
| BMI (kg/m 2 ) | 29 ± 6 | 28 ± 5 | 30 ± 6 | <0.01 |
| Waist circumference (cm) | 101 ± 16 | 98 ± 16 | 104 ± 14 | <0.01 |
| Hemoglobin A1c (%) | 7.9 ± 1.6 | 7.8 ± 1.6 | 7.9 ± 1.6 | 0.6 |
| Insulin treatment | 112 (47) | 43 (36) | 69 (58) | <0.01 |
| DM complication ∗ | 99 (41) | 53 (44) | 46 (38) | 0.4 |
| Hypertension † | 161 (67) | 81 (68) | 80 (67) | 1.0 |
| Systolic blood pressure (mm Hg) | 136 ± 18 | 134 ± 17 | 138 ± 18 | 0.1 |
| Diastolic blood pressure (mm Hg) | 83 ± 10 | 83 ± 11 | 84 ± 10 | 0.5 |
| Antihypertensive drug use ‡ | 137 (57) | 70 (58) | 67 (56) | 0.7 |
| Hypercholesterolemia § | 185 (77) | 91 (76) | 94 (78) | 0.8 |
| Total cholesterol (mmol/L) | 4.6 ± 1.1 | 4.4 ± 1.1 | 4.7 ± 1.1 | 0.09 |
| Total cholesterol (mg/dl) | 178 ± 42 | 170 ± 42 | 181 ± 42 | 0.09 |
| Statin use | 161 (67) | 87 (73) | 74 (62) | 0.07 |
| Smoker | 60 (25) | 32 (27) | 28 (23) | 0.6 |
| Stroke or transient ischemic attack | 12 (5) | 7 (6) | 5 (4) | 0.5 |
| Peripheral artery disease | 31 (13) | 21 (18) | 10 (8) | 0.04 |
| Angiotensin-converting enzyme inhibitor | 61 (25) | 31 (26) | 30 (25) | 0.9 |
| Angiotensin II receptor antagonist | 66 (28) | 29 (24) | 37 (31) | 0.2 |
| β blocker | 26 (11) | 13 (11) | 13 (11) | 1 |
| Calcium antagonist | 25 (10) | 12 (10) | 13 (11) | 0.8 |
| Aspirin | 46 (19) | 21 (18) | 25 (21) | 0.5 |
| Plasma creatinine (μmol/L) | 78 ± 24 | 77 ± 29 | 78 ± 18 | 0.7 |
| Glomerular filtration rate (ml/min/1.73 m 2 ) ¶ | 93 ± 28 | 96 ± 33 | 89 ± 21 | 0.04 |
∗ DM complication included retinopathy, nephropathy, neuropathy, and peripheral vascular disease as derived from the structured clinical history.
† Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic pressure ≥90 mm Hg, or use of antihypertensive medication.
‡ Antihypertensive drug use included angiotensin-converting enzyme inhibitors, angiotensin II receptor antagonist, β blockers, and calcium antagonists.
§ Hypercholesterolemia was defined as serum total cholesterol ≥5 mmol/L or use of lipid-lowering therapy.
¶ Glomerular filtration rate was calculated with the MDRD study equation. 29
Coronary CTA results and p values for comparison are listed in Table 2 . South Asian patients had a significantly higher presence and extent of CAC. Moreover, the presence of significant CAD was significantly higher: 49 (41%) versus 33 (28%) patients, p = 0.008. The presence of significant 1-, 2-, and 3-vessel CAD was significantly higher, especially the left anterior descending (LAD) coronary artery was more frequently affected. Also, the Gensini score was significantly higher. There was no significant difference in coronary plaque composition.
| Variable | Overall (n = 240) | South Asian (n = 120) | Caucasian (n = 120) | p Value |
|---|---|---|---|---|
| Dominant right coronary | 183 (76) | 90 (75) | 93 (78) | 0.6 |
| CAC (CS ≥1) | 143 (60) | 79 (66) | 64 (53) | 0.03 |
| Total Agatston calcium artery score | 16 (0–149) | 26 (0–205) | 3 (0–99) | 0.03 |
| Normal or wall irregularities <30% | 82 (34) | 32 (27) | 50 (42) | <0.01 |
| Nonsignificant CAD 30%–50% | 76 (32) | 39 (33) | 37 (31) | |
| Significant CAD ≥50% | 82 (34) | 49 (41) | 33 (28) | |
| Gensini score | 6 ± 8 | 8 ± 9 | 5 ± 7 | <0.01 |
| No. of coronary arteries narrowed | 0.03 | |||
| 1 | 44 (18) | 26 (22) | 18 (15) | |
| 2 | 24 (10) | 13 (11) | 11 (9) | |
| 3 | 14 (6) | 10 (8) | 4 (3) | |
| Coronary artery narrowed | ||||
| LM | 3 (1) | 3 (3) | 2 (2) | 0.08 |
| LAD | 68 (28) | 42 (35) | 26 (22) | 0.02 |
| LCx | 30 (13) | 18 (15) | 12 (10) | 0.2 |
| Right | 33 (14) | 19 (16) | 14 (12) | 0.3 |
| Location of CAD narrowing | ||||
| Proximal ≥30% ∗ | 128 (53) | 76 (63) | 52 (43) | <0.01 |
| Distal ≥30% † | 133 (55) | 71 (59) | 62 (52) | 0.2 |
| Proximal ≥50% | 47 (20) | 29 (24) | 18 (15) | 0.07 |
| Distal ≥50% | 68 (28) | 43 (36) | 25 (21) | 0.01 |
| Number of segments narrowed | ||||
| ≥30% | 2.7 ± 2.9 | 3.1 ± 3.0 | 2.3 ± 2.8 | 0.03 |
| 30%–50% | 1.9 ± 2.0 | 2.1 ± 2.1 | 1.7 ± 2.0 | 0.1 |
| ≥50% | 0.8 ± 1.4 | 1.0 ± 1.6 | 0.6 ± 1.2 | 0.03 |
| Coronary plaque composition | ||||
| Noncalcified | 1.4 ± 1.5 | 1.4 ± 1.8 | 1.5 ± 1.2 | 0.5 |
| Mixed | 1.7 ± 1.9 | 1.8 ± 1.8 | 1.7 ± 1.9 | 0.7 |
| Calcified | 1.0 ± 1.6 | 1.2 ± 1.7 | 0.8 ± 1.5 | 0.2 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


