The present project investigated whether cardiac magnetic resonance (CMR) of aortic arch anomalies can be performed successfully in infants <6 months of age without the use of cardiac anesthesia or deep sedation. We performed a retrospective review of infants ≤6 months old from 2005 to 2009 who underwent either CMR or computed tomography angiography to investigate aortic arch abnormalities. The CMR procedure used a “feed and swaddle” protocol without deep sedation or cardiac anesthesia. Of the 52 infants referred for CMR, 24 underwent the feed and swaddle protocol (aged 2.6 ± 1.4 months). One patient awoke during the study, and examination of the remaining 23 yielded a definitive diagnosis (success rate 96%). The scanning time was 6.2 ± 3.1 minutes, with the large airways evaluation accounting for the time. Single-shot axial steady-state free precession, in which the definitive diagnosis was made, accounted for 0.59 ± 0.3 minutes. Fifteen infants were diagnosed with a vascular ring. Of the 8 infants who underwent surgery, the diagnostic accuracy was 100%. During the same period, 19 patients, who had undergone computed tomography angiography (aged 1.67 ± 1.20 months), were referred for aortic arch evaluation. Of these 19 patients, 6 (32%) underwent sedation or anesthesia. The imaging time was 0.08 ± 0.06 minutes, significantly different from the CMR times (p <0.01). However, the overall room times (31.3 ± 22.3 and 35.8 ± 3.86 minutes, respectively) were not different between the CMR and angiographic groups. The radiation dose was 1.41 ± 1.03 mSv. In conclusion, CMR evaluation of aortic arch anomalies in children <6 months old can be successfully completed quickly using a feed and swaddle approach with high diagnostic accuracy. This protocol avoids the risks of sedation, as well as the radiation associated with computed tomography angiography.
Cardiac magnetic resonance (CMR) has become increasingly important and integrated into the care of many patients with congenital heart disease. It is the reference standard in many areas (e.g., vascular rings or ventricular volumes and mass ). However, the patient needs to remain motionless during the scan. This is an important issue with infants who typically require cardiac anesthesia (CA) or deep sedation (DS). CMR of infants or neonates without the use of CA or DS would be beneficial. Computed tomographic angiography (CTA) can acquire anatomic and limited functional data within a short period without the need for pharmacologic intervention. Advances in hardware and software have enabled CMR to obtain anatomic and functional information in selected neonates and infants with certain congenital cardiovascular lesions within minutes, allowing CMR to compete favorably with CTA for efficiency. Using CMR can avoid the ionizing radiation and iodinated contrast required with CTA, as well as providing the additional capability of obtaining high-resolution functional data. The present retrospective, single-center study investigated an approach for performing CMR in neonates and infants without the use of CA or DS using a feed and swaddle technique (F&S), in which the neonates and infants are fed and then swaddled with a blanket to induce sleep. Patients referred to CMR to assess for vascular rings and aortic arch anomalies were chosen because these diagnostic categories are quickly and easily imaged. Because DS or CA was not administered, the expected adverse event rate should be near 0. A comparison with the CTA experience in similar infants at our institution within the same period was also performed. If high-quality, diagnostic CMR images can be obtained within a short period (≤5 minutes), this method would decrease the risk of CMR to near 0 and make aortic arch CMR an even more attractive alternative to CTA.
Methods
A search of the CMR and computed tomographic angiographic databases at our institution from January 1, 2005 to March 18, 2009 was performed for all patients who had been referred for CMR or CTA for vascular ring or aortic arch abnormality evaluation and who were ≤6 months old. The choice of CMR or CTA for evaluation was by individual physician practice. The type of approach to imaging (F&S, DS, or CA) was recorded. The DS method in children undergoing magnetic resonance has been widely published. Our institution uses midazolam, ketamine, or fentanyl. The patients also had to be receiving enteral nutrition. CMR studies were performed using a Siemens 1.5 Tesla Sonata or Avanto magnetic resonance imaging system and analyzed using Siemens’ analysis package on a Leonardo workstation (Siemens Medical Solutions, Malvern, Pennsylvania). The patients undergoing CTA were screened to determine if they would undergo CA or DS. The institutional review board at the hospital granted approval and a waiver of informed consent for the present study.
The patients who underwent the F&S protocol had their imaging and clinical data examined to determine whether their CMR study was complete. The 2 criteria for a successful study were (1) the study was completed without the use of CA or DS; and (2) the quality of the images allowed a definitive diagnosis.
For the F&S approach, the families with neonates and infants scheduled to undergo CMR with the F&S approach were instructed not to feed their infants for 2 to 3 hours before the examination. On arrival and after evaluation of history and physical examination by the nursing staff, an intravenous line was inserted, and electrocardiographic leads were placed. An infant hat was placed over the child’s ears to decrease the perception of noise. In addition, ear plugs were placed. The patient was then moved to the sedation room adjacent to the scanner (so as not to interfere with on-going imaging) with the lights dimmed and the infant in the mother’s or nurse’s arms, swaddled with a blanket, and fed. The blanket swaddling was also over the ears to further decrease noise perception. Rocking and other forms of calming actions (e.g., singing to the infant) were performed as needed. Once the child had fallen asleep, the infant was immediately transferred to the CMR scanner, placed in the supine position within a head coil with supporting cushions and moved to the isocenter. The knee coil was not used because it was too small for any infant.
CMR imaging was performed using a 1.5 Tesla Siemens Avanto whole body magnetic resonance imaging system (Siemens Medical Solutions) using the phased array head coil. Each infant underwent the following protocol with the following techniques (note: nearly the entire examination was a vascular study, and no sequences such as cine or phase-contrast mapping were performed):
After localizers were performed to identify the heart and vascular structures in the chest, a stack of electrocardiographic-gated, static, steady-state free precession contiguous end-diastolic axial images spanning the entire thorax from the thoracic inlet to the diaphragm were performed using multiple averages. This was initially done using a segmented approach with the typical parameters listed in Table 1 and taking approximately 2.5 to 3 minutes. As our experience increased, this was changed to the “single shot” form (all phase encoding steps performed in 1 RR interval) with 1 average for time considerations; this took just slightly >1/2 minute. Changes to the parameters are also listed in Table 1 . Parallel imaging was used with an acceleration factor of 2 obtaining 24 reference lines. This portion of the examination made the definitive diagnosis and therefore occurred in just slightly >1/2 minute. Some patients had both “single shot” and “averaged” scan.
Table 1
Magnetic resonance imaging parameters
Parameter
Setting
Multiple averages
Single shot
Repetition time (ms)
180
300
Echo time (ms)
1.4
1.4
Field of view (mm)
160–200
160–200
Slices (n)
45–50
40
Thickness (mm)
3
3
Distance factor (% overlap)
20
0
Matrix
128 × 128
128 × 128
Excitations (n)
3
1
Rectangular field of view (% total field)
75
75
Flip angle (°)
75–90
75–90
Acquisition time (ms)
400–500
400–500
Segments (n)
29
96
Bandwidth (Herz/pixel)
1,220
1,220
Dark blood imaging
Gadolinium imaging
Repetition time (ms)
500
3.15
Echo time (ms)
63
1.15
Field of view (mm)
160–200
160–200
Slices (n)
3
45–60
Thickness (mm)
3
1.3
Distance factor (% overlap)
0
NA
Matrix
128 × 128
192 × 192
Excitations (n)
3
1
Rectangular field of view (% total field)
75%
75%
Flip angle (°)
75–90
25
Acquisition time (ms)
400–500
NA
Segments (n)
29
NA
Bandwidth (Herz/pixel)
235
410
Electrocardiographic-gated, double-inversion dark blood imaging was used to delineate the large airways in 2 orthogonal views (off-axis sagittal and coronal) and was prescribed from the stack of steady-state free precession images. The parameters are listed in Table 1 , and the scans took approximately 2.5 to 3 minutes to perform. Saturation bands were laid down parallel to the imaging plane and on the chest wall to decrease the respiratory artifact. Parallel imaging was used with 32 reference lines. This constituted the longest part of the CMR examination.
A static 3-dimensional T 1 -weighted contrast-enhanced magnetic resonance angiographic sequence was performed using a bolus technique in the left anterior oblique sagittal plane. The bolus techniques used a time-resolved, T 1 -weighted sequence to follow the contrast agent through the cardiovascular system after peripheral injection. Once it reached the target (in this particular case, the aorta), the static 3-dimensional gadolinium sequence was begun, with 0.4 ml/kg of Magnevist (Berlex Laboratories, Montville, New Jersey) injected intravenously by power injector at 2 ml/s followed by 10 ml of saline. The parameters are listed in Table 1 , and the sequence took approximately 30 seconds. In patients with high heart rates, the imaging scan was begun when the bolus was seen in the pulmonary arteries, because the flow tends to quickly traverse the heart, and the aortic imaging could have been missed otherwise.
CTA imaging was performed using a Siemens Somatom Sensation, 64-slice, scanner. After obtaining a digital scout chest radiograph and intravenously injecting 2 ml/kg of Omnipaque 350 (Novaplus, Irving, Texas) with a power injector, a volumetric helical CTA acquisition at 80 kVp and effective mAs of 80 was obtained from the diaphragm to the thoracic inlet as the contrast reached the target. The data were used to evaluate the axial source images and for multiplanar reconstructions at an independent workstation.
The CMR studies were reviewed to determine whether the study was complete and which techniques were performed. For successful CMR using F&S, a study must have been completed without the use of CA or DS and the quality of the images must have allowed a correct diagnosis. The studies were read again by one of the authors (M. A. F.), who had no knowledge of the original reading. Because the goal of the examination is to obtain a diagnosis and not solely to create esthetically pleasing images, the grading of imaging quality was not performed for either CTA or CMR. The only criteria was that the image quality was great enough to obtain the diagnostic information. For both CMR and CTA studies, the recorded times were defined as follows: The room time was defined as the interval from the patient entering the CTA or CMR scanner until the time the patient left the scanner room. The imaging time was defined as the interval taken to acquire the images. For the CMR studies, 2 groups of patients were found: those who had ultrafast “single-shot” steady-state free precession imaging alone and those who also had steady-state free precession imaging with 3 excitations. Because the diagnoses can be obtained simply from the “single shot” images alone, the 2 groups were analyzed together, as well as separately. The imaging time was calculated from the digital time stamps on the images. The study time was defined as the period from beginning the localizer until the end of the last scan. The time was calculated using the time stamps on the first and last images of the study.
Descriptive statistics were used to describe the population and included the mean and SD. The unpaired Student t test was used to determine differences between the CMR and CTA scan room times.
Results
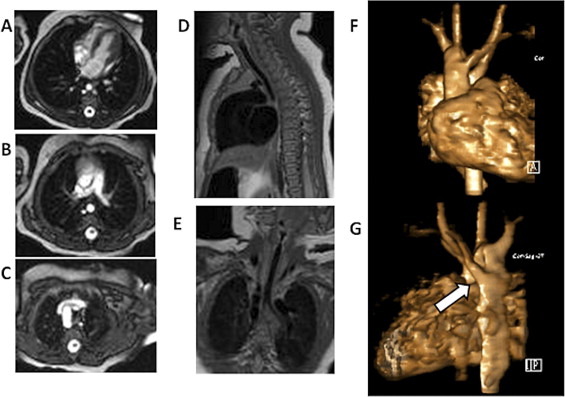
A total of 52 patients (age 2.93 ± 1.87 months, range 0.10 to 6.13) were referred for CMR for evaluation of the possibility of a vascular ring. Of the 52 patients, 24 (46%) underwent CMR using the F&S protocol (age 2.6 ± 1.4 months). The reasons for not using F&S included tenuous respiratory status, more extensive imaging (e.g., evaluation for tetralogy of Fallot), and parental preference for the patient to undergo DS or CA (to ensure successful imaging). One patient who had difficulty going to sleep awoke after the localizer images and needed to return to undergo CMR under DS. All other subjects completed the CMR using the F&S protocol and had diagnostic quality images, for a 96% success rate. All diagnostic information was contained in the static steady-state free precession “single shot” imaging or the static steady-state free precession “multiple average” imaging. The other imaging sequences simply enhanced the information already obtained. No change occurred in the diagnosis from the repeat evaluation of the initial reading. No adverse events were noted. Figure 1 shows the images obtained from a typical patient.